Gastric hormones handout text
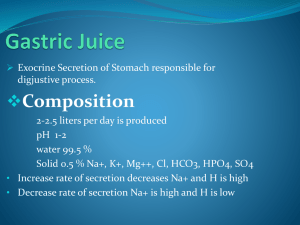
advertisement

ENDOCRINOLOGY 7 GASTRO-INTESTINAL HORMONES Coordination of G-I tract Function Functions: • G-I hormones, with the enteric and autonomic nervous systems, integrate and coordinate the mechanisms which move, digest and absorb the various meals that are ingested, at the same time preserving homeostasis of the milieu interne. • They control G-I tract exocrine and endocrine secretion, motility, growth, & blood flow. • They also affect appetite and feeding behaviour Routes: • Hormones released from gut endocrine cells act via endocrine and paracrine routes (and possibly also via the gut lumen). • Peptides are also released from nerves of the enteric nervous system. • Because many actions are local and not via the blood stream it is difficult to determine the physiologically active concentration of hormone. Antibodies which neutralise the action of gut hormones have therefore been used to elucidate their physiology. Gut (entero-) endocrine cells: • Part of G-I tract epithelium; derived from endoderm; positioned in crypts; • Most cells have sensory microvilli on apex open to gut lumen; • Hormone is secreted basally; • Distribution varies fetus/adult (e.g. in fetus most gastrin is in pancreas). Gut hormones: • Evolution has produced families: gastrin/CCK; secretin/VIP/GIP/glucagon; (many have homologues in the brain); • Most are peptides produced from larger precursors, so different molecular forms of the hormones are found; • An endocrine role is established for most, others are candidate hormones;Many show Amine Precursor Uptake & Decarboxylation (APUD cells; hence clinically tumours are sometimes called “APUDomas”). GASTRIN – stimulates gastric acid & pepsinogen secretion and motility • Distribution: G cells of gastric antrum crypts; some duodenal. • Synthesis: preprogastrin → gastrin G34 → G17 → G13 + G4 (pentagastrin)(sulphati on) Release of gastrin after meal 1 • Plasma: fasting 10-50pmol/l; increased by 40 pmol/l after meal; G17 t0.5=5 min; (G34 t0.5=40 min has only 20% potency of G17) • Mechanism of action: via Gαq, Ca, PKC • Release: Stimulated by: protein digestion products (esp tryptophan, phenylalanine)(also beer, wine, coffee) vagus, via acetylcholine, gastrin-releasing peptide distension of stomach hypercalcaemia (cause? ) Inhibited by: stomach pH<2.5; alkali short-term has little effect, long-term causes hyperplasia; somatostatin (local negative feedback) Trophic effects of gastrin • Actions: stimulates gastric acid secretion (direct & indirect via histamine H2); stimulates parietal cell growth stimulates pepsinogen secretion from chief cells; (also water & electrolyte secretion in liver, pancreas, intestine) stimulates antral motility, mucosal blood flow trophic to body of stomach; ? to other parts (high levels: stimulate calcitonin, food intake, insulin secretion, pancreatic enzyme secretion, antagonise secretin) • Pathology: gastrinoma (usually in pancreas) causes repeated peptic ulceration due to high acid and pepsin secretion NB Effect on acid secretion synergises with that of vagal acetylcholine (M3 receptors Gαq, Ca, PKC) Effects of histamine and H2 antagonists HISTAMINE – stimulates gastric acid secretion • Distribution: Enterochromaffin-like (ECL) cells of stomach wall. • Synthesis: from histidine by histidine decarboxylase • Release: Stimulated by vagus (ACh), gastrin • Actions: Stimulates gastric acid (HCl) secretion via H2 receptors (Gαs, cAMP, PKA) • Pharmacology: H2 receptor antagonists used to treat peptic ulceration (now largely superceded by proton (H-K) pump inhibitors) 2 GASTRIN-RELEASING PEPTIDE peptide; in nerves of GI tract (vagus)(also lung mucosal neuroendocrine cells); releases gastrin SECRETIN – neutralises stomach acid • Distribution: S cells, duodenum to distal ileum; in neck of crypts • Synthesis: small, very basic peptide. Plasma: 20pmol/l after meals; t0.5=3 min • Release: stimulated by acid in proximal duodenal lumen (pH<4.5); somatostatin inhibited by • Actions: via cAMP - stimulates pancreatic ducts to secrete HCO3- & water; (cAMP stimulates Cl- secretion via CFTR, HCO3- is then exchanged for Cl-) this washes pancreatic enzymes into the gut. - stimulates liver secretion of HCO3- & water into bile (potentiates CCK) NB synergises with vagal acetylcholine (M3 receptors Gαq, Ca, PKC) CHOLECYSTOKININ (CCK; aka PANCREOZYMIN) - secretion of pancreatic enzymes and bile into duodenum • Distribution: I cells in the duodenum and jejunum • Forms: CCK33, CCK58, CCK39; CCK8 (in brain); shares terminal pentapeptide with gastrin • Release: stimulated by protein and fat digestion products in duodenum 3 • Actions: (via Gαq, Ca, PKC) - stimulates secretion of pancreatic enzymes and potentiates action of secretin - stimulates contraction of gall bladder (inhibits gastric emptying; increases small bowel transit) (high levels potentiate secretion of calcitonin) - causes satiety (feeling one has had enough to eat) via vagal nerve terminals and in the CNS NB synergises with vagal ACh (M3 receptors Gαq, Ca, PKC) THE ‘INCRETIN’ EFFECT - glucose stimulates insulin more powerfully if than intravenously GLP-1[7-37] Glucagon-like peptide (a type of gut glucagon) • Distribution: L cells in small bowel (also produce oxyntomodulin – see below) • Release: stimulated by meals: especially oral (not intravenous) fat; also by GIP • Actions: powerfully potentiates glucose-stimulated insulin release effect); alone, does not stimulate insulin GIP (Glucose-dependent Insulinotropic Peptide) (Originally named for its gastric inhibitory peptide action, which is weak) • Distribution: K cells of duodenum > proximal jejunum > distal jejunum • Structure: 43aa peptide of secretin/glucagon family given orally carbohydrate and ("incretin" • Release: stimulated by oral (not intravenous) glucose, fat and protein; insulin may inhibit release • Actions: potentiates glucose-stimulated insulin release ("incretin" effect); alone, does not stimulate insulin LOCAL INHIBITION/NEGATIVE FEEDBACK SOMATOSTATIN • Distribution: D cells from gastric antrum through to colon • Structure: small (14aa) peptide (28aa in brain); acts via inhibition of cAMP production • Release: stimulated by meals (amino acids, glucose, fatty acids), gastrin, • Actions: suppresses secretion of most GI hormones and their effects paracrine negative feedback retards absorption of glucose and so protects against hyperglycaemia (in liver) secretin (acid etc); post-prandial • Pathology: Tumour - somatostatinoma. Effects: steatorrhoea (fatty faeces; lack of CCK); hypoacid (lack of gastrin); bowel stasis (lack of motilin). diabetes mellitus (lack of insulin); • Pharmacology: somatostatin analogue (eg Octreotide; 8aa) used to treat gut endocrine tumours; also to treat acromegaly. 4 PANCREATIC POLYPEPTIDE • Distribution: Islets in uncinate process of (ventral) pancreas • Structure: small peptide related to neuropeptide Y; Y4 receptor, inhibition of cAMP • Release: stimulated by vagus, nutrients (not glucose) gastric distension, inhibited by hyperglycaemia, somatostatin • Actions: inhibits postprandial pancreatic enzyme secretion reduces gastric and intestinal motility reduces appetite centrally • Pathology: secreted by some GI tumours, used as tumour marker. Other major gut hormones Vasoactive Intestinal Polypeptide - VIP • Distribution: in enteric neurons (also brain; and in pelvic parasympathetic nerves where, with NO, it is causes penile erection) • Structure: small peptide; secretin/glucagon family; acts via cAMP (c.f. cholera) • Release: ?oesophageal distension; plasma levels don't rise after meal • Actions: relaxes cardiac sphincter and stomach, anal sphincter; vasodilator Pathology: Tumour - VIPoma (Verner-Morrison syndrome): watery diarrhoea; hypokalaemia; achlorhydria Motilin • Distribution: gut endocrine cells from gastric antrum to colon • Structure: small peptide • Actions: increases the motility of the bowel; induces migrating myoelectric complexes at antro-duodenal pacemaker Neurotensin • Distribution: N cells of distal small intestine (also extensively in CNS neurons) • Structure: small peptide • Stimuli: intraluminal fat • Actions: physiology unknown: reported to pancreatic secretion; gastric/ small bowel motility; colonic motility trophic effects on gut mucosa Gut glucagon (enteroglucagon, glicentin) • Distribution: Gastric A cells; ileal and colonic L cells • Structure: extended forms of glucagon-like molecules • Actions: stimulates gastric/intestinal motility; intestinal absorption sugars; has systemic glucagon-like effects trophic to small bowel (compensatory hypertrophy) 5 Pathology: Multiple Endocrine Neoplasia (MEN) Tumours are usually multiple; both types are genetically determined) MEN 1: tumours of pancreas (gastrinoma, insulinoma, VIPoma), pituitary and MEN 2: tumours of thyroid C cells, adrenal chromaffin cells and parathyroids GUT HORMONES IN THE CONTROL OF APPETITE AND FEEDING In addition to the feedback effects from taste, stomach distension etc by the sensory nerves of the alimentary tract, it is now clear that gastrointestinal hormones affect feeding by an action on the hypothalamus and brain stem (via the blood). The same is true for insulin, which suppresses appetite. This is dealt with more fully in year 2 integrative physiology CCK – inhibits feeding (see above) PANCREATIC POLYPEPTIDE – inhibits feeding (see above) GHRELIN – stimulates feeding Distribution: produced by stomach parietal cells in fasting conditions.. Levels rise 1-2h before a meal and decline to a minimum afterwards Structure: small peptide Actions: powerful stimulator of feeding by action in hypothalamus and brain stem Pathology: increased in people who have lost weight by dieting. Plasma ghrelin is very high in (rare) Prader-Willi obesity PEPTIDE YY (PYY) – inhibits feeding Distribution: produced in ileum and more distal bowel after meals Structure: small peptide Actions: has a prolonged action on Y2 receptors in hypothalamus to decrease food intake. STOP PRESS Two other hormones – oxyntomodulin (produced in small intestine from the same gene as glucagon) and obestatin (very recently discovered in the stomach and derived from same gene as ghrelin) are now being actively researched, with pancreatic polypeptide, as appetite suppressants. OTHER SITES OF HORMONE PRODUCTION Respiratory tract endocrine cells There are similar endocrine cells in the epithelium of the lower respiratory tract Adipose tissue – dealt with next year LEPTIN: peptide produce by adipocytes in relation to amount of body fat; inhibits appetite by action in hypothalamus ADIPONECTIN: peptide acting in muscle and liver to increase sensitivity to insulin. Decreased plasma adiponectin is associated with the ‘metabolic syndrome’ of increased BMI, insulin resistance and plasma lipid disturbance. Heart ATRIAL NATRIURETIC PEPTIDE Production: small peptide secreted by atrial myocytes 6 Release: atrial dilatation (i.e. increased venous return, right heart failure) Actions: stimulates loss of sodium (and water) in urine probably by an effect on glomeruli inhibits renin-angiotensin-aldosterone system reduces blood pressure (reduces venous return and cardiac output) Kidneys ERYTHROPOIETIN Production: glycoprotein produced by epithelial cells of glomeruli (and liver) Release: stimulated by reduced oxygen saturation of the blood (HIF); also by androgens and βadrenergic effects Actions: stimulates production of erythrocytes in bone marrow Abuse: by athletes wishing to improve the oxygen-carrying capacity of their blood. The risk is that the blood will become too viscous. RENIN-ANGIOTENSIN SYSTEM Renin - an acid protease produced by juxtaglomerular cells in the afferent arterioles of renal glomeruli Release: stimulated by sodium depletion, hypotension, dehydration, low renal artery blood flow, sympathetic nerve stimulation Renin cleaves plasma angiotensinogen to angiotensin I which is then cleaved by lung angiotensinconverting enzyme (ACE) to active angiotensin II, which stimulates aldosterone secretion, thirst, and vasoconstriction. Pharmacology: ACE inhibitors used in the treatment of hypertension. Renal 1α-hydroxylase activates 25(OH)D3 to 1,25(OH)2D3 (see bone lecture; calcium control lecture in Y2 Integrative Physiology). General Most tissues produce PROSTANOID/EICOSANOID hormones (prostaglandins, leukotrienes, thromboxanes). These act locally to a large extent (e.g. in inflammation) but can act at a distance – contraction of uterus in childbirth; effects on ductus arteriosus. Remember that some prostaglandins (PGF2, PGE2) stimulate the contraction of smooth muscle (e.g. in uterine contraction at parturition) whereas others (PGI = prostacyclin) inhibit the contraction (e.g. in vasodilation) Gonads, placenta Hormones produced by the gonads and placenta were dealt with in the Reproduction lectures. 7