Methotrexate SCG
advertisement

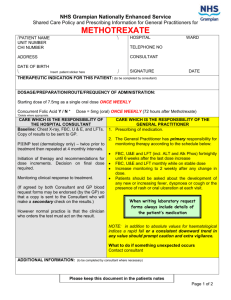
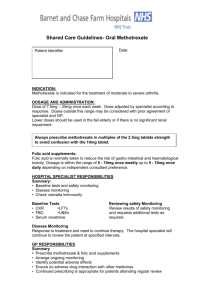
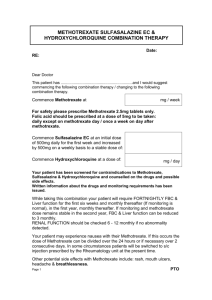
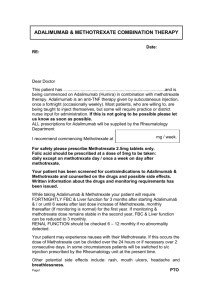
WORKING IN PARTNERSHIP WITH SHARED CARE PRESCRIBING GUIDELINE Methotrexate for the treatment of inflammatory conditions, including Inflammatory Arthritis, Psoriasis and Crohn’s Disease in adults Surrey PCT’s Medicines Management Committee classification: Amber N.B. The eligibility criteria included here apply to new patients commencing treatment under this guideline & not to existing patients whose treatment was initiated under the previous version. However, monitoring and discontinuation criteria apply to all patients. NOTES to the GP Amber drugs: Prescribing to be initiated by a hospital specialist (or if appropriate by a GP with specialist interest) but with the potential to transfer to primary care. The expectation is that these guidelines should provide sufficient information to enable GPs to be confident to take clinical and legal responsibility for prescribing these drugs . The questions below will help you confirm this: Is the patient’s condition predictable? Do you have the relevant knowledge, skills and access to equipment to allow you to monitor treatment as indicated in this shared care prescribing guideline? Have you been provided with relevant clinical details including monitoring data? If you can answer YES to all these questions (after reading this shared care guideline), then it is appropriate for you to accept prescribing responsibility. Sign and return a copy of page 4 to the requesting consultant at the Acute Trust. Until the requesting consultant at the Acute Trust has received a signed copy of page 7 indicating that shared care has been agreed all care (including prescribing) remains with the consultant at the Acute Trust. If the answer is NO to any of these questions, you should not accept prescribing responsibility. You should write to the consultant outlining your reasons for NOT prescribing. If you do not have the confidence to prescribe, we suggest you discuss this with your local Trust/specialist service, who will be willing to provide training and support. If you still lack the confidence to accept clinical responsibility, you still have the right to decline. Your PCT pharmacist will assist you in making decisions about shared care. Prescribing unlicensed medicines or medicines outside the recommendations of their marketing authorisation alters (and probably increases) the prescriber’s professional responsibility and potential liability. The prescriber should be able to justify and feel competent in using such medicines. The patient’s best interests are always paramount The GP has the right to refuse to agree to shared care, in such an event the total clinical responsibility will remain with the consultant. Reason for Update: New January 2011 with minor amendments July 2011 Page 1 of 8 Prepared by LMH Review Date: January 2014 WORKING IN PARTNERSHIP WITH Information This guideline covers the use of Methotrexate in Inflammatory Arthritis, Psoriasis and Crohn’s Disease (unlicensed indication) in adult patients. Methotrexate is an antineoplastic agent, which acts as an antimetabolite of folic acid. It also has Immunosuppressant properties and interferes with tissue cell reproduction to which actively proliferating Tissues, such as malignant cells are more sensitive. Methotrexate also inhibits antibody synthesis. Folic acid is also administered to reduce the risk of gastrointestinal side effects and hepatotoxicity and improves compliance. METHOTREXATE SHOULD ONLY BE PRESCRIBED IN MULTIPLES OF 2.5 MG TABLETS (THIS AVOIDS CONFUSION BETWEEN 2.5 MG and 10 MG TABLETS WHICH LOOK SIMILAR) (1) All patients should have an NPSA shared care booklet (purple), which patients should be encouraged use to record details of blood results and for the clinician to record any dose changes. (1) Dose Information Methotrexate is given ONCE weekly on the same day each week, swallowed whole with a glass of water one hour after food while sitting or standing. The therapeutic range is normally between 5mg - 25mg weekly, but higher doses may be used depending on patient response. Time to a therapeutic response is approximately 4 – 12 weeks. In exceptional circumstances, the dose can be separated over a 48 hour period if the patient is experiencing sideeffects. The doses used in practice may not correspond with BNF or SPC dosage ranges. (2) (3) If oral administration causes intolerance, or the maximum oral dose is not effective, the parenteral route of administration will be considered. Folic acid should be prescribed routinely at a dose of 5 mg weekly, to be taken at least 24 hours after the Methotrexate. Folic acid can be given at an increased dose e.g. 10mg and / or more frequently but NOT on the day of Methotrexate. Folic acid reduces the risk of hepatotoxicity and gastrointestinal side effects and improves compliance. This information sheet does not replace the SPC, which should be read in conjunction with this guidance. http://www.medicines.org.uk/emc/ (3) Prescribers should also refer to the appropriate paragraphs in the current edition of the BNF. (3) Inflammatory Arthritis Initially 5mg to 15mg orally once a week then adjusted gradually to achieve optimal response and minimise side effects with maintenance dose varying through a similar range. Once a response has been achieved, the dose should be slowly reduced until the lowest possible effective dose is reached. (Range 2.5mg - 25mg per week) Psoriasis Treatment of severe psoriasis 10 - 25 mg orally, once weekly, is recommended. Dosage should be adjusted according to the patient's response and the haematological toxicity. (3) Crohn’s Disease (unlicensed indication) For maintenance of remission: 10mg - 25mg once weekly orally. Induction of remission, 25mg once weekly, maintenance 15mg once weekly by intramuscular injection. (3) Reason for Update: New January 2011 with minor amendments July 2011 Page 2 of 8 Prepared by LMH Review Date: January 2014 WORKING IN PARTNERSHIP WITH Drug Interactions See Statement of Product Characteristics (SPC) and BNF for further details (2) (3) Avoid folate antagonist drugs especially Co-trimoxazole and Trimethoprim. NSAID’s and aspirin used concurrently are not contraindicated but may increase toxicity. Refer to BNF before prescribing antibiotics Alcohol should be reduced to three units per week during treatment with METHOTREXATE Adverse Effects Photosensitivity, marrow suppression, GI disturbances, hepatic fibrosis, infertility, teratogenicity, pulmonary toxicity, renal failure (rare). Patients with known allergy to Methotrexate should not receive the drug Contraindications and cautions Conception and pregnancy – Methotrexate is teratogenic. For men and women, contraceptive advice should be given, as pregnancy should be prevented for a minimum of 4 months after discontinuation of treatment. Male Fertility may be reduced. (4) (5) Breastfeeding is contraindicated. (4) Ascites, pleural effusions - Methotrexate elimination is reduced in patients with a third distribution space (ascites, pleural effusions). Such patients require especially careful monitoring for toxicity, and require dose reduction or, in some cases, discontinuation of methotrexate administration. (3) Vaccinations o with LIVE vaccines - must NOT be given. Inactivated polio is available although sub-optimal response may be seen. o Pneumovax and annual influenza vaccination is recommended. o Patients exposed to chicken pox or shingles (who have not had prior exposure to these viruses), passive immunisation should be carried out using VZIG. The Herpes Zoster immunoglobulins can be obtained from the Health Protection Agency telephone: Telephone: 0845 8942944 (Surrey & Sussex Health Protection Unit) NSAIDs - Can continue, if taken regularly and monitored, may increase risk of toxicity but is considered appropriate in most patients providing patient is monitored for toxicity. Avoid over the counter NSAIDs/aspirin. Low dose aspirin- The opinion of clinicians locally is that there may be some patients in whom the benefit of co-prescribing of low dose aspirin and low dose methotrexate outweighs the risks involved, provided that regular monitoring is carried out. Vitamins - some preparations containing folic acid or its derivatives may alter response to methotrexate. Patients should be advised to avoid the use of over-the-counter products without consulting their GP, Hospital Consultant, Community or Hospital Pharmacist. Blood Test Results WBC < 3.5 X 10^ 9 /l Neutrophils < 2 X10^9/l Actions Withhold drug; repeat WBC in 1/52, if normal continue, otherwise discuss with Specialist Dept Withhold until discussed with Specialist Dept Platelets <150 X10^9/l Withhold until discussed with Specialist Dept Liver function 2-3 fold rise in ALT >3 fold rise in ALT Reduce the dose by 2.5 mg and repeat in 2 weeks Withhold until discussed with Specialist Dept Reason for Update: New January 2011 with minor amendments July 2011 Page 3 of 8 Prepared by LMH Review Date: January 2014 WORKING IN PARTNERSHIP WITH MCV > 105-110 fl Mouth ulcers Check folate, TFT, B12 and treat if appropriate. If WCC normal repeat in 4 weeks, and continue drug. Stop MTX and seek advice Methotrexate toxicity can be increased as renally excreted. Caution in patients with comorbidities (i.e. dehydration), look for changes to medications, withhold if worsening renal function Ensure patient is on Folic acid. Split methotrexate dose over one evening and the next morning. If the nausea is severe, consider increasing the folic acid up to 5mg 6 days per week, omitting day methotrexate is taken. An anti-emetic can be prescribed. May respond to an increase in Folic Acid, as above Rash or severe oral ulceration Urgent FBC for WCC. Withhold until discussed with Specialist Dept. Look for alternative causes. Re-challenge with lower dose once symptoms settle. Menstrual dysfunction / Amenorrhoea May occur during treatment and for a short time following cessation. Otherwise unexplained dyspnoea/cough Pneumonitis may occur. Withhold drug and discuss urgently with Specialist Dept. Urgent CXR. Severe sore throat, abnormal bruising Immediate FBC and withhold until result of FBC available MCV>110 fl Renal impairment Nausea Methotrexate Injection Patients unable to tolerate oral methotrexate may be considered for transfer to parenteral methotrexate, by subcutaneous injection, using METOJECT® prefilled syringes. Metoject® is a licensed product of methotrexate 50mg/mL For transfer to Primary Care patients MUST be able to self administer. Methorexate is a cytotoxic drug and patients will be taught how to self administer these injections by specialist nurses trained handling of cytotoxic drugs. The initiating specialist must ensure that the patient will be supervised for a minimum of two injections or until competent prior to transfer to primary care. Training will include risk assessment, safe storage, handling and disposal, including spillage. (RCN – Guidance Administering subcutaneous methotrexate for inflammatory arthritis 2004) (5) In addition to the NPSA methotrexate booklet the patient should be offered the Metoject® patient’s guide. Patients should have their technique reviewed at least yearly by the specialist nurse and have a named contact. Monitoring: If a patient is changed from a stable dose of oral methotrexate to Metoject®, this is treated as a “dose increase”. Patients will need fortnightly monitoring for 6 weeks as per any other dose increase. All other precautions are the same as for oral METHOTREXATE. Metoject® Pre-filled Syringes DOSE VOLUME 7.5mg 0.15 mL 10mg 0.20 mL Reason for Update: New January 2011 with minor amendments July 2011 Page 4 of 8 Metoject® should be stored at room temperature and out of the sight and reach of children. Prepared by LMH Review Date: January 2014 WORKING IN PARTNERSHIP WITH 12.5mg 0.25mL 15mg 0.30 mL 17.5mg 0.35mL Metoject®, methotrexate injection, licensed dose range: 7.5mg to 30mg 20mg 0.40 mL Strength: 50mg/mL 22.5mg 0.45mL 25mg 0.50 mL 27.5mg 0.55mL 30mg 0.60mL Appendix A: Disposal of domestic cytotoxic sharps waste in Surrey Waste disposal: Metoject® is a cytotoxic drug and is therefore classified as ‘hazardous waste’ and must be disposed of in a ‘purple’ topped cytotoxic sharps bin. At least the initial cytotoxic sharps bin will be provided by the acute trust. Disposal arrangements will vary according to the policy of the local borough council. See Appendix A: Disposal of domestic cytotoxic sharps waste in Surrey RESPONSIBILITIES and ROLES Specialist responsibilities 1.Pre-treatment checks:Confirmation of diagnosis Exclude pregnancy. Consider possible drug interactions. Conduct baseline tests (FBC, U&E‟s, creatinine, LFTs (including AST/ALT), ESR, CPR, Chest X-ray Dermatologists / Gastroenterologists may request Type III collagen propeptide 2. Patient education:Discuss benefits versus risks with patient. Provide written information and a NPSA purple “Methotrexate patient held blood monitoring and dosage record booklet” and importance of showing this to all healthcare professionals. (1) Explain dose (in mgs and number of 2.5mg tablets) and once weekly administration. Ask patient to contact GP practice after one week to inform the practice that MTX has been started. Obtain patient’s consent if methotrexate is used for an unlicensed indication. If changing to self administered injectable methotrexate discuss cautions and benefits versus risks including handling precautions. To ensure the patient, if on parenteral methotrexate is aware of how to dispose appropriately of any ‘purple topped’ cytotoxic sharps bins and obtain a replacement bin. See Appendix A: Waste disposal. 3. Starting of treatment:Record baseline blood tests in “Methotrexate patient held blood monitoring and dosage record booklet” Issue hospital prescription for a minimum 4 weeks supply. Ask GP to continue prescribing and monitor blood results, providing baseline test results, a copy of the shared care agreement, details of methotrexate dose, its frequency, together with dose and timing of any folic acid. The frequency of monitoring and hospital review OR send fully completed copy of ‘Agreement for transfer of prescribing to GP’. Monitor efficacy, inform GP of any dose changes and document changes in patient held record book. Inform GP of any blood test results performed. Report adverse events to the MRHA (CHM) and GP. Reason for Update: New January 2011 with minor amendments July 2011 Page 5 of 8 Prepared by LMH Review Date: January 2014 WORKING IN PARTNERSHIP WITH General Practitioner responsibilities 1. Notify hospital within 14 days if not willing to prescribe methotrexate under shared care agreement. 2. Continue to prescribe methotrexate in line with hospital recommendation (prescribe 2.5mg tablets only). 3. Ensure that patient understands weekly dosing interval, and which warning symptoms to report. 4. Request and monitor blood tests and record on practice clinical system (see page 6- monitoring requirements). 5. Encourage patient to record blood test details in the “Methotrexate patient held blood monitoring and dosage record booklet” 6. Refer back to hospital if results are not within the normal range, or if there is cause for concern (e.g. toxicity). Contact specialist team for advice. 7. Ensure patient is scheduled for and attends reviews in secondary care. 8. Monitor for drug interactions – see under clinical information (page 3) 9. Adjust dose/ stop treatment as advised by specialist. 10. Monitor the patient’s overall health status. 11. Report adverse events to the specialist and MHRA (CHM). Monitoring requirements (if relevant to specific drug) (6) Baseline tests will be performed by the specialist and an initial prescription for 4 weeks issued. Dermatology or Gastroenterology patients may be required to have Type III collagen propeptide levels measured by the hospital to check for liver fibrosis. Monitoring to be performed by GP once shared care accepted:For the 1st Month: Two-weekly blood tests including, FBC, LFTs, U&Es, Creatinine, ESR (Rheumatology only if indicated by specialist.), CRP (if indicated by specialist). 2-4 weekly thereafter for 6 months post-initiation: FBC LFTs U&Es Creatinine ESR (if indicated by specialist) CRP (if indicated by specialist) After 6 months: If results remain stable, monitoring can be reduced to every 2-3 months (follow advice from specialist). Dose increases: Perform 2 - 4 weekly monitoring for at least 6 weeks after final dose change before considering changing to 2-3 monthly monitoring (follow advice from specialist). 1 2 3 4 5 6 7 Patient's / Carer’s role and responsibilities Ask the specialist or GP for information, if he or she does not have a clear understanding of the treatment. Share any concerns in relation to treatment with methotrexate Tell the Consultant, GP or Pharmacist of any other medication being taken, including over-the-counter products. Read the patient information leaflet included with the medication and the methotrexate information leaflet from the Arthritis Research Council (via the hospital clinic). Report any side effects or concerns you have to the Consultant, Clinical Nurse Specialist or GP. Read the NPSA “Methotrexate patient held blood monitoring and dosage record booklet” shared care booklet and ensure this is taken with them when seeing any healthcare professional. To show the booklet to community pharmacist. Maintain details of blood results. To attend appointments and organize blood tests as advised. If using parenteral methotrexate, to ensure that the ‘cytotoxic’ sharps waste is disposed appropriately. See Appendix A: Disposal of domestic cytotoxic sharps waste in Surrey. Reason for Update: New January 2011 with minor amendments July 2011 Page 6 of 8 Prepared by LMH Review Date: January 2014 WORKING IN PARTNERSHIP WITH SHARED CARE PRESCRIBING GUIDELINE Methotrexate for the treatment of INDICATION Agreement for transfer of prescribing to GP Patient details / addressograph: Name…………………………………….. Address………………………………….. ………………………………….. ………………………………….. DOB………………. Hospital No………………………………. Diagnosis:…………………………………………………………….. This patient has been started on oral methotrexate or self administered subcutaneous methotrexate on ……/……/…… for the above diagnosis. (delete as appropriate) Patient information has been given outlining the potential aims & side effects of this treatment and a patient held monitoring and dosage record book supplied. For parenteral methotrexate the patient has been trained to self administer and understands the precautions to be taken an initial cytotoxic sharps bin has been supplied. The following investigations where appropriate have been performed on ….../..…./..…. and are acceptable to start methotrexate: (6) Hb……………………..……….……..g/dl Urea…………….……………mmol/L MCV…………………………………..fl Creatinine……………………micromol/L WBC……………………………..…..x109/L ALT………………………… iu/L Platelets…………………………..…x109/L Alkphos…………………… iu/L Neutrophils…………………….……x109/L Gamma GT………………… iu ESR………………………………….mm/hr CRP………………………… mg/L CXR Procollagen III peptide (if requested) At the last patient review the drug appeared to be effectively controlling symptoms/ providing benefit: Yes / No The patients has now been stabilised on a dose of: ………………………………………….. I will arrange to review this patient regularly. Date of next clinic appointment:…………………………… Consultant: Address: Agreement to shared care, to be signed by GP and Consultant. Contact Number Consultant Signature: ……………………………………………….. Date: GP: GP Signature: Address: ………………………………………………… Date: Contact Number Main Carer: Contact Number: Key worker if appropriate: If shared care is agreed and GP has signed above please return a copy of this page to the requesting consultant or alternatively fax to: Fax Number: Contact Number: Reason for Update: New January 2011 with minor amendments July 2011 Page 7 of 8 Prepared by LMH Review Date: January 2014 WORKING IN PARTNERSHIP WITH BACK-UP ADVICE AND SUPPORT Contact details Specialist Telephone No. Email address: Specialist Dr Mark Lloyd, Consultant Rheumatologist 01276 604 604 Mark.lloyd@fph-tr.nhs.uk Sarah.langlands@fphtr.nhs.uk Dr Sarah Langlands, Consultant Gastroenterologist Fiona.antony@fph-tr.nhs.uk Dr Fiona Antony, Consultant Dermatologist Clinical Nurse Specialist Sara Burton, Rheumatology CNS Hospital Pharmacy Medicines Information 01276 604 604 Sara.burton@fph-tr.nhs.uk Kate Gilbert, Gastroenterology CNS Kate.gilbert@fph-tr.nhs.uk 01276 604 744 Medicines.information@fphtr.nhs.uk AUDIT / SURVEY (to be carried out by specialist clinic) Support groups and information websites Arthritis Research Campaign www.arc.org.uk Arthritis Care www.arthritiscare.org.uk NRAS www.rheumatoid.org.uk BSR www.rheumatology.org.uk Disposal of Cytotoxic Waste See Appendix A: Disposal of domestic cytotoxic sharps waste in Surrey Bibliography: 1. NPSA. [Online] [Cited: ] http://www.nrls.npsa.nhs.uk/resources/?entryid45=59800. 2. BNF No 61. British National Formulary. London : BMA & Pharmaceutical Press, 2011. 3. eMC. [Online] http://www.medicines.org.uk/EMC/default.aspx. 4. British Society for Rheumatology. [Online] [Cited: 28th July 2011.] http://www.rheumatology.org.uk/includes/documents/cm_docs/2009/d/diseasemodifying_antirheumatic_drug_dmard_therapy.pdf. 5. Appendix - Metoject. British Society of Rheimatology. [Online] August 2010. [Cited: 28th July 2011.] http://www.rheumatology.org.uk/includes/documents/cm_docs/2010/a/appendix_to_dmard_guideline_aug_2010.pdf. 6. Quick reference guideline for monitoring of disease modifying anti-rheumatic drug (DMARD) therapy. [Online] [Cited: ] http://www.rheumatology.org.uk/includes/documents/cm_docs/2009/d/dmard_grid_november_2009.pdf. 7. (RCN –Guidance Administering subcutaneous methotrexate for inflammatory arthritis 2004). [Online] Reason for Update: New January 2011 with minor amendments July 2011 Page 8 of 8 Prepared by LMH Review Date: January 2014