Barnet Hospital - Derwent Medical Centre
advertisement

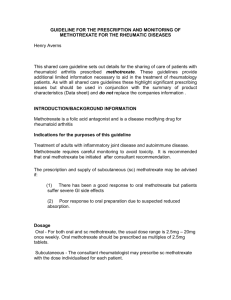
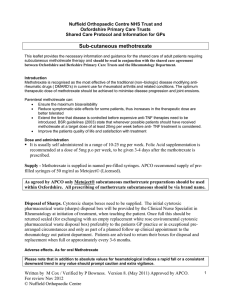
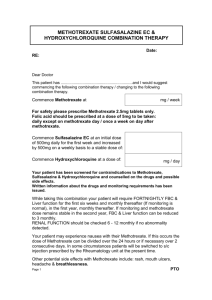
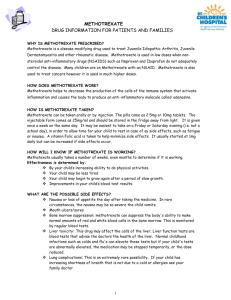
Shared Care Guidelines- Oral Methotrexate Date: Patient Identifier INDICATION: Methotrexate is indicated for the treatment of moderate to severe arthritis. DOSAGE AND ADMINISTRATION: Dose of 7.5mg – 25mg once each week. Dose adjusted by specialist according to response. Doses outside this range may be considered with prior agreement of specialist and GP. Lower doses should be used in the fail elderly or if there is no significant renal impairment. Always prescribe methotrexate in multiples of the 2.5mg tablets strength to avoid confusion with the 10mg tablet. Folic acid supplements: Folic acid is normally taken to reduce the risk of gastro-intestinal and haematological toxicity. Dosage is within the range of 5 - 10mg once weekly up to 5 - 10mg once daily depending on independent consultant preference. HOSPITAL SPECIALIST RESPONSIBILITIES Summary: • Baseline tests and safety monitoring • Disease monitoring • Check varicella immmunity Baseline Tests • CXR •LFTs • FBC •U&Es • Serum creatinine Reviewing safety Monitoring Review results of safety monitoring and requests additional tests as required. Disease Monitoring Response to treatment and need to continue therapy. The hospital specialist will continue to review the patient at specified intervals. GP RESPONSIBILITIES Summary • Prescribe methotrexate & folic acid supplements • Arrange ongoing monitoring • Identify potential adverse effects • Ensure no adverse drug interaction with other medicines • Continued prescribing is appropriate for patients attending regular review Safety Monitoring See the British Society for Rheumatology (BSR) guidelines for Second Line Drug monitoring- Appendix 1 Test results should be recorded in the patient’s booklet. ADVERSE EFFECTS AND PRECAUTIONS Nausea: Commonly encountered. Can occur at ant time during therapy. May resolve with dose reduction and/or addition of anti-emetic medication Decreased resistance to infection: Especially respiratory / urinary tract or shingles / chickenpox. Temporarily withhold methotrexate if patient is systemically unwell with significant infection requiring anti-infective intervention. Alopecia, rash, stomatitis, diarrhoea: Contact the specialist if severe or persistent. Respiratory function: Very rarely, methotrexate can cause interstitial pneumonitis, pulmonary oedema and fibrosis. Patient complaining of unexplained dyspnoea or unexplained dry cough should be referred immediately to the specialist. Alcohol: Patient are advised that alcohol consumption should be advised or kept to a minimum, due to the increased potential for liver toxicity. Contraindications include: Female patient must be advised not to conceive whilst receiving methotrexate. A reliable form of contraception should be used by men and women whilst on methotrexate and for at least 3 months after discontinuing it. Discontinue methotrexate and refer immediately if a patient or partner discovers they are pregnant whilst taking methotrexate. Contraindications include: • Severe renal or hepatic impairment. • Chronic or recurrent infections especially respiratory or urinary tract. • Severe anaemia, leucopenia or thrombocytopenia. • Untreated folate deficiency. • History of alcohol abuse / cirrhosis • Hepatitis Vaccines: Live vaccines should be avoided in patients taking methotrexate. Methotrexate should be discontinued for 3 months prior to the live vaccines and not restarted until 2 weeks after vaccination. Live vaccines are BCG, MMR, measles, varicella and yellow fever. Pneumococcal vaccine (IMPORANT revaccination is not recommended see BNF) and ‘FLU’ vaccines are recommended. Passive immunisation should be carried out using Varicella zoster immunoglobulin (VZIG) in non –immune patients if exposed to chickenpox or shingles. DRUG INTERACTIONS The following drugs may cause an increase in methotrexate serum level and should be used with caution. A FBC taken 1-2 weeks following initiation of new therapy is recommended to ensure toxicity has not occurred. • NSAIDs & Aspirin: • Tetracycline: • Penicillins: • Herbal Remedies Although a well documented interaction, NSAIDS or Aspirin (<300mg) are unlikely to cause any clinically significant adverse effect. A documented interaction unlikely to cause an adverse effect. A documented interaction unlikely to cause an adverse effect. Avoid if possible due to unknown interaction potential !!! DO NOT prescribe concomitant Trimethoprim or Co-trimoxazole !!! due to risk of pancytopenia. Co-prescription of drugs with potential hepatotoxic or nephrotoxic effects is also not advisable. Abnormal renal function can make these interactions for severe.Please contact the Pharmacy if you are in doubt about possible hepatotoxic and nephrotoxicty. Please refer to the Summary Product Characteristics for further drug interaction information- www.medicines.org.uk. COMMUNICATION Rheumatology department-Barnet Hospital: 020 82164969 Rheumatology department-Chase Farm Hospital: 020 83751608 Rheumatology department –Edgware Hospital: 020 87326697 Pharmacy Medicines Information- 020 83751486 Prepared: March 2005 Review: March 2008 Appendix 1: BSR Methotrexate monitoring guidelines A typical dose regimen may be: - 7.5mg weekly increasing by 2.5mg every 6 weeks to a maximum of 25mg. Lower doses should be used in the frail elderly or if there is significant renal impairment. Regular folic acid supplements are thought to reduce toxicity. Cotrimoxazole or trimethoprim must be avoided in patients taking methotrexate. Excess alcohol should be avoided. Live vaccines should be avoided in patients taking methotrexate. NSAIDs in addition to the above doses of methotrexate are not contraindicated. Annual ‘flu vaccine should be given. Pretreatment assessment: - FBC, U&E's, creatinine, LFT's, Chest Xray. Monitoring: - FBC fortnightly until 6 weeks after last dose increase and provided it is stable monthly thereafter. LFT's (incl. AST or ALT) with each blood test. U&E's 6-12 monthly (more frequently if there is any reason to suspect deteriorating renal function). Action to be taken: WBC <4.0x10^9/l withhold until discussed with rheumatologist Neutrophils<2.0x10^9 withhold until discussed with rheumatologist Platelets<150x10^9 /l withhold until discussed with rheumatologist >2-fold rise in AST, ALT withhold until discussed with rheumatologist (from upper limit of reference range) Unexplained fall in albumin withhold until discussed with rheumatologist Rash or oral ulceration withhold until discussed with rheumatologist New or increasing dyspnoea or cough withhold until discussed with rheumatologist MCV>105fl investigate and if B12 or folate low start start appropriate supplementation Significant deterioration in renal function reduce dose Abnormal bruising or sore throat withhold until FBC result available Please note that in addition to absolute values for haematological indices a rapid fall or a consistent downward trend in any value should prompt caution and extra vigilance.