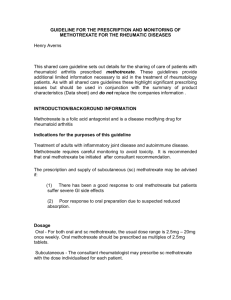
METHOTREXATE SULFASALAZINE EC
advertisement

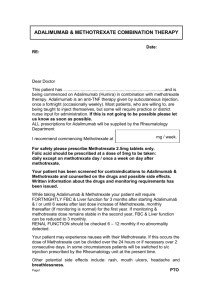
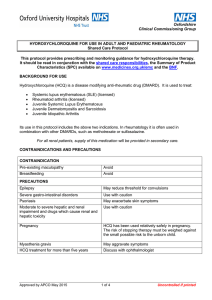
METHOTREXATE SULFASALAZINE EC & HYDROXYCHLOROQUINE COMBINATION THERAPY Date: RE: Dear Doctor This patient has ..................................................................and I would suggest commencing the following combination therapy / changing to the following combination therapy. Commence Methotrexate at mg / week For safety please prescribe Methotrexate 2.5mg tablets only. Folic acid should be prescribed at a dose of 5mg to be taken: daily except on methotrexate day / once a week on day after methotrexate. Commence Sulfasalazine EC at an initial dose of 500mg daily for the first week and increased by 500mg on a weekly basis to a stable dose of: Commence Hydroxychloroquine at a dose of: mg / day Your patient has been screened for contraindications to Methotrexate, Sulfasalazine & Hydroxychloroquine and counselled on the drugs and possible side effects. Written information about the drugs and monitoring requirements has been issued. While taking this combination your patient will require FORTNIGHTLY FBC & Liver function for the first six weeks and monthly thereafter (If monitoring is normal), in the first year, monthly thereafter. If monitoring and methotrexate dose remains stable in the second year, FBC & Liver function can be reduced to 3 monthly. RENAL FUNCTION should be checked 6 - 12 monthly if no abnormality detected. Your patient may experience nausea with their Methotrexate. If this occurs the dose of Methotrexate can be divided over the 24 hours or if necessary over 2 consecutive days. In some circumstances patients will be switched to s/c injection prescribed by the Rheumatology unit at the present time. Other potential side effects with Methotrexate include: rash, mouth ulcers, headache & breathlessness. Page 1 PTO Your patient may experience the following side effects with Sulfasalzine EC: nausea, diarrhoea, rash, mouth ulcers, initial headache, dyspnoea, discolouration of urine In men Sulfasalazine EC can cause a reversible reduction in sperm count Your patient should attend for a yearly optician review. A formal ophthalmology examination should be undertaken if the patient complains of visual symptoms. Your patient may notice blurring of vision or difficulty focusing when first taking Hydroxychloroquine. This improves over time or on reducing the dose of Hydroxychloroquine. Rarely Hydroxychloroquine causes maculopathy. If this occurs Hydroxychloroquine must be stopped and the Rheumatology Department contacted. Your patient may experience the following side effects with Hydroxychloroquine: rash, nausea, headache, sun sensitivity, hair lightening, hearing disturbance. If these occur they are usually reversible on lowering the dose of Hydroxychloroquine or stopping it. Treatment should be withheld and the Rheumatology Department contacted if: Neutrophils < 1.5 x 109 Platelets < 100 x 109 MCV > 105 fl unexplained fall in serum ALBUMIN rash or oral ulceration >2 fold increase in ALT (from upper limit of reference range) deterioration in renal function (reduce dose) abnormal bruising/sore throat (urgent FBC) BP increases of 10-15% (from baseline on 2 or more occasions) new/increasing dyspnoea or cough Please note that live vaccines should not be given to patients taking Methotrexate. Pregnancy and fatherhood should be avoided in all patients taking Methotrexate as it is teratogenic. Breastfeeding should be avoided while taking methotrexate. If your patient is planning pregnancy please contact the Rheumatology Department for advice. If your patient is in close skin contact with chickenpox or shingles, then Methotrexate should be stopped for 2 weeks and: Varicella Zoster antibody IgG levels checked (after discussion with Rheumatology or Microbiology) If negative your patient should receive 1gm IM immunoglobulin – via pharmacy at Victoria Hospital Kirkcaldy or Queen Margaret Hospital Dunfermline. If your patient develops chickenpox or shingles then Methotrexate must be stopped and high dose anti-virals should be commenced as soon as possible. The use of NSAID’s in a standard dose with Methotrexate is NOT contraindicated. Once stable most patients will be able to reduce or stop their NSAID. For full SPC please refer to Fife ADTC website. Yours Sincerely General enquiries: 01592 648193 Page 2 Updated October 2012 Version 1 due for review October 2013