Hepatitis B Liver Transplant Protocol
advertisement
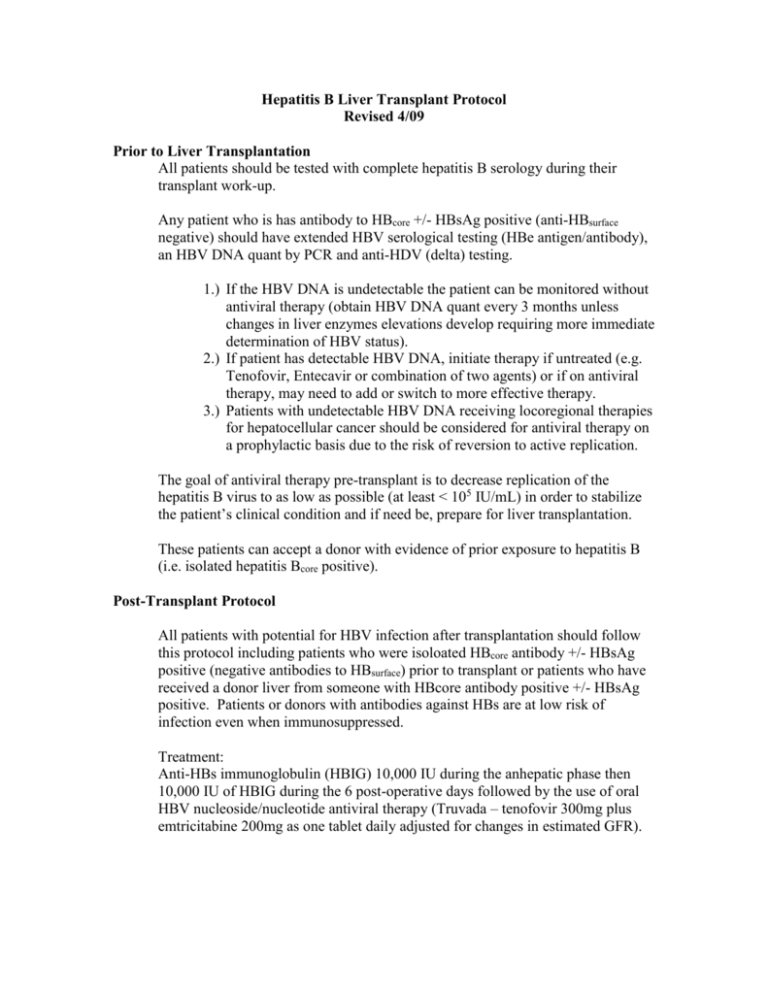
Hepatitis B Liver Transplant Protocol Revised 4/09 Prior to Liver Transplantation All patients should be tested with complete hepatitis B serology during their transplant work-up. Any patient who is has antibody to HBcore +/- HBsAg positive (anti-HBsurface negative) should have extended HBV serological testing (HBe antigen/antibody), an HBV DNA quant by PCR and anti-HDV (delta) testing. 1.) If the HBV DNA is undetectable the patient can be monitored without antiviral therapy (obtain HBV DNA quant every 3 months unless changes in liver enzymes elevations develop requiring more immediate determination of HBV status). 2.) If patient has detectable HBV DNA, initiate therapy if untreated (e.g. Tenofovir, Entecavir or combination of two agents) or if on antiviral therapy, may need to add or switch to more effective therapy. 3.) Patients with undetectable HBV DNA receiving locoregional therapies for hepatocellular cancer should be considered for antiviral therapy on a prophylactic basis due to the risk of reversion to active replication. The goal of antiviral therapy pre-transplant is to decrease replication of the hepatitis B virus to as low as possible (at least < 105 IU/mL) in order to stabilize the patient’s clinical condition and if need be, prepare for liver transplantation. These patients can accept a donor with evidence of prior exposure to hepatitis B (i.e. isolated hepatitis Bcore positive). Post-Transplant Protocol All patients with potential for HBV infection after transplantation should follow this protocol including patients who were isoloated HBcore antibody +/- HBsAg positive (negative antibodies to HBsurface) prior to transplant or patients who have received a donor liver from someone with HBcore antibody positive +/- HBsAg positive. Patients or donors with antibodies against HBs are at low risk of infection even when immunosuppressed. Treatment: Anti-HBs immunoglobulin (HBIG) 10,000 IU during the anhepatic phase then 10,000 IU of HBIG during the 6 post-operative days followed by the use of oral HBV nucleoside/nucleotide antiviral therapy (Truvada – tenofovir 300mg plus emtricitabine 200mg as one tablet daily adjusted for changes in estimated GFR). DOSING of TRUVADA: RENAL IMPAIRMENT Clcr ≥50 mL/minute: No adjustment necessary. Clcr 30-49 mL/minute: Increase interval to every 48 hours. Clcr <30 mL/minute or hemodialysis: Not recommended. Follow-up: Labs: Complete hepatitis B serology and HBV quant by PCR at 1 month post transplant and every three months thereafter for the first year and every 6 months after the first year. Consider discontinuing HBV antiviral therapy 6 months after a patient with HBeAg seroconverts to anti-HBe or any patient who seroconverts to anti-HBs (more robust endpoint). References: Lok AS, McMahon BJ AASLD Practice Guidelines: Chronic Hepatitis B. Hepatology. 2007; 45: 507–539. European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Management of chronic hepatitis B. J Hepatol 2009; 50: 227–242. Keefe EB, Dieterich DT, Han SH, et al. A Treatment Algorithm for the Management of Chronic Hepatitis B Virus Infection in the United States: 2008 Update. Clinical Gastroenterol Hepatol. 2008; 6: 1315-1341. Markowitz J, Martin P, Conrad A, et al. Prophylaxis against hepatitis B recurrence following liver transplantation using combination lamivudine and hepatitis B immune globulin. Hepatology. 1998; 28: 585-589. Samuel D, Muller R, Alexander G, et al. Liver transplantation in European patient with the hepatitis B surface antigen. N Engl J Med. 1993; 329: 1842 – 1847. Buti M, Mas A. Prieto M, et al. Adherance to Lamivudine after early withdrawal of hepatitis B immune globulin plays an important role in the long-term prevention of hepatitis B viral recurrence. Transplantation. 2007; 84: 650-654. Dumortier J, Chevallier P, Scoazec J, et al. Combine Lamivudine and hepatitis B immunoglobulin for the prevention of hepatitis B recurrence after liver transplantation: Long-term results. Am J Transplant. 2003; 3: 999-1002.