pathological changes after living donor liver transplantation in
advertisement
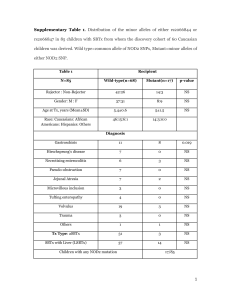
PATHOLOGICAL CHANGES AFTER LIVING DONOR LIVER TRANSPLANTATION IN PEDIATRIC AGE GROUP M. S. El Monayeri1,2 , MD, M. A. Kotb2,3, MD, N. A. Hegazy1, MD, A. F. Hamza1,2, MD, M. S. El Meteini1,2, MD Ain Shams Center of Organ Transplantation1, Wadi El Neel Hospital2 and Department of Pediatrics, Cairo University3, Cairo, Egypt Introduction: The long term histological outcome after pediatric liver transplantation is not yet fully understood. Histological abnormalities are commonly present; with many known to be found in some children who appear clinically well with good graft function. Objectives: The purpose of this study was to define histopathological changes during longterm follow-up in the liver allograft of children who had undergone living donor liver transplantation Methods: Forty infants and children (20 males and 20 females) had Living donor liver transplantation at Wadi El Neel hospital between October 2001 and March 2010. Their age ranged between 8 months and 16 years. Thirty two of the transplanted cases, who survived more than one year, were included in the analysis. Sixty six protocol and clinically indicated liver biopsy specimens were reviewed, with at least 1 year follow-up; biopsy findings were correlated with clinical, biochemical and serological findings. Results: Normal or near normal histology was reported in 11 (34.4%) cases. Chronic hepatitis was diagnosed in 7 (21.8%) cases (mild in 5 cases and moderate in 2 cases), serological findings were normal, however, patients responded to treatment with increase immunosuppressant and addition of steroids. Late cellular rejection was reported in 4 (12.5%) cases, ductopenic rejection in 5 cases (15.6%), biliary/vascular complications in 4 (12.5%) cases and recurrent disease ( HCV) in 1 (3.1%) case. Among cases with abnormal biopsy findings (21 cases,) serum transaminases were normal in 5 cases (23.8%) and the biopsies showed late cellular rejection, chronic hepatitis, ductopenic rejection and periportal fibrosis; follow-up showed progression of disease process. Graft fibrosis was detected as an isolated finding or associated with other pathological changes. The incidence of graft fibrosis increased with time (18.75%, 25.32% and 43.7% at 1,3 and 5 years respectively( Conclusion: Children are more liable to develop late cellular rejection and idiopathic chronic hepatitis, but they are much less likely to suffer problems with disease recurrence. The cause of chronic hepatitis in transplanted allografts is uncertain and may be immune mediated, representing a hepatitic form of chronic rejection. Transplanted livers of immunosuppressed children who are clinically healthy and have normal transaminase levels may show histological changes necessitating change of therapeutic strategies