Treacher Collins
advertisement

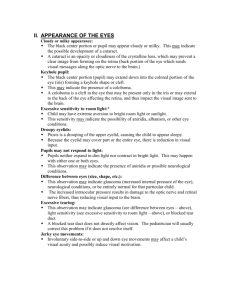
TREACHER COLLINS SYNDROME Mandibulo-facial dysostosis - MFD. First reported by Thompson (1846) and later, in depth, by Berry (1889). E. Treacher Collins, an English ophthalmologist, reported (1900) the colobomas of the lower lid and the associated malar defect. Franceschetti coined the term mandibulo-facial dysostosis (1944). Bilateral defects in structures derived from the 1st and 2nd branchial arches. Variable clinical spectrum from slight anti-mongoloid slant of the eyes to full blown picture. Some call the complete form as Franceschetti syndrome INCIDENCE AD variable penetrance; 60% sporadic 1 in 25,000 to 50,000 live births All race groups are affected. DIAGNOSTIC FEATURES 1. Anti-mongoloid slant of the palpebral fissures (downward sloping) 2. Eyelid colobomas (eyelid cleft) of the outer portion of the lower eyelids (almost constant feature) o most common position is at the junction of the lateral and middle third of the lower lid. o Absent eyelashes medial to the coloboma o Coloboma is present in the lower eyelid in Treacher Collins syndrome and in the upper eyelid in Goldenhar syndrome. 3. Malar hypoplasia, 4. Mandibular hypoplasia o typically contain an enlarged antegonial notch that can be easily observed on a lateral cephalogram. o The gonial angles are obtuse o obstructive apnea is frequently caused by mandibular hypoplasia that retrodisplaces the base of the tongue into the oropharynx, resulting in obliteration of the airway. o Anterior open bite and give the appearance of lower face retrusion. 5. Defects of the external ear and occasionally of the middle and inner ear o Conductive hearing loss(50%) 6. Macrostomia, high palate, malocclusion o cleft palate are often present 7. Blind fistula between the angle of the mouth and the ears 8. Anteriorly displaced sideburns - atypical hair growth in the form of tongueshaped processes of the hairline extending toward the cheeks most frequent findings: downward-slanting palpebral fissures, hypoplasia of the zygomatic complex, hypoplasia of the mandible, conductive deafness, any degree of microtia, and atresia of the external ear canal. GENETICS Autosomal dominant (chromosome 5q) Mutation in the TCOF1 (Treacle) gene The genetic defect produces a variably penetrant genetic phenotype. The gene encodes a nucleolar phosphoprotein, and its mutation conducts to premature ending of the coded protein (haploinsufficiency). Miscarriages in families with MFD is common. Between generations, there is a high variability in phenotypic expression, whereas among affected siblings of the same generation, there is low variability. PATHOGENESIS Due to aberrant expression of a nucleolar protein critically required during human craniofacial development Down-regulation of treacle expression results in inhibition of ribosomal DNA transcription and cell growth. Theories: 1. Failure of differentiation of branchial arch mesoderm. 2. Defective facial bone ossification. 3. Tissue ischaemia resulting from stapedial artery hypoplasia. 4. Developmental defects of neural crest cells (the current theory according to McC). All major aspects of MFD are expressed by the 15 week foetus. In mice, phenotype expressed following the administration of retinoic acid on gestational day 8. CLINICAL FEATURES AND CLASSIFICATION Complete form shows the presence of Tessier clefts 6, 7 and 8. Great variability in the degree of phenotypic expression and thus much confusion regarding classification. Obligatory features 1. Anti-mongoloid palpebral fissures 2. Colobomas of lower eyelids 3. absent eyelashes medial 1/3-2/3 4. Malar defects 5. Pre-auricular hair displacement 6. Mandibular defects 7. Micrognathia 8. Fish-like facial appearance Frequent features 1. Atresia of lacrimal puncta – nearly always inferior puncta 2. Auricular defects 3. External auditory canal defects 4. Deafness 5. Pre-auricular sinuses 6. Nasal deformity 7. Macrostomia 8. High arched palate 9. Malocclusion 10. Open bite 11. Skeletal defects Infrequent features 1. Flat parieto-occipital bone 2. Colobomas of iris and upper eyelid 3. Absence of meibomian glands 4. Hypertelorism 5. Cleft palate 6. Absent parotid gland 7. Under-development of epiglottis 8. Mental retardation Sleep apnoea and SIDS common in these children. Due to 1. small pharynx 2. small mandible On endoscopy, the pharynx has been found to be 50% smaller than normal. Choanal atresia can occur. The small mandible worsens the scenario. As a consequence of sleep apnoea, behavioural and intelligence changes have been noted. It is thus important to recognise. Always bilateral. Unilateral form does not exist. Cases reported as unilateral are usually variations of craniofacial microsomia or 1st and 2nd brachial arch syndromes. Differential 1. Nager’s acrofacial dysostosis autosomal recessive disorder characterized by a face similar to that of individuals with Treacher Collins syndrome. Very rare <100 cases also have bird-like features and the mandibles are typically retrognathic with an obtuse gonial angle and an enlarged antegonial notch. The distinction lies in the fact that they have more severe auricular deformities than patients with Treacher Collins syndrome. They also have characteristic upper and lower extremity defects in a preaxial distribution (thumb/radius hypoplasia). Unlike in Treacher Collins, lower eyelid colobomas are not as frequent but cleft palate is practically universal. genetic mutation associated with Nager syndrome is currently unknown. 2. Miller’s syndrome postaxial acrofacial dysostosis autosomal recessive 30 cases worldwide 3. Goldenhar’s Colobomas in Goldenhars involve the upper lid TCOG1 gene negative RADIOGRAPHIC FEATURES Obligatory 1. Deficient zygoma 2. Hypoplastic mandible 3. Antigonial notch on ramus of mandible (notch on outer border of mandible) Frequent 1. Small mastoids with hypopneumatization 2. Defects of ossicles of middle ear 3. Straight naso-frontal angle 4. Deficient zygomatico-temporal bones 5. Hypoplastic maxilla and sinus 6. Cleft palate 7. Short ramus and body of mandible 8. Obtuse (straight) naso-frontal angle Infrequent 1. Styloid process malformations 2. Sella turcica defects 3. Persistant frontal suture 4. Hypoplasia of the frontal sinus 5. Acute cranial base angle 6. Deficient palatine bones 7. Choanal atresia 8. Inner ear malformations TREATMENT Best treated by multi-speciality craniofacial team. Non surgical treatment 1. Genetic counselling for the family 2. Psych counselling for the child 3. Speech therapy, audiology, etc 4. Help with early feeding Surgical considerations A plan of Mx needs to be tailored to the patient’s specific deformities and timed to take into account their normal facial growth and psychosocial needs. Timing is important. Generally, bone reconstruction should precede soft tissue correction. Modern craniofacial approaches (bicoronal, intra-oral incisions) should be used to minimise scarring. Autogenous tissue should be used (calvarial, rib, costal cart grafts). Alloplasts avoided. Narrowed airway often leads to difficulties with anaesthesia Aims of Surgical Treatment 1. To close the palpebral coloboma 2. To build up the zygoma 3. To correct the malformed ear 4. To correct macrostomia 5. To establish normal occlusion 6. To harmonise the profile Surgical sequence Infancy 1. Securing the airway a. prone to sleep apnoea and SIDS positioning or even tracheostomy b. Early distraction has been used 2. Protect the globe a. Exposure may need urgent attention 3. Feeding difficulties a. gastrostomy <1 year old 1. Cleft palate repair 2. remove skin tags 3. macrostomia correction Age 5-10 1. Mandibular reconstruction a. Mandibular distraction for Pruzansky I and II b. Type III defects require costochondral rib grafts, which are best performed during the mixed dentition phase (age 6 to 10 years). 2. Zygoma reconstruction a. Rib grafts 3. Auricular reconstruction 4. Orthodontic treatment, including possible functional appliance therapy to promote eruption and growth of the dentoalveolus on the affected side. Age 10-19 1. Definitive orthognathic surgery a. Sagittal split b. LeForte 1 c. Genioplasty 2. Soft tissue augmentation MX OF SPECIFIC DEFORMITIES 1. Maxillary and orbital deficiencies Problems 1. Orbit is oval in shape and inclined downwards laterally; 2. The supra-orbital ridge slopes downwards from medial to lateral; 3. The orbital floor is deficient infero-laterally (as for a Tessier 6 cleft); 4. Zygoma is small and rudimentary, often as only a small spine of bone above the glenoid fossa ( as in a Tessier 7 cleft); 5. Maxilla is laterally and anteriorly positioned and is deficient in height and width. The maxilla is flattened; 6. The muscles of the orbit and of mastication (temporalis / masseter, medial and lateral pterygoids) may be fused across the infra-orbital cleft which can make dissection difficult. Requirements 1. Reconstruction of the zygomatic arch, zygoma, anterior maxilla, infra-orbital rim. 2. Bone grafting of the infero-lateral orbital deficiency or cleft. 3. Correction of downward slope of superior orbital rim. 4. resuspension of lateral canthus Treatment Historically various graft augmentation materials have been used: dermal-fat, cartilage and bone. Bone grafts as rib or calvarial onlays have been used extensively. Calvarial grafts may be advantageous: in the operative field, good size and contour, minimal donor site morbidity. Can be used as split or FT calvarial bone graft or as vascularised bone pedicled on the temporalis muscle and fascia. less resorption of calvarial grafts as compared to rib grafts. Less resorption of vascularised bone compared to grafts Usual timing advocated is correction of bony defects < 3 years of age. Specific treatment involves correction of the anti-mongoloid slant by burring or resection of upper lateral part of orbit and onlay of bone to augment the zygoma, floor and lateral orbital rims. The cleft in the bone usually extends from the inferolateral part of the orbit to the inferior orbital fissure and this must be closed with a piece of bone to prevent prolapse of the orbital contents into the temporal fossa and to raise the orbital floor to a horizontal level. The LCL must also be repositioned. There is a tendency for bone grafts to resorb with time so initial over-correction and subsequent further surgery is required. The soft tissue cover over the bone is often thin and requires coverage with a flap: pericranial (temporo-parietal) or free flap. Eyelid Deformities Variable: anti-mongoloid slant to extensive colobomas lacking skin, tarsal plate, orbicularis oculi muscle and conjunctiva. Severe cases can have colobomas of the upper lid and an absence of the lateral canthus (cleft 8). Aggravated by the underlying deficiency of the bony orbit. The cornea is rarely in danger of exposure damage. If the eyelid coloboma is small and well managed with topical lubrication, then surgery may be delayed until later in childhood. Usually, it is corrected by direct closure. If the eyelid coloboma is large, immediate surgical closure is usually needed to prevent corneal compromise. A 2-stage reconstruction may be required for those defects that occupy greater than 40-50% of the lid. Eyelid reconstruction difficult, but follows the usual principles Methods that have been used: 1) Direct closure 2) Transposition flaps from the upper to lower lid (I Jackson PRS 1981) Full thickness laterally based upper lid flap leaving a superior rim of tarsus attached to the levator Lateral canthal repositioning 3) Skin grafts (FT) 4) Kuhnt-Szymanowski procedure 5) Z-plasty (Tessier) Consists of Z-plasty for cutaneous lengthening, overlapping sutures of the preseptal orbicularis muscle and canthopexy. 6) Lateral tarsorrhaphies, canthoplasties and canthopexies 7) Temporalis fascial slings 8) Tarsoconjunctival flap from the upper lid (Hughes) or modified Cutler-Beard procedure for upper lid coloboma 9) Rotation flap – Tenzel’s semicircular flap All the above leave scars on the lower lid. The method recommended in McC is excision of the coloboma and lower lid lateral to it combined with lateral canthopexy to fill the defect and lift the antimongoloid slant. This method avoids scars on the lid. Mandibular Hypoplasia Micrognathia and microgenia are consistent features of Treacher Collins. The lower face is markedly retruded on profile. The condyles, coronoid, ramus and body may be malformed and deficient. The mandibular angle is obtuse and there is an antigonial concavity, considered by some to be a diagnostic feature. Anterior open bite and class II occlusion are common. Orthognathic surgery often delayed until growth is complete. Osteotomies augmented by bone grafts are the usual method of treatment. Distraction osteogenesis should be considered. Open bite may need later correction with either Le Fort I, or occasionally Le Fort II, maxillary osteotomy. Minor open bites can be treated by removal of bicuspids and orthodontics. Orthodontics should be used in any case. Genioplasty may be considered. Rhinoplasty and anterior maxillary set back may be required for a prominent mid face. 4. Other problems Ear: Variable deformity from normal to complete absence. Reconstruction as normal. Anteriorly displaced sideburns can be repositioned by transposition - leaves bad scar. Absent medial lashes: no effective treatment.