Guidelines for Hospital Internal Accounting
advertisement

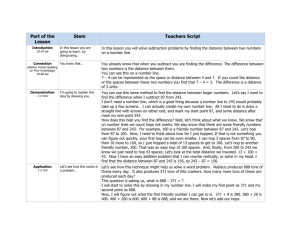
Guidelines for Hospital Internal Accounting South Carolina Healthy Outcomes Initiative April 10, 2015 Purpose This paper is prepared in accordance with recommendations provided by a special task force of the SCDHHS Hospital and Clinic Innovations Healthy Outcomes Program workgroup’s Fiscal Integration Transformation Team. It is intended only to present functions determined to be best practices by its preparers. These practices are only intended to stimulate the considerations of issues unique to this program and are not to be considered a standard protocol. The contents of this paper have not been reviewed or accredited by the American Institute of Certified Public Accountants (AICPA), Governmental Accounting Standards Board (GASB), Financial Accounting Standards Board (FASB) or any third party accreditation agency or review board or governmental agency. Hospitals should give consideration to having their accounting process for Proviso 33.26 reviewed by their accounting audit group prior to the end of their Fiscal Year. Executive Summary In 2013, the South Carolina Healthy Outcomes Plan Initiative (HOP) was initiated through Proviso 33.34 (H. 3710), which directly linked disproportionate share funding and financial incentives through September 2014 to hospital participation in local HOP initiatives designed to reduce system cost and improve health outcomes. HOP was continued in 2015 by the South Carolina Legislature and is anticipated to be approved again for 2016. Each HOP is designed individually by the contracting hospital or hospital system to address the particular needs of their community. Currently all South Carolina hospitals are participating either individually or by way of a multi-hospital system HOP program. It has become obvious that hospitals are accounting for HOP activities in a number of different billing and accounting structures. Hospital executives are encouraged to review their current accounting procedures for HOP accounts and give consideration to the following observations. Introduction Proviso 33.26 (H. 4701), passed in June 2014, extended the time frame of HOP and provided funds for hospitals and community partners participating in HOP through September 2015. Hospitals indicate their participation in HOP by attestation to the SC Department of Health and Human Services (SCDHHS) and by demonstrating enrollment of people eligible for HOP and the completion of care plans for their HOP participants. Statewide, the goals for the 2015 program are to enroll 12,756 people into HOP by June 30, 2015 (based on the SCDHHS contract) and to have a care plan in place for each enrolled participant. Beginning October 1, 2014, persons eligible for HOP enrollment are uninsured individuals below 194% of the Federal Poverty Level (FPL), chronically ill high utilizers of a hospital Emergency Department. Chronic conditions include diabetes, behavioral health conditions, cardiovascular disease, end stage renal disease, hypertension, Chronic Obstructive Pulmonary Disease, sickle cell, HIV/AIDS, and other conditions upon approval by SCDHHS. More specifically, eligible patients meet at least one of the following criteria: 1 Unplanned readmission within 30 days in the past year Two or more admissions in the past year Two or more Emergency Department visits in the past year Poorly controlled chronic condition(s) combined with one or more hospitalizations in the prior year Three or more approved chronic conditions Seven or more medications Poorly controlled chronic condition with a comorbid behavioral health diagnosis or social care need(s) Patients can be enrolled at the hospital, a provider partner or at any other location as the eligible patient approaches the health system or as outreach to a potentially-eligible patient population is conducted. An enrollment is simply the patient’s signing of the hospital’s HOP patient authorization which informs patients that their information will be shared with SCDHHS and describes how their information will be used. When a participant is enrolled, the hospital and/or HOP partners are expected to conduct surveys and screenings which include a Medicaid and Insurance Eligibility Screening. The Medicaid and Insurance Eligibility Screening should then be completed annually. Only uninsured individuals less than 194% of the Federal Poverty Level may participate in the 2015 HOP program. Prior to October 1, 2014 there was no FPL requirement. Participants enrolled with higher incomes prior to October 1, 2014 can remain in HOP until February 1, 2016. Hospital responsibilities: Under the HOP contract, hospital and hospital system providers agree to develop care strategies with partnered primary care physicians, FQHCs and other safety-net providers to co-manage the care of enrolled participants. Hospitals in the programs serve as the coordinator of care and are responsible for funding the provision of all related care by sub-contracting primary care physicians, FQHCs and other providers to direct HOP participants to the appropriate level of care and to encourage routine and preventative care. These payments are made at the hospital’s expense. In addition to the delivery of medical care, patient care plans should include the provision of necessary medications, monthly meetings, a number of social determinants and behavioral health evaluations. Please refer to your hospital’s HOP contract and your approved HOP for further information regarding the required delivery of care and documentation. While HOP is not an insurance plan and does not contractually require a prescribed set of benefits, the program is intended to improve the overall health status of the eligible participants. Funding: All money allocated for HOP is available for use in innovative approaches to meeting this goal. SCDHHS indicates that the following funding is intended to support HOP participants and staffing in 2015, which is available by community, and includes: Hospital rate increase of 2.75% for services provided to Medicaid patients Primary Care Enhancement provided to hospitals Allocation to hospitals of $20 million in 2013 disproportionate share funds Baseline funding for Federally Qualified Health Centers Potential Growth funding for Federally Qualified Health Centers Funding for partnering Free Clinics Two of these sources of funding relate specifically to HOP hospitals. First, the HOP requires SCDHHS to make available to hospitals a $35 million aggregate rate increase beginning October 1, 2013 to help fund new program expenses. SCDHHS determined that the best means to distribute the $35 million is through an across-the-board 2.75% rate increase paid directly to hospitals from SCDHHS Medicaid 2 payments for fee for service claims. The adjustments are to be paid directly to Medicaid Managed Care Organizations for all MCO claims. It is the MCOs’ responsibility then to pay hospitals this amount in full with no withholding of administrative or other fees. This rate increase should not be made by the MCO as a market basket or other contractual adjustment, but is intended specifically to cover a portion of the cost of a hospital’s HOP. This same methodology has been extended to both 2014 and 2015 HOP programs. The 2014 HOP Program also provided $5 million in Primary Care Enhancement Funds to safety net hospitals in particular need of start-up funds. These funds are distributed to hospitals based on a Facility Needs Index developed by the state. In the 2014 HOP, only HOP hospital providers above a Facility Needs Index of 3.0 received enhancement funding. Designated hospitals received $1,060 per assigned participant of a statewide total of 8,511 participants. In the 2015 program, the number of assigned participants increased to 12,756. Enhancement funds were increased to $7.5 million and distribution was restructured to allow all hospital participants to receive funding. Hospitals with a Facility Needs Index in the upper 50% of hospitals receive a per-participant rate of $800 while the remaining facilities receive $400 per assigned participant. The 2015 Enhancements will be converted to a Per Member Per Month (PMPM) and distributed to hospitals quarterly based on the contract. Disproportionate share funds are at risk for hospitals that do not participate in HOP. It is important to demonstrate active HOP participation, as there will be no reductions in disproportionate share funds for hospitals actively participating in HOP. Hospital Financial Best Practices-Patient Accounting Classification: The HOP is designed to enhance the care of a select population of the uninsured. SCDHHS has made it clear that HOP is not an insurance plan. HOP is also not a Medicaid program. No charges can be billed to any patient or third party on accounts qualifying as HOP related. Beginning October 1, 2014, hospitals must apply a 194% FPL test for participation in HOP. It is recommended that HOP accounts remain classified as Uninsured, but with a plan code designating the account as HOP in much the same internal billing structure as Medically Indigent Assistance Program (MIAP) accounts. Payments and Contractuals: As noted above, hospital HOP accounts are funded by a 2.75% rate increase paid for routine Medicaid charges using federally matched (FMAP) Medicaid funds. These funds can only be used to pay for Medicaid-covered services. Therefore, these payments are not intended to be applied to uninsured HOP accounts. For the purpose of accounting, this should simply be viewed as a Medicaid rate increase. Likewise, the Primary Care Enhancement Funds are designated to pay for primary care provided outside of the hospitals and are not account-specific payments and are therefore also unrelated to individual HOP accounts. There will generally be no payment at all applied to HOP applicable accounts, therefore charges for HOP-related accounts must be written off in full, regardless of a hospitals standard charity protocol and qualifications. To be considered eligible to participate in the Proviso 33.26 HOP, an individual applicant’s household income is required to meet a designated FPL of less than 194%. The Fiscal Integration task force has agreed that, for the purpose of the HOP, this income amount should be considered charity as it compares to the SCDHHS MIAP requirement of 200% FPL and to most South Carolina hospitals’ own charity guidelines. For this reason, the task force is of the opinion that these accounts should be 3 written off in full as a charity deduction and recommends that a special indicator be applied to identify these adjustments for tracking, accounting and reporting purposes in much the same approach as the hospitals current MIAP procedures. These accounts should be written off in total as a HOP Charity. No sliding scale payments should apply. As the Proviso provides no specific guidelines other than the 194% FPL, it is not a requirement that participants complete a SCDHHS MIAP application or a hospital charity application. The participant’s income should be documented in accordance with the hospital’s routine procedures. Hospital Financial Best Practices-General Ledger It will be very important to track revenues and expenses applicable to the HOP program. This information will be necessary for cost accounting in future periods to determine if your hospital has a net gain or loss from this program. This information will be important to hospitals for determinations regarding participation and future negotiations. This will also be important at the state level to determine the overall is meeting its goal of reducing cost while improving the delivery of care. A general ledger department should be created specific to the HOP Program to distinguish the accrual of revenues and expenses specific to the program. Net Revenue: HOP hospital charges and contractual adjustments require no changes from the current hospital billing and accounting functions. The 2.75% rate increase is part of the Medicaid or MCO reimbursement rate and should remain recorded as patient payments. HOP Enhancement Payments should be recorded as revenue on the HOP general ledger department as Other Revenue. HOP charges written off with a charity deduction should also follow the same GL posting of other charity programs already in place. Again, it is recommended that these write offs be identified separately from other charity adjustments. Expenses: It is recommended that hospitals create a new GL department for the HOP program. Recording the cost of the HOP program will require efforts on two different levels. Expenses associated with the routine delivery of care provided internally should follow accounting policies and procedures already in place. Internal direct expenses such as salaries and other operational expenses attributable to the program should be coded to the HOP GL Department. Other costs unrelated to the hospital’s direct cost of care to HOP patients will also need to be recorded for tracking purposes . Contracted expenses such as payments for direct costs such as PMPM payments for physician care and costs billed by FQHCs, home health, free clinics, etc. should be expensed to this department. It is not recommended that administrative and overhead costs be allocated to the HOP Department. Cost Accounting: Again, it will be vital to estimate the overall cost of the HOP program to your facility in order to determine a gain or loss from the program. Your hospital’s usual cost accounting policies and procedures should be applied to these efforts. Estimates should encompass the 2.75% Medicaid rate increase, total HOP Primary Care Physician Enhancement Payments, and any other incidental revenues and expenses attributable to the program. For the sake of cost accounting for the internal delivery of care, if a hospital has no standardized method of determining the cost of care, these expenses may be determined by applying hospital cost-to-charge ratios (RCC) to HOP account balances. Hospitals should develop a means of determining the cost of care for HOP patients and similar non-participating patients to estimate cost savings of the program. Hospitals should address Medicare, Medicaid and other cost reporting procedures for the HOP program directly with their Cost report preparer. 4