Pain Management - Suffolk County Community College
advertisement

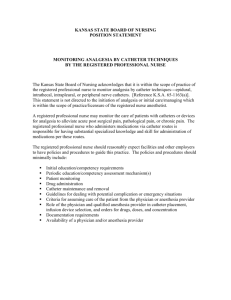
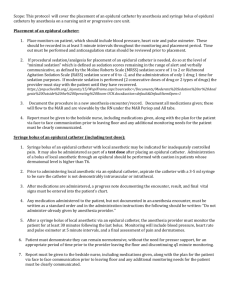
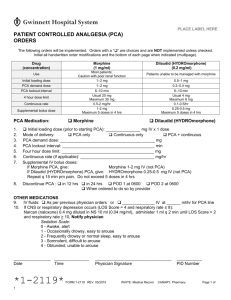
NUR133 Burger SUFFOLK COUNTY COMMUNITY COLLEGE School of Nursing NUR133 LAB #9 Pain Management Instructions: Complete this worksheet prior to the lab session. Procedural checklists should also be reviewed. You will be required to demonstrate your preparation by participating in the discussion of this worksheet and performing the skills demonstrated by the instructor. Definition of Pain: “Pain is whatever the experiencing person says it is, existing whenever he or she says it does.” – Margo McCaffrey, R.N. Identify TYPES of pain: List (3) types of PAIN SCALES: PATIENT CONTROLLED ANALGESIA (PCA): allows patients to self-administer small continuous doses of IV narcotics, as they feel the need. Advantages: 1. better pain control: more constant serum levels of narcotic avoids peaks and troughs 2. less sedation and respiratory depression 3. fewer post-op complications 4. saves nursing time 5. increases patient autonomy Selection of Patients 1. Adequate renal, hepatic and respiratory function 2. Alert and oriented 3. Able to demonstrate an understanding of the system and how to use it 4. Motivated to use PCA 5. No allergy to the narcotic 6. Covered by insurance 7. Research shows that addicted patients don’t misuse PCA. In fact PCA may lessen opioid demand and obviate drug seeking behavior. Components of System 1. Infusion pump with a chamber that houses the pre-filled syringe of narcotic (obtained from pharmacy and stored in narcotic cabinet). 2. Timing unit linked to a switch or button that is activated by patient to deliver a preset dose of medication (ordered by physician). 3. Tubing that delivers the medication from the pre-filled syringe through the timing unit to an indwelling IV. Burgerk rev0108 1 NUR133 Burger Define the following terms Loading Dose: Lock-out interval: Basal Rate: Drug Morphine Dilaudid (Hydromorphon e) Common Drugs and Dosing For PCA Pump Common Hourly Onset Duratio Concentrations Rate n In mg. per ml. 1 mg. per ml. 6-10ml per hr. immediat 4-5 hr. 100mg in 100mL (6-10-mg per hr.) e 0.2mg per mL 20mg in 100 mL 6-10ml.per hr. (1.2-2mg/hr. 10-15 minutes 2-3hrs. Sample One Hour Limit 6 ml. (q.10 min.=6 doses/hr.x l ml./dose=6mg 6ml. (9-10 min.=6 doses/hr.x 1mL=1.2mg. Identify the potential complications and side effects of PCA therapy Nursing Responsibilities 1. Patient Education – Teach patients during pre-op period when they are not sedated (e.g.pre-op testing area, physician’s office) and include the following: a. harmful effects of unrelieved pain b. goals of PCA therapy c. use of a pain rating scale to maintain a comfort level d. how to use the PCA pump e. built-in safety parameters of the pump to alleviate fear of overdose f. how adverse effects will be managed g. should be controlled by patient, not designee 2. Patient assessment - Common frequency of assessment: assess with first dose given every 10 minutes, then every 2 hrs. for 8 hrs., then every 4 hrs. 3. Documentation on PCA medication as per agency policy. 4. During assessments, check the settings on the pump for accuracy and the history on the pump for the number of attempted injections and the number that were actually delivered. An excessive number of dosing attempts may indicate medication needs to be increased or changed, prescribed dosing interval should be adjusted or that the patient needs to be reeducated. (Most machines provide print outs of above information). Burgerk rev0108 2 NUR133 Burger CONTINOUS INTRAVENOUS INFUSION (Morphine Drip) 1. High dose morphine is the drug of choice for severe acute and chronic pain (e.g. cancer) because it can be administered by all routes, is metabolized quickly and completely and is economical. 2. When the morphine dose is increased gradually there’s no ceiling on the amount the patient can receive. The dose should be as high as necessary to relieve the pain without causing unacceptable adverse reactions: respiratory depression, sedation, nausea and vomiting, constipation. The patient works up to the high-dose needed for pain relief. 3. Morphine drips are commonly in a concentration of 1 mg in 1 ml. Hourly doses start at 0.8-1.0 mg per hr. and have been used at doses of 15-20 mg per hr. when needed. *Use infusion pump. EPIDURAL ANALGESIA: Injection of narcotics via a catheter directly into the epidural space (between the lining of the vertebral canal and the dura mater of the spinal cord). Advantages 1. Relief of severe pain with low blood levels of the drug, as narcotics act directly on spinal receptors. 2. Less CNS depression. 3. Fewer post-op complications, as patient mobile sooner. Dosing Schedule Single doses: one dose (usually morphine) given after procedure. Respiratory depression can occur for up to 24 hours after dose of morphine. Intermittent doses: narcotic injected into catheter at physician specified intervals. Continuous dosing: continuous infusion of narcotic into catheter using a volume controlled infusion pump for dose accuracy. Patient is commonly cared for on med/surg units and must be monitored closely. Drug Fentanyl Morphine Duramorph Common Drugs and Dosing Opioids *all must be free of preservatives Common Dose Infusion Peak Duration Concentration Rate per hr. In mg per ml 10mcg/ml. 50-100mcg per 10-15 minutes 2-4 hrs. 1mg in 100 ml hr. (5-10 ml. per hr.) 1 mg. per ml. 2-5mg per hr. 30-60 minutes 6-24 hrs. (100 mg in 100 ml) (2-5ml per hr.) *Because of lingering effects of fentanyl and especially morphine, IV access must be maintained for 24 hrs after the epidural analgesia has been stopped and no other narcotics or CNS depressants can be given except as prescribed by the clinician or anesthetist responsible for the epidural analgesia. Burgerk rev0108 3 NUR133 Burger Potential Complications 1. Neurotoxicity from accidental administration and IV medications or solutions into an epidural catheter. Use “epidural catheter” labels for bag of epidural narcotic solution, tubing and pump. Tape all ports. Use no alcohol to clean ports during tubing changes, as alcohol is neurotoxic. (Betadine acceptable). 2. Respiratory Depression Assess for change in LOC: note sedation scale and respiratory rate on epidural analgesia flow sheet every 1 hr., stimulate patient as necessary. Pulse oximetry and apnea monitors as ordered. Have naloxone (Narcan) 0.4mg/ml. (one ampule) available. Administer as per agency policy (e.g. 0.08 mg, in increments to a total dose of 0.4mg until respirations are satisfactory. If too much naloxone is given or it is given too quickly, analgesia will be reversed. 3. Catheter Dislodgement or Migration a. Catheter secured with dressing, no sutures, taped up back and over shoulder. b. Check site as per agency policy for leakage. c. Prevent kinks, pulling on catheter. d. Headache and motor and sensory losses in legs can indicate migration of catheter into subarachnoid space. e. HOB 30 degrees, as medication may migrate towards head. 4. Hypotension Vital signs monitored as per agency policy on epidural analgesia flow sheet. 5. Urinary Retention (side-effect of opiate by any route) Monitor I+O, palpate bladder. Most common in men in the first 24-48 hrs. Less of a problem in post-op patients, as usually have a retention catheter. 6. Prurtis (common side-effect of epidural opiates) Benadryl (Diphenhydramine) 25 mg IV or PO q 6 hr is frequently ordered. 7. Nausea and Vomiting (side-effect of opiates by any route) Frequently managed with: Metoclopramide (Reglan) IV *assess for extra pyramidal reactions Ondansetron Hydrocholoride (Zofran) IV 8. Infection (relatively uncommon) Can occur with permanent, tunneled catheters at suture sites during healing. Those catheters used for management of chronic pain. Assess sites and temperature. Epidural catheter site: Anything more than slight erythema should be reported. Burgerk rev0108 4 NUR133 Burger 9. Break-Through Pain – Toradol (NSAID) frequently ordered by anesthesiologist. 10. Epidural Hematoma More common in patients receiving anti-coagulants. If severe back pain or change in sensory or motor function occurs - call anesthesiologist immediately. 11. Sympathetic Blockade Can be caused by local anesthetics. Assess for vasodilation, hypotension & motor blockade. 12. Constipation CONTINUOUS LOCAL ANESTHESIA – Peripheral nerve Catheter ( On-Q) 1. Excellent postoperative pain control can be achieved by infusing a local anesthetic, subcutaneously into or near the incision site postoperatively, to block nerve conduction. 2. Postoperatively the surgeon inserts a 20-gauge epidural type catheter under the subcutaneous tissue and on top of the fascia or muscle adjunct to or in the wound. A transparent dressing is applied. 3. A long acting local anesthetic such as 0.25% bupivacaine or 0.2% ropicaine is administered continuously in the subcutaneous tissue via an infusion. 4. This method of pain relief has been used in shoulder repair, knee arthroplasty, abdominal hysterectomy, hernia repair and mastectomy. Advantages 1. Provides uninterrupted pain relief 2. Reduces opioid requirements 3. Avoids adverse effects of opioids such as sedation and respiratory depression that are common with conventional administration methods. Nursing Responsibilities 1. Keep catheter site clean and dry and maintain intact dressing to prevent catheter dislodgement. The dressing is not usually changed. 2. Administer proper dose of medication with an infusion pump. Assess for pain relief. 3. Assess for signs of drug toxicity. a. Dizziness b. Tinnitus c. Metallic taste d. Peri-oral anesthesia e. Twitching, tremors 4. Teach patient use of pump and catheter care if he is discharged with continuous local anethesia. Call the patient the day after discharge to assess the quality of pain relief and the presence of adverse effects. Burgerk rev0108 5 NUR133 Burger OTHER PAIN RELIEF MEASURES: Patient Controlled Transdermal System (PCTS) Fentanyl Credit card size system with adhesive to attach to patient’s arm. Medication delivered by Iontophoresis ( an electrical current introduces the medication into the tissue) Fentanyl Transdermal Patch (Duragesic) Drug slowly absorbed producing relatively constant blood levels over a long period. Used for chronic, severe pain. Available in 25, 50, 75 and 100 mcg/hr. patches. Put on flat area of upper torso-can be worn for 72 hrs. At home disposal: flush down toilet so any residual drug not a hazard to children and pets. Patch needs up to 12 hrs to start working; may not reach full effect for 48 hrs Lidocaine Patch Used for neuropathic pain Worn over site of pain for 12 hrs Extended-release preparations Oral preparations taken every 8 hr. (Roxanol) or every 12 hr. (MS Contin). Ordered around the clock. Do not chew, break or crush. Swallow whole. Oral transmucosal Fentanyl (Actig Oralet) via a sucker. Quickly absorbed through oral mucosa. Used for breakthrough pain in clients already taking opioids for chronic pain Oral opioids * Codeine * Oxycodon * Hydrocodone Non-opioids *Acetaminophen (Tylenol) *Nonsterioidal anti-inflammatory drugs (NSAIDS) e.g. Advil, Toradol, Aleve *Cox-2 inhibitors (Celebrex) Adjuvants (given with pain relieving drugs) *Anti-depressants e.g. Elavil *Anticonvulsants e.g. Tegretol, Dilantin *Multi-purpose e.g. Decadron, Ritalin Burgerk rev0108 6 NUR133 Burger TENS (Transcutanenous Electrical Nerve Stimulation) Battery-operated unit with electrodes applied to skin to produce a tingling, vibrating or buzzing sensation in the area of pain. Believed to decrease pain by stimulating nonpain receptors in the same area as the fibers that transmit the pain. Consistent with the Gate Control Theory of Pain, this blocks transmission of pain signals to the brain. Other Non-Pharmacological Techniques: Identify (5) other non-pharmacological pain relieving measures Heat or cold Opioids and the Elderly A number of factors that affect distribution of drugs are altered by age. There is a decrease in muscle and soft tissue mass and an increase in the proportion of body fat. Renal and liver function also decrease in the elderly. As a result, elderly patients may experience a higher peak effect and a longer duration of pain relief from an opioid. Also, drug accumulation and toxicity can occur more often in the elderly. It is therefore best to start with 25% to 50% of the recommended adult dose and titrate upward slowly as needed. *The Dying Patient in Pain Read and reflect upon the following: If we agree that patients have a right to effective pain relief, then nurses have a duty to advocate for that relief and they harm patients when they ignore the duty. Nurses often are not applying the guidelines of the Agency for Health Care Policy and Research even though they are familiar with them. With dying patients, nurses may fear they are hastening death with pain medication. However, patients are harmed when they are left to suffer. When patients die in pain unwillingly, it is an ethical problem. The ANA (American Nurses’ Association) Position Paper states that nurses should not hesitate to use full and effective doses of pain medication for proper management of pain in the dying patient. If death is hastened it is an unintended result of the action. What do you think? Respond with your reflections in the space below: Burgerk rev0108 7 NUR133 Burger Critical Thinking Exercise Read and reflect on the following scenario: “Gram, my head really hurts. Can you push my button?” The teenaged patient was “in and out” of an anesthesia-induced sleep, having just returned from neurosurgery for removal of a lemon-sized blood clot that had been pressing on the base of his brain. He had not been expected to survive the surgery, yet he did, and now, in pain, he was reaching out, seeking the “button” that he knew would offer some relief. A long-term cancer patient, he had become knowledgeable about his care, the medical equipment it required, and his pain management regimen, long before this latest intervention. His grandmother pushed the PCA line, and released the merciful liquid that would bring some comfort to the boy. “Gram, if I fall asleep, will you keep pushing the button?” her grandson asked groggily. “I’m allowed to have the pain med every 10 minutes.” “Sure, honey. I’ll watch the clock and I’ll press every 10 minutes,” promised the caring grandmother, hoping to keep the boy comfortable. Scenario excerpt from: Bezyack, M. (2005). The dangers of PCA by proxy. Nursing Spectrum. September 12,2005. #1 What are the nursing implications inherent in the above scenario? #2 What potential problems/complications (if any) could arise from the above situation? Research and read the following JCAHO Sentinel Event Alert at: http://www.jointcommission.org/SentinelEvents/SentinelEventAlert/sea_33.htm Revise and/or reinforce your answers to questions #1 and #2 based on this reading Burgerk rev0108 8