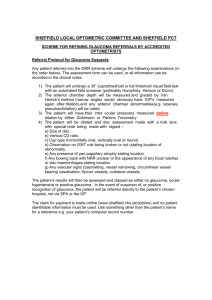
Glaucoma service - referral guidelines for Optometrists
advertisement
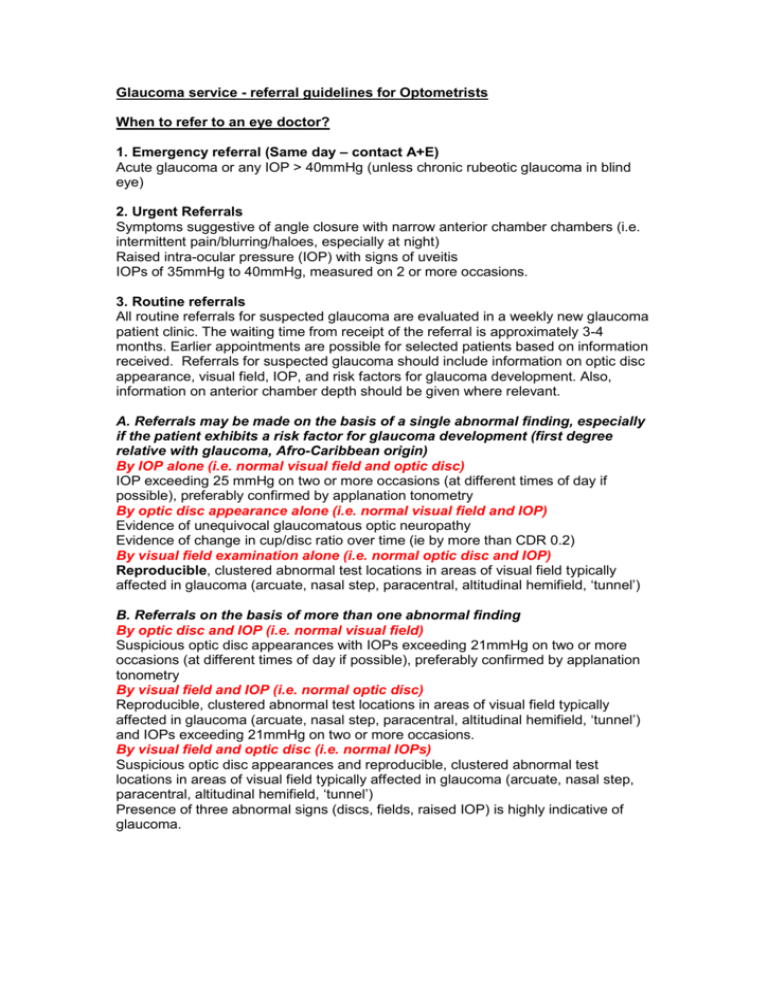
Glaucoma service - referral guidelines for Optometrists When to refer to an eye doctor? 1. Emergency referral (Same day – contact A+E) Acute glaucoma or any IOP > 40mmHg (unless chronic rubeotic glaucoma in blind eye) 2. Urgent Referrals Symptoms suggestive of angle closure with narrow anterior chamber chambers (i.e. intermittent pain/blurring/haloes, especially at night) Raised intra-ocular pressure (IOP) with signs of uveitis IOPs of 35mmHg to 40mmHg, measured on 2 or more occasions. 3. Routine referrals All routine referrals for suspected glaucoma are evaluated in a weekly new glaucoma patient clinic. The waiting time from receipt of the referral is approximately 3-4 months. Earlier appointments are possible for selected patients based on information received. Referrals for suspected glaucoma should include information on optic disc appearance, visual field, IOP, and risk factors for glaucoma development. Also, information on anterior chamber depth should be given where relevant. A. Referrals may be made on the basis of a single abnormal finding, especially if the patient exhibits a risk factor for glaucoma development (first degree relative with glaucoma, Afro-Caribbean origin) By IOP alone (i.e. normal visual field and optic disc) IOP exceeding 25 mmHg on two or more occasions (at different times of day if possible), preferably confirmed by applanation tonometry By optic disc appearance alone (i.e. normal visual field and IOP) Evidence of unequivocal glaucomatous optic neuropathy Evidence of change in cup/disc ratio over time (ie by more than CDR 0.2) By visual field examination alone (i.e. normal optic disc and IOP) Reproducible, clustered abnormal test locations in areas of visual field typically affected in glaucoma (arcuate, nasal step, paracentral, altitudinal hemifield, ‘tunnel’) B. Referrals on the basis of more than one abnormal finding By optic disc and IOP (i.e. normal visual field) Suspicious optic disc appearances with IOPs exceeding 21mmHg on two or more occasions (at different times of day if possible), preferably confirmed by applanation tonometry By visual field and IOP (i.e. normal optic disc) Reproducible, clustered abnormal test locations in areas of visual field typically affected in glaucoma (arcuate, nasal step, paracentral, altitudinal hemifield, ‘tunnel’) and IOPs exceeding 21mmHg on two or more occasions. By visual field and optic disc (i.e. normal IOPs) Suspicious optic disc appearances and reproducible, clustered abnormal test locations in areas of visual field typically affected in glaucoma (arcuate, nasal step, paracentral, altitudinal hemifield, ‘tunnel’) Presence of three abnormal signs (discs, fields, raised IOP) is highly indicative of glaucoma.