Case Study: Improving the Referral and Diagnostic pathway for
advertisement

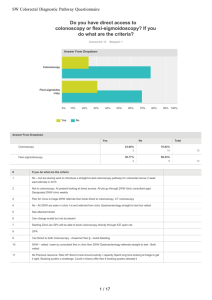
Case Study: Improving the Referral and Diagnostic pathway for Patients with New Colorectal Symptoms across Tayside What was the problem? There were too many ways into the colorectal service, which resulted in inequity of access, confusion and extreme variation in the management of the patient presenting with new colorectal symptoms Inequity of Access Too many ways into the Service Confusion and extreme variation in patient management There can be up to 200 days difference in time between presentation and surgical management depending on which pathway the patient enters Variation in clinical practice Support Staff overwhelmed and Burdened by a paper system which was slow, prone to error and introduced delays in patient management S What improvement tools were used? A Rapid Improvement Event (RIE) using Lean methodology, was held from 23rd- 27th April 2007. A multidisciplinary team of 19 people from Radiology, Endoscopy, Primary Care and NHS Tayside Modernisation Team were freed from their work commitments and were facilitated through the week by Ross International. Having been introduced to the principles of Lean Methodology the team split into groups and visited the three sites in Tayside which receive colorectal referrals. The process was examined from start to finish, mapping every step and any problem experienced at each step. This was also an opportunity to speak to staff and patients about their experiences. A set of Team Goals was developed and the Team set to work designing solutions which were subsequently discussed with staff at all three sites in order to obtain their views and acceptance to the suggested changes. An agreed 12-week action plan was developed allowing progression of the improvements required to develop an enhanced colorectal pathway. Each member of the Team had responsibility for a specific action point. What is the situation now? Protocol based referrals Single route referral management system Combined same day Flexible Sigmoidoscopy / Barium Enema service across the three sites in Tayside. Daily screening of all referrals by a team of Consultant Medical Gastroenterologists Tracking of all referrals through the pathway Patient information at every stage. Information and rapid dissemination of results to General Practioners Generic Tayside patient Information leaflets for patients referred to the colorectal service Standardised Operational Procedures and consistent clinical practice at the point of service delivery across Tayside Daily screening of results with timeous managed clinical decisions. Co-ordinating the patient journey form start to finish Patient receives the right test, at the right time, by the right person NHS Tayside - time from receipt of referral to outcome of examination for routine colorectal patients Routine wait Mean wait 180 160 140 Days 120 100 80 60 40 20 October - December 2007 October - December 2006 Date of receipt of referral What are the benefits to patients? What are the benefits to staff? Information at the point of referral Information on receipt and screening of the referral Information on diagnosis and results Information on cancer pathway Journey happens in a timely fashion Patient knows the length of wait Patient less likely to get lost in the journey Less duplication of work More patient centred environment Less chasing of patient notes and results Ownership and pride in the new process Less disruption and interruptions WHAT ARE THE BENEFITS TO THE ORGANISATION? Improved efficiency and reducing waste Clear patient pathway Referrer informed of progress Improved interface between Primary and Secondary care More appropriate testing Well informed Patients resulting in a reduction in complaints KEY SUCCESS FACTORS Strong Clinical Leadership. Involvement of staff who know the process inside out Passion and Commitment to Improve Senior Management support gave the team the power to push harder and ensure the sustainability of the changes. WHAT WOULD WE DO DIFFERENTLY NEXT TIME? Stick to the original aims and goals Improved communication strategy Ensure a good interface between Primary and Secondary care is vital Ensure a good interface between secondary care clinicians and management Further Information available from: Jill Forbes, Endoscopy Services Manager jillforbes@nhs.net Dr Nigel Reynolds, Consultant Gastroenterologist nigel.reynolds @nhs.net 56 PT 52 PT 48 PT 44 PT 40 PT 36 PT 32 PT 28 PT 24 PT 21 PT 17 PT 13 PT 9 PT 5 PT PT 1 0