H1N1 and Pregnancy
advertisement
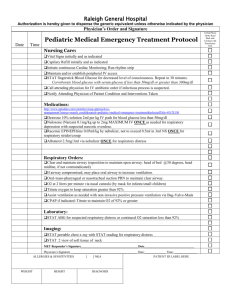
H1N1 and Pregnancy 16/2/11 SPECIFIC CHALLENGES - known high incidence of morbidity and mortality in mother and foetus in H1N1 infection and severe community acquired pneumonia. - multidisciplinary team approach: O&G, NICU, anaesthetics, ICU - planned delivery of foetus (although the teams may have conflicting interests) - indication for intubation: if respiratory failure, hypoxaemia, hypercapnia, exhaustion. - high risk intubation: aspiration, difficult airway, narrow airway, worsening acidosis, cardiac arrest. - difficulties ventilation and complication of ventilation: pneumothorax, tension, cardiac arrest, increased airway pressures, watch intrinsic PEEP, high pressures may reflect raised intra-abdominal pressures. - importance of keeping family members well informed of considerations and likelihood of possible poor foetal outcome as priority will be given to mother’s survival. Mother - physiologic changes of pregnancy: respiratory/cardiovascular, aortocaval compression syndrome. - need to be aware of the changes in blood gas reference values. - need to position carefully -> ideally left lateral position. - pregnancy can worsen respiratory failure– pulmonary congestion, reflux disease, low FRC - reduced respiratory reserve - > decompensation can be rapid - hx of pregnancy: gestational age, singleton?, size of baby / polyhydramnious? - does baby impair mothers state / ventilation - protective ventilation and permissive hypercapnoea -> significant foetal acidosis - safety of various drugs in pregnancy (antivirals, sedatives) Foetus - viable? - lung development possible/bethametasone considered? - effect of medication given to mother: -> -> -> -> Steroids – potential malformations in the fetus if used in the first trimester – cleft lip Benzodiazepines – floppy infant syndrome Opiates- fetal respiratory depression Prolonged paralysis – risk of arthrogyphosis in the fetus - maternal hypercapnia – reduces uteroplacental blood flow + shifts oxyHb dissociation curve in the fetus to the right -> thus impairing fetal oxygenation – fetal monitoring essential - long term maternal hypoxia associated with IUGR Jeremy Fernando (2011) MANAGEMENT Resuscitate A: secure early, RSI, anticipate that it may be difficult and prepare adequately including calling for help B: head up, protective lung strategy, but limiting hypercapnoea if possible (SIMV, FiO2 1.0, TV 6-7mL/kg, low rate, I:E 1 to 3, PEEP 10-15cmH2O titrated to oxygenation, paralyse) C: fluid resuscitate to clinical endpoints, invasive monitoring, vasoactive agents to maintain MAP > 60mmHg, may require Q monitoring, left lateral position Acid-base and Electrolytes - respiratory acidosis -> manipulation of ventilation - metabolic acidosis -> treatment of sepsis Specific Therapy - oseltamivir IV antibiotics to cover possible superinfection steroids for baby planned triggers for delivery -> may require it urgently consideration for adjuncts: iNO, HFOV, (prone and ECMO contraindicated) monitoring for pulmonary and extra-pulmonary complications Jeremy Fernando (2011)