Genetics 1: Meiosis and Recombination
advertisement

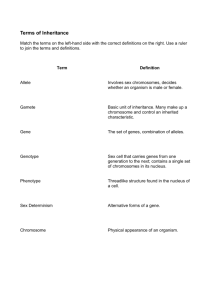
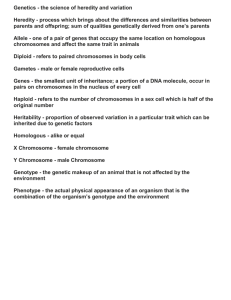
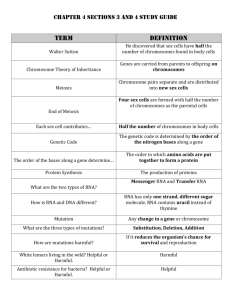
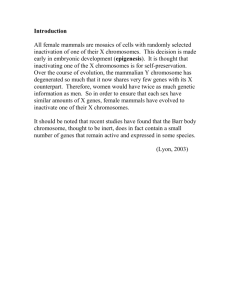
Genetics 1: Meiosis and Recombination Explain the different stages of meiosis I Mitosis Meiosis Occurs in all somatic cells to replicate cells Occurs in germ line cells to produce gametes 2 identical cells are produced 4 non-identical cells are produced (variation) Daughter cells are diploid (2n = 46) Daughter cells are haploid (n = 23) Single one-step process Two-step process: meiosis I and meiosis II Mitosis: somatic cell division Prophase: The chromosomes condense (become shorter and fatter) and become visible The centrioles migrate to opposite poles of the cell Microtubules radiate from each centriole to form the mitotic spindle The nuclear envelope disintegrates Metaphase: The chromosomes become aligned along the equatorial plane of the cell The centriole of each chromosome attaches to a microtubule of the spindle Anaphase: The centromere of each chromosome divides The spindle contracts and the 2 daughter chromatids separate to opposite poles of the cell Telophase: A nuclear envelope develops around each set of daughter chromosomes Cytokinesis: the cell cytoplasm separates to form 2 new diploid daughter cells Meiosis I: reduction division (the chromosome number is halved) Prophase I: The chromosomes condense and become visible Synapsis: homologous chromosomes align directly opposite each other to form bivalents Recombination: crossing over occurs between homologous regions of non-sister chromatids Chiasmata formation: homologous recombinant chromosomes remain attached where crossing over has occurred at chiasmata Metaphase I: The nuclear membrane disintegrates The mitotic spindle is formed The chromosomes become aligned along the equatorial plane of the cell The centriole of each chromosome attaches to a microtubule of the spindle Anaphase I: The spindle contracts and the chromosomes separate to opposite poles of the cell Telophase I: Each set of haploid chromosomes has completely separated to opposite poles of the cell The cell cleaves into 2 new daughter gametes (secondary spermatocytes/oocytes) Explain what occurs at meiosis II Meiosis II: Similar to mitosis Each chromosome exists as a pair of chromatids The chromosomes align along the equatorial plane of the cell The 2 chromatids of each chromosome separate to opposite poles of the cell 2 new haploid daughter gametes are formed (spermatids or ova) Fertilisation: the fusion of 2 haploid gametes to form a diploid zygote Meiosis is important in maintaining the diploid number of chromosomes in the offspring since it produces haploid gametes Draw a diagram of meiosis showing segregation of two pairs of chromosome Explain how recombination of chromosomes occurs Meiosis introduces genetic variation in the offspring: 1. Meiotic recombination: Each chromatid contains DNA portions from each parental homologous chromosome due to recombination during prophase I Each chromosome forms at least one chiasma Small, medium and large chromosomes have 1, 2 and 3 chiasmata respectively 2. Independent assortment of chromosomes: Different bivalents separate to gametes independently of each other Therefore each gamete receives a selection of parental chromosomes Genetics 2: Polymorphism and Inheritance of Variation Define a polymorphism Polymorphism: the occurrence of two or more genetically determined forms (e.g. alleles) in a population in such frequencies that the rarest of them could not be maintained by mutation alone Most polymorphisms are silent (i.e. they do not affect a gene) since they are present in intron DNA Polymorphism: a variant present in a population at a frequency of more than 1% Mutation: a variant present in a population at a frequency of less than 1% Define genetic markers Locus: the site of a gene on a chromosome Allele: an alternative form of a gene found at the same locus on homologous chromosomes Marker: a flag in a genome which is always inherited with a given allele The precise location of the marker within the genome is known Linkage: the association of any known marker with another marker more often than by chance (i.e. in more than 50% of cases) Genetic linkage: 2 alleles are inherited together more often than by chance Genetic linkage often occurs due to physical linkage Physical linkage: 2 loci are situated close together on the same chromosome; therefore the alleles at these loci are inherited together more often than by chance (genetic linkage) Recombination fraction (θ): a measure of the physical distance separating 2 loci The recombination fraction indicates the likelihood of a cross-over occurring between the 2 loci For θ = 0.05: there is on average a 95% chance that the alleles of 2 loci will be inherited together CentiMorgan (cM): the unit of measurement for genetic linkage (not physical distance) If 2 loci are 1 cM apart: a cross-over occurs between them on average in 1/100 meioses 1 cM corresponds to a physical distance of ~ 1 Mb (106 bp) LOD score: a measure of the likelihood of 2 loci being linked LOD score > 3: confirmation that 2 loci are linked (103:1 in favour) LOD score < -2: confirmation that 2 loci are not linked (102:1 in favour) Describe how markers are used to investigate variation Markers: the marker allele will co-segregate with the disease allele Microsatellites: short sequence repeats (2-4 bp) Minisatellites: large sequence repeats (500bp) SNPs: single base changes within an allele Microsatellites Minisatellites Single nucleotide polymorphisms (SNPs) Highly polymorphic • • • Randomly distributed • Easily detectable • Stable Linkage analysis: used to map disease in families • • • • Explain how markers are used to follow inheritance Draw a pedigree Describe variation in humans Describe the inheritance of variation Describe recessive, dominant and X-linked inheritance Describe co-dominant inheritance Modes of inheritance: Autosomal inheritance: determined by an autosomal gene Sex-linked inheritance: determined by an allosomal gene Recessive inheritance: 2 alleles are required for phenotypic expression Dominant inheritance: 1 allele is required for phenotypic expression Co-dominant inheritance: both alleles are expressed (e.g. blood groups) Autosomal recessive inheritance Autosomal dominant inheritance Usually no family history (asymptomatic carriers) At least 1 parent is affected Transmitted by males and females Horizontal transmission: affected individuals are usually in a single generation Vertical transmission: affected individuals are in multiple generations Males and females are affected in equal proportions 25% of the offspring are typically affected 50% of the offspring are typically affected E.g. cystic fibrosis E.g. osteogenesis imperfecta; achondroplasia Compound heterozygote: 2 different defective alleles are present at the same locus Variable expressivity: clinical features may vary Consanguinity increases the autosomal recessive risk Reduced penetrance: abnormal clinical features may be absent in a heterozygous individual X-linked recessive X-linked dominant Transmitted by female carriers to their sons Transmitted by males and females No male-to-male transmission occurs No male-to-male transmission occurs Males are almost exclusively affected Males and females are affected in equal proportions If mother is a carrier: 50% of sons are typically affected and 50% of daughters are typically carriers If father is affected: all daughters are affected If father is affected: 50% of daughters are carriers; normal sons E.g. haemophilia; Duchenne muscular dystrophy If mother is affected: 50% of sons and daughters are affected E.g. hypophosphatemic rickets Females are usually less severely affected than males Genetics 3: Aneuploidies and Other Chromosome Aberrations Describe the normal karyotype, chromosome banding and nomenclature Karyotype: the chromosome constitution of an individual Diploid cells (i.e. somatic cells): 46 chromosomes (22 pairs of autosomes and 1 pair of allosomes) Haploid cells (i.e. gametes): 23 chromosomes Chromosome banding: G (giemsa) banding: used to identify individual chromosomes The banding pattern of each chromosome is specific Idiogram: shows the banding pattern of each chromosome Karyogram: shows each chromosome pair in descending order of size Chromosome nomenclature: Bands are labelled according to the chromosome number, arm and distance from the centromere Each chromosome 2 arms: p (short) and q (long) Each arm regions Each region bands Numbering is outwards from the centromere E.g. 15q32: chromosome 15, arm q, region 3, band 2 Karyotype nomenclature: Male karyotype: 46,XY Female karyotype: 46,XX Chromosome morphology: Metacentric chromosomes: the centromere is located centrally Acrocentric chromosomes: the centromere is located terminally Chromosomes 13, 14, 15, 21 and 22 are acrocentric They often have satellites on their short arms which contain the genes for rRNA Submetacentric chromosomes: the centromere is located in an intermediate position Draw a diagram of a balanced translocation and explain why these are generally not deleterious Common chromosomal abnormalities: 1. Structural: translocations, deletions, insertions, inversions, rings 2. Numerical: aneuploidy, polyploidy 3. Mosaicism: different cell lines (mixoploidy) Translocations: transfer of genetic material from one chromosome to another Translocations of somatic cells are associated with cancer Balanced translocation: the chromosome complement is complete, with no loss or gain of genetic material due to exchange of genetic material between chromosomes Usually the chromosome number remains at 46 and all genetic material is present Therefore the person is generally normal, unless breakage has occurred within a functional gene Unbalanced translocation: the chromosome complement is incomplete, and contains an incorrect amount of genetic material Reciprocal translocation: involves breakage of 2 chromosomes, with subsequent exchange of segments between them to form 2 new derivative chromosomes Robertsonian translocation: involves breakage of 2 acrocentric chromosomes at or near their centromeres, with subsequent fusion of their long arms to form 1 new derivative chromosome The short arms of each chromosome are lost: this is insignificant since they only contain genes for rRNA Draw a diagram showing possible meiotic products from someone with a balanced translocation All genetic material is present in a balanced translocation parent At meiosis: the chromosomes segregate and generate significant imbalance Gametes from a balanced translocation: 50% are unbalanced for a translocation 25% are balanced for a translocation 25% are normal Offspring from a balanced translocation parent may have an unbalanced set of chromosomes This may lead to: Miscarriage Birth of an infant with multiple abnormalities (mentally and/or physically handicapped) Describe how 3 different chromosome aberrations lead to Down syndrome Aneuploidy: the loss or gain of one or more individual chromosomes Non-disjunction: failure of 2 members of a homologous chromosome pair (bivalent) to separate Monosomy: loss of a single chromosome lethal in the case of autosomal monosomy Trisomy: gain of 1 homologous chromosome Usually caused by non-disjunction in anaphase I of maternal meiosis I: the pair of homologous chromosomes fails to separate (May also be caused by non-disjunction during anaphase II of meiosis II: the pair of sister chromatids fails to separate) A disomic gamete is formed: it receives 2 homologous chromosomes If this disomic gamete is fertilised by a normal gamete, a trisomic zygote results Tetrasomy: gain of 2 homologous chromosomes Down syndrome: incidence and clinical features Incidence: 1 in 650 to 1 in 700 Newborn period: severe hypotonia, sleepy, excess nuchal skin (back of the neck) Craniofacial features: protruding tongue, small ears, upward sloping palpebral fissures (below the eyes), bilateral epicanthic folds (inner eyelids), Brushfield spots (on the iris), broad nasal bridge Limbs: single palmar crease, abnormally short 5th finger, wide gap between first and second toes Cardiac: atrial and ventricular septal defects Other: short stature, duodenal atresia (digestive tract) Down syndrome: natural history IQ range: 25-75 Relatively advanced social skills Children are happy and affectionate Adult height: 150 cm Severe cardiac anomaly causes early death in 15-20% of cases Average life expectancy: 50-60 years (omitting cardiac anomaly) Most adults develop Alzheimer’s disease in later life Down syndrome: causes 1. Non-disjunction: trisomy 21 (95% of cases) Trisomy 21: there is an extra chromosome 21 Caused by non-disjunction of the pair of homologous chromosomes 21 in maternal meiosis I This results in the formation of 2 disomic gametes (and 2 nullisomic gametes) If a disomic gamete is fertilised by a normal gamete, the zygote is trisomic for chromosome 21 Causes of non-disjunction: There is a strong association between advancing maternal age and incidence of Down syndrome Maternal age may cause predisposition to non-disjunction since there is an ageing effect on the primary oocyte There may be an age-related reduction in immunological competence: this allows survival of trisomic embryos Radiation Delayed fertilisation after ovulation Genetic control of non-disjunction (as in Drosophila) 2. Translocation: (3% of cases) Caused by a Robertsonian translocation involving chromosome 21 and another acrocentric chromosome A balanced translocation parent carrying the 14q21q translocation can produce a gamete with the translocation chromosome 21 and a normal chromosome 21 13q21q and 14q21q: 10% risk of Down syndrome in offspring 21q21q: all offspring will have Down syndrome 3. Mosaicism: post-zygotic non-disjunction during mitosis (2% of cases) Mosaicism: the presence of 2 or more cell lines with different genetic constitutions, which are derived from a single zygote Chromosome mosaicism: caused by non-disjunction in an early embryonic mitotic division Mosaicism may also be caused by a mutation in a somatic or germ-line cell division Children are less severely affected than the full syndrome since the embryo shows 33% mosaicism for trisomy 21 Describe 2 common autosomal and 2 common sex chromosome aneuploidies Autosomal aneuploidies: Patau syndrome (trisomy 13) and Edwards syndrome (trisomy 18) Incidence: 1 in 5000 to 1 in 10000 Most infants die within the first few days/weeks of life Severe learning difficulties in the rare event of long-term survival Cardiac abnormalities occur in 90% of cases Craniofacial features: severe bilateral cleft lip and palate; cyclopia (in some cases) There is a strong association between advancing maternal age and incidence 90% of cases are caused by non-disjunction: the extra chromosome is usually of maternal origin 10% of cases are caused by mosaicism or unbalanced translocations Sex chromosome aneuploidies: Turner syndrome: 45,X Incidence: 1 in 3000 live female births Features in 2nd trimester: generalised oedema or swelling localised to the neck Features at birth: either normal or may have intra-uterine oedema with puffy extremities, neck webbing, low posterior hair-line, short 4th metacarpels, aorta defect (coarctation in 15% of cases) Normal intelligence Adult features: short stature and ovarian failure Short stature: average adult height is 145 cm without growth hormone treatment Ovarian failure: leads to primary amenorrhea and infertility Treatment: oestrogen replacement therapy (in adolescents) for development of secondary sexual characteristics and long-term prevention of osteoporosis 80% of cases are caused by loss of a sex chromosome in paternal meiosis (45,X) 20% of cases are caused by chromosome mosaicism (e.g. 45,X/46,XX) Klinefelter syndrome: 47,XXY Incidence: 1 in 1000 live male births Childhood features: clumsiness, mild learning difficulties (particularly verbal skills) 10-20 point decrease in verbal IQ Adult features: taller than average, with long lower limbs 30% of adults show moderately severe gynecomastia (breast enlargement) Infertile, with small soft testes: absence of sperm in the semen In adults: increased incidence of leg ulcers, osteoporosis and breast carcinoma Cause: the extra X chromosome arises from the mother or the father (47,XXY) Some cases are caused by mosaicism (46,XY/47,XXY) Males with more than 2 X chromosomes show severe learning difficulties and more marked physical characteristics than Klinefelter men XXX females: 47,XXX Incidence: 1 in 1000 of all females No physical abnormalities 10-20 point decrease in IQ Cause: the extra X chromosome arises from an error in maternal meiosis I Normal fertility Offspring have normal karyotypes Females with more than 3 X chromosomes show high incidence of learning difficulties Phenotype deterioration: the severity of learning difficulties is proportional to the number of X chromosomes present XYY males: 47,XYY Incidence: 1 in 1000 newborn males 2-3% of institutionalised males are XYY due to antisocial behaviour or learning difficulties Most XYY males do not have learning difficulties or antisocial behaviour Emotional immaturity, impulsive behaviour Normal fertility Normal physical appearance and above average stature 10-20 point decrease in IQ Cause: extra Y chromosome arises from non-disjunction in paternal meiosis II or as a post-zygotic event (mitotic error) Describe why sex determination is not solely based on sex chromosome karyotype Sex determination: The sex chromosomes determine the sex of an individual Presence of a Y chromosome male The Y chromosome is much smaller than the X chromosome: it carries only a few functional genes Female gametes: ova carry an X chromosome Male gametes: sperm carry either an X or a Y chromosome Until 6 weeks after fertilisation: the embryonic gonads are undifferentiated Differentiation into a phenotypic male or female occurs 6 weeks after conception: The embryo develops into a female unless the testis-determining factor is present This stimulates the undifferentiated gonads to develop into testes Testis-determining factor: located in the sex-determining region of the Y chromosome (SRY) XX males: the SRY determining gene is translocated from the Y to the X chromosome Infertile phenotypic males (some genes on the Y chromosome are required for spermatogenesis) Karyotype: 46,XX XY females: the SRY determining gene is lost from the Y chromosome by a mutation or deletion Infertile phenotypic females Karyotype: 46,XY Genetics 4: Prenatal Diagnosis of Genetic Diseases Describe the indications for prenatal diagnosis Ideal situation: couples who have a high prior risk of having an abnormal baby should be identified and counselled before a pregnancy Less ideal alternative: couples who have a high prior risk of having an abnormal baby should be identified in early pregnancy to allow them to consider all available prenatal diagnostic options Common indications of prenatal diagnosis include: High risk of aneuploidy: E.g. due to advanced maternal age Family history of a chromosome, single-gene or structural abnormality Increased risk predicted on the result of a screening test E.g. detection of a structural anomaly in the foetus on routine ultrasound screening Describe the use of non-invasive tests: maternal serum screening and ultrasound Ultrasound: Use: prenatal diagnosis of structural abnormalities (e.g. neural tube defects or cardiac anomalies) Limitations: requires specialised expensive equipment and a skilled and experienced operator Down syndrome: Down syndrome foetuses have increased foetal nuchal translucency: increased thickness of the fold of skin on the back of the neck Ultrasound is used to measure nuchal pad thickness to screen for Down syndrome Maternal serum screening: Use: screening for neural tube defects (NTD) and Down syndrome at around 16 weeks gestation Neural tube defects: e.g. spina bifida and anencephaly Detection: by assay of α-fetoprotein (αFP) in the maternal serum If the foetus has an open NTD: αFP leaks into the maternal serum which leads to an elevated αFP level Maternal serum αFP screening: Not 100% sensitive since there is an overlap between the curves for maternal serum αFP levels in normal and affected pregnancies Not 100% specific since factors other than an open NTD may cause elevated levels of maternal serum αFP (e.g. a twin pregnancy) Down syndrome: Detection: by analysing the level of particular biochemical markers in the maternal serum Maternal serum marker Marker level in affected pregnancies vs. normal levels α-fetoprotein (αFP) Reduced level Unconjugated estriol (µE3) Reduced level Pregnancy-associated plasma protein A (PAPP-A) Reduced level Human chorionic gonadotropin (free ß-hCG) Elevated level Inhibin-A Elevated level Down syndrome screening: Risk of Down syndrome increases with: Increasing nuchal translucency (detected by ultrasound) Increasing maternal age Changes in the levels of biochemical markers found in the maternal serum Down syndrome can be screened for in pregnancy by accounting for these risk factors: 1. Maternal age: strong association between maternal age and increasing risk of Down syndrome 2. Maternal serum markers: 3. Nuchal translucency: Down syndrome foetuses have increased foetal nuchal translucency Test Time (weeks) Risk factors accounted for Triple test 14-21 Maternal age, αFP, µE3 and hCG Quadruple test 14-21 Maternal age, αFP, µE3, hCG and inhibin-A NT scan 11-13 Nuchal translucency Combined test 10-13 Nuchal translucency, maternal age, free ß-hCG and PAPP-A Integrated test 1st trimester Nuchal translucency, PAPP-A (1st trimester) and αFP, free ß-hCG, µE3 and inhibin A (2nd trimester) NICE antenatal care guidelines: April 2007: 75% detection and less than 3% false positive Integrated test Combined test Serum integrated test Nasal bones: Poor prenatal diagnostic tool since there is racial variation in nasal bone characteristics Confirmation of Down syndrome requires cytogenetic analysis of foetal material obtained by an invasive procedure (amniocentesis or chorionic villus sampling) Describe the use of invasive tests: amniocentesis and chorionic villus sampling Specific prenatal diagnosis of chromosome and single-gene disorders usually requires an invasive test: this involves obtaining material of foetal origin Amniocentesis: Optimal time: 16 weeks gestation Method: Equipment: 22G needle with stylet Aspire 15-20 ml of amniotic fluid via the abdominal wall under ultrasound guidance Discard the first 2 ml of fluid to remove maternal cells Cytogenetic analysis: Centrifuge the sample to yield a pellet of foetal cells and supernatant fluid Supernatant fluid: used for prenatal diagnosis of neural tube defects by assay of α-fetoprotein Cell pellet: used for chromosome analysis and biochemical or DNA studies The cell pellet is cultured in multiple cultures for 14 days to stimulate cell growth Culture failure rate: 0.5% Maternal contamination is rare Mosaicism in amniotic fluid culture: Mosaicism: it is possible to find 2 or more cell lines with different chromosomal constitutions in amniotic fluid culture This is mainly due to culture artefact; therefore mosaicism must be present in more than 2 cultures for it to be significant Risks and complications: Miscarriage risk: 0.5-1% A late mid-trimester abortion may be necessary if the result is abnormal *Rh negative women get Anti D within 72 hours There is a 1.3% risk of liquor leakage Infection risk: less than 0.1% Chorionic villus sampling (CVS): Optimal time: 11-12 weeks Method: Transabdominal (or transcervical) aspiration of chorionic villi under ultrasound guidance Chorionic villi are derived from the outer cell layer of the blastocyst (i.e. the trophoblast) Maternal decidua must be removed before sample analysis Cytogenetic analysis: A provisional result is possible within 24 hours by direct chromosome analysis of chorionic villi Direct culture of trophoblast cells is possible Culture of chorionic villi: ideal for chromosome analysis Chorionic villi are cultured for 14 days Culture failure rate: 0.2% Mosaicism: 0.5% False negative result: 0.03% Risks/complications: Miscarriage risk: 0.5-2% (CVS is a technically demanding procedure) There is a high risk of limb abnormalities if CVS is performed before 9-10 weeks gestation *Rh negative women get Anti D within 72 hours Advantage: CVS offers first-trimester prenatal diagnosis and therefore an early termination is possible *Rh: blood group antigen which is present in 80% of women Rh sensitisation: in Rh negative women there is an autoimmune response against the foetus Foetal blood sampling: Primary use: to obtain a foetal blood sample to test for foetal anaemia Optimal time: 18 weeks Method: either of the following: Transplacental insertion: into the umbilical cord/placenta Transamniotic insertion: into the intrahepatic vein Transamniotic insertion is preferred since the loss rate is lower Amniocentesis and CVS are preferred for obtaining a sample for chromosome analysis Describe the use of karyotype analysis and FISH for detection of chromosomal abnormalities Karyotype (chromosome) analysis: 1. Prepare a metaphase spread of suitable cells by treating the cells to prevent spindle formation Suitable cells include: chorionic villi and cells from amniotic fluid The cell sample must be cultured for 10-12 days to obtain a sufficient number of cells for analysis Metaphase spread: the preparation of chromosomes during the metaphase stage of mitosis in which they are fully condensed 2. G banding: provides high-quality chromosome analysis Chromosomes are treated with trypsin to denature proteins Chromosomes are stained with Giemsa (DNA-binding dye) which gives each chromosome a characteristic pattern of light and dark bands 3. Count the number of chromosomes present in a given number of cells using metaphase spreads 4. Analyse the banding pattern of each pair of homologous chromosomes in 3-5 metaphase spreads Each chromosome has a specific banding pattern Karyogram: shows each pair of homologous chromosomes in descending order of size Karyotype analysis allows detection of any large rearrangement of DNA without any prior knowledge of the defect (e.g. aneuploidy, translocation or deletion) FISH: fluorescent in situ hybridisation Aim: to detect and localise the presence of specific DNA sequences on chromosomes Principle: a fluorescent single-stranded DNA probe anneals to a very closely related target sequence (i.e. one which shows a high degree of sequence similarity) FISH allows interphase cells to be studied, as well as metaphase cells Advantage: results are obtained rapidly with interphase FISH FISH is used widely for clinical diagnosis of several diseases which cause developmental problems E.g. the common aneuploidy syndromes: trisomy 13, 18 and 21 Chromosome specific fluorescent DNA probes are 99.6% informative FISH method: A fluorescent probe is incubated with the patient sample (interphase or metaphase spread) to allow hybridisation A fluorescent microscope is used to visualise the region where hybridisation has occurred Elective late karyotyping: performed at ~32 weeks Advantages Disadvantages No miscarriage risk May cause iatrogenic prematurity (early birth) Allows antenatal diagnosis and pregnancy termination Termination of pregnancy is late Describe the management options following prenatal diagnosis A compromise must be made between the risk of the potential condition and the risk of the prenatal diagnostic procedure Abortion Act 1967: amended by the Human Fertility and Embryology Act 1990 Pregnancy can be terminated within 24 weeks under one of the following circumstances if it: 1. Puts the life of the mother at risk 2. Poses a risk to the mental and physical health of the pregnant woman 3. Poses a risk to the mental and physical health of the foetus 4. Shows there is evidence of extreme foetal abnormality i.e. the child would be seriously physically or mentally handicapped after birth and during life Management options: Termination of pregnancy Continuation of pregnancy: The multidisciplinary team must: support the parents’ decision, offer continuous ultrasound monitoring and make detailed plans for the following: o Mode of delivery o Monitoring in labour o Neonatal resuscitation o Post-mortem o Postnatal care: e.g. surgical, cardiac, neurological Genetic counselling: The multidisciplinary team must: calculate the risk of recurrence of a genetic disease, offer management strategies for future pregnancies and detail implications related to other family members Describe the use of PCR for mutation detection with examples PCR allows one to amplify a specific, small region of the genome from a patient. This DNA can then be analysed easily for mutations. Advantages: you start with very little DNA - down to 1 cell. Very fast analysis within 1 day. Can be automated. Disadvantage: easy to get contamination. Need to know the precise region you are interested in - you can only amplify about 2 kb at a time. Detection of a CFTR mutation by PCR Allele-specific PCR, also known as amplification refractory mutation system or ARMS test can be used to detect any known point mutation. Use different primers to recognise the normal and mutant sequences. Over 1000 different CFTR mutations have been identified so it is extremely difficult to test for all of them. Generally test for about 5 mutations which make up 80% of all cases. PCR detection of trisomy 21 Use PCR to amplify microsatellites on chromosome 21. If there are three alleles, clearly trisomy 21 is present. If there are two different allele sizes, they would be in a 1:1 ratio in a diploid cell, but a 2:1 ratio in a cell with a trisomy 21. Genetics 5: Genetics of Childhood Diseases Explain the underlying defects for phenylketonuria and other diseases in the same biochemical pathway ‘One gene-one enzyme concept’: Metabolic processes are a sequence of linked steps Each step is controlled by a specific enzyme Each enzyme is coded for by a gene Phenylketonuria (PKU): autosomal recessive disorder of amino acid metabolism Cause: Deficiency of phenylalanine hydroxylase (PAH) PAH: catalyses conversion of phenylalanine tyrosine Symptoms: Phenylalanine accumulates: it is converted into phenylpyruvic acid which is excreted in the urine Tyrosine is deficient: it is necessary for melanin formation (tyrosine DOPA melanin) Reduction in melanin formation: affected children have a fair complexion (often blond hair and blue eyes) Untreated children have severe mental retardation and epilepsy (they often have convulsions) Treatment: Restrict phenylalanine in the diet N.B. phenylalanine is an essential amino acid and cannot be entirely removed from the diet Monitor the blood level of phenylalanine to provide a sufficient dietary quantity of phenylalanine If PKU is detected in early infancy mental retardation (and epilepsy) can be prevented by restricting dietary phenylalanine Diagnosis: Guthrie test (performed in the 1st week of life): tests for elevated blood phenylalanine levels Related disorders: Hypothyroidism: tyrosine thyroxine Alkaptonuria: (tyrosine ) homogentisic acid (in urine) acetoacetic acid ( CO2 + H2O) Albinism: (tyrosine ) DOPA melanin Describe the clinical features and genetic defects in common disorders of carbohydrate metabolism Galactosaemia: autosomal recessive disorder of monosaccharide metabolism Cause: deficiency of galactose 1-phosphate uridyl transferase Galactose 1-phosphate uridyl transferase is necessary for galactose metabolism Symptoms: vomiting, lethargy, failure to thrive and jaundice in the 2nd week of life Complications: mental retardation, cataracts and cirrhosis of the liver Diagnosis: screen for the presence of galactose in the urine Treatment: early diagnosis and feeding infants with milk substitutes which lack galactose and lactose prevents complications Hereditary fructose intolerance: autosomal recessive disorder of monosaccharide metabolism Cause: deficiency of fructose 1-phosphate aldolase Dietary fructose is present in honey, fruit and certain vegetables and with glucose in cane sugar Symptoms: range from minimal to failure to thrive, vomiting, jaundice and convulsions Symptoms present at different ages depending on when fructose is introduced into the diet Diagnosis: screen for the presence of fructose in the urine; enzyme assay on an intestinal mucosal or liver biopsy sample Treatment: dietary restriction of fructose conveys a good long-term prognosis Describe the clinical features and genetic defects in common disorders of steroid metabolism Congenital adrenal hyperplasia (CAH): autosomal recessive disorder of steroid metabolism Cause: deficiency of 21-hydroxylase (90% of patients), 11ß-hydroxylase or 3ß-dehydrogenase Symptoms: ambiguous genitalia; lack of cortisol and aldosterone and excess androgen In newborn females: virilisation of the external genitalia (pseudohermaphroditism) occurs In adolescent males: the increase in androgen production stimulates growth of the phallus ¼ of infants have the salt-losing form of CAH: circulatory collapse occurs in the 2nd week of life Complications: gender identity and assignment of gender are problematic; there may be damaging psychological effects Treatment: replacement cortisol (and fludrocortisone for the salt-losing form); steroid replacement must be increased during periods of stress (e.g. surgery) or recurrent illness Virilised females: may require plastic surgery Describe the clinical features and genetic defects in common sphingolipidoses Sphingolipidoses (lipid storage diseases): inability to degrade sphingolipid, resulting in progressive deposition of lipid/glycolipids primarily in the brain, liver and spleen Tay-Sachs disease: autosomal recessive sphingolipidosis Cause: deficiency of the α subunit of ß-hexosaminidase This leads to accumulation of GM2 ganglioside Incidence: 1 in 3600 among Ashkenazi Jews Symptoms: By 6 months: poor feeding, lethargy and floppiness 6-12 months: lack of developmental milestones (developmental regression) Progressive symptoms: feeding becomes difficult, deafness, visual impairment and spasticity Death often occurs in the 3rd year due to respiratory infection Diagnosis: reduced serum levels of hexosaminidase A Gaucher disease: Diagnosis: reduced glucosylceramide ß-glucosidase activity in white blood cells Symptoms: Type I (adult onset): febrile episodes; limb/joint/trunk pain; a tendency to pathologic fractures; enlarged liver and spleen; mild anaemia Type II (infantile onset): failure to thrive and hepatosplenomegaly (3-6 months); developmental regression, neurological deterioration, spasticity and fits (by 6 months); death in the 2nd year Treatment for type I: symptomatic pain relief; removal of enlarged spleen (since it causes a secondary anaemia due to hypersplenism) Describe the clinical features and genetic defects in common urea cycle disorders Urea cycle: occurs in liver cells 5 step metabolic pathway that removes waste nitrogen from the amino groups of amino acids Ammonia + bicarbonate + 2 ATP urea Enzyme deficiencies in the urea cycle lead to protein intolerance due to accumulation of ammonia in the body Elevated ammonia levels are toxic to the CNS and may lead to coma or death Urea cycle disorders: all autosomal recessive, except OTC deficiency (X-linked) CPSI deficiency OTC deficiency Citrullinaemia: ASS deficiency Argininosuccinic aciduria: ASL deficiency Hyperargininaemia: ARG deficiency Explain the classification of congenital defects Malformation: a primary structural defect of an organ or tissue which results from an inherent abnormality in development E.g. congenital heart abnormalities (ventricular or atrial septal defects), cleft lip and neural tube defects (anencephaly) Malformations involving a single organ generally show multifactorial inheritance: i.e. the defect is caused by the interaction of several genes with other factors Disruption: a secondary structural defect of an organ or tissue which results from external factors disturbing the normal developmental process E.g. amputation of digits when an amniotic band/strand becomes entwined around the digits Extrinsic factors that can disrupt normal development include: ischemia, infection and trauma A disruption is not genetic by definition; genetic factors may predispose individuals to disruption Deformation: a defect involving distortion of a structure resulting from abnormal mechanical force E.g. hip dislocation and mild ‘positional’ talipes (‘club foot’) Causes may include: lack of amniotic fluid (oligohydramnios) or intra-uterine crowding due to twinning or a structurally abnormal uterus Deformations occur late in pregnancy and convey a good prognosis with appropriate treatment since the underlying organ is otherwise normal in structure Dysplasia: a defect involving abnormal of organisation of cells into tissue E.g. skeletal dysplasias: thanatophoric dysplasia is caused by a mutation in FGFR3 This results in short flat bones, a small thorax and a large head Main cause: single-gene defect Effects are usually observed in all parts of the body in which the defective tissue is present There is a high recurrence risk for siblings and/or offspring Sequence: a pattern of multiple abnormalities which result from a single primary factor E.g. Potter sequence: chronic leakage of amniotic fluid or defective urinary output causes oligohydramnios This causes foetal compression which results in squashed facial features, hip dislocation, talipes and pulmonary hypoplasia This usually results in early neonatal death from respiratory failure Syndrome: a consistent pattern of multiple abnormalities which have a known underlying cause E.g. Down syndrome Underlying causes: chromosome abnormalities or single-gene defects Association: the non-random occurrence of multiple abnormalities which cannot be explained by a sequence or syndrome There is a lack of consistency of abnormalities between individuals The underlying cause is generally unknown: it is not usually genetic There is a low recurrence risk for siblings and/or offspring E.g. VATER association: Vertebral, Anal, Tracheo-Esophageal and Renal abnormalities Explain how non-genetic factors lead to congenital abnormalities Genetic causes of congenital abnormalities: Chromosome abnormalities (6%): caused by an abnormality in chromosome number (loss/gain of chromosome material) Single-gene defects (7.5%): caused by a point mutation within a single gene Multifactorial inheritance (20-30%) Neural tube defects (NTDs): e.g. spina bifida and anencephaly Most NTDs show multifactorial inheritance Cause: defective closure of the developing neural tube during the 1st month of embryonic life Severe symptoms Recurrence risk: 4-5% in first-degree relatives in areas where NTDs are common Incidence in the UK is highest in Celtic populations (they may have an adverse susceptibility gene) No single susceptibility genes have been identified for NTDs Polymorphisms in the MTHFR (methylene tetrahydrofolate reductase) gene: may be a susceptibility factor for NTDs Digenic inheritance: an interaction between PAX1 mutations and Pdgfra mutations causes severe NTDs in 100% of double mutant embryos in mice Environmental factors: Teratogen: an environmental agent which can cause a congenital defect by interfering with normal embryonic/foetal development E.g. rubella; thalidomide Potential teratogenic effects of a drug depend upon: timing of drug administration and dosage Low-grade teratogens are difficult to detect since: There is a relatively small number of reported cases There is a relatively high background incidence of congenital defects Many pregnant women take medication at some stage during pregnancy Exhaustive tests are performed before drugs are approved for use by pregnant women Agents which are teratogenic during pregnancy include: vitamin A, alcohol, lithium, tetracycline, warfarin and streptomycin Thalidomide: Formerly used as a sedative Associated with severe limb abnormalities (phocomelia) in babies whose mothers had taken thalidomide during the 1st trimester Critical period for foetal damage: 20-35 days after conception 40% of thalidomide babies died in early infancy due to severe internal abnormalities of the heart, kidneys or GI tract Maternal infections: Rubella: Damages 15-25% of infected pregnancies if the mother is infected during the 1st trimester Symptoms: cardiac defects, cataracts, retinitis, microcephaly Prevention of congenital rubella infection: widespread immunisation by administration of the MMR vaccine in early childhood or the rubella vaccine to adolescent women Cytomegalovirus (CMV) retinitis: Damages 5% of infected pregnancies No immunisation is available against CMV Symptoms: eye defects, deafness, microcephaly Toxoplasmosis: Maternal infection during the 1st trimester: 20% risk of foetal infection Maternal infection during the 2nd and 3rd trimesters: 75% risk of foetal infection No vaccines are available against toxoplasmosis Symptoms: eye defects, deafness, microcephaly, hydrocephalus Genetics 6: Genetic Services within the NHS Describe the aims, methods and practice of genetic counselling Clinical genetics consists of a variety of specialties, for example: Prenatal diagnosis Cancer genetics Dysmorphology: recognition of disorders by looking at clinical symptoms Neurogenetics… Genetic counselling is a branch of clinical genetics Genetic counselling: patients or relatives at risk of developing or transmitting a (potentially) hereditary disorder are advised of: Consequences of the disorder Probability of developing or transmitting the disorder Ways to prevent or ameliorate the disorder Examples: A couple who has had a child with a serious disorder must consider the recurrence risk of the disorder in future children Individuals with a family history of a serious disorder must consider the likelihood of developing the disorder themselves or transmitting it to future generations Common theme in genetic counselling: communication and education which addresses concerns related to the development and/or transmission of a hereditary disorder Steps in genetic counselling: 1. Diagnosis: involves establishing a medical diagnosis, prognosis and possible treatment 2. Risk assessment: involves looking at the mode of inheritance of the disorder and the risk of developing and/or transmitting it 3. Discussion of options: involves discussing the options available for dealing with the risks 4. Communication 5. Long-term contact and support Communication and support: important to allow the individuals concerned to reach their own fully informed decisions 1. Establishing the diagnosis: Establishing an accurate diagnosis involves: 1. Taking a history (family history and medical history) 2. Performing a full examination 3. Undertaking appropriate investigations (including chromosome and molecular studies) 2. Calculating and presenting the risk: This involves: Quantification: calculation of the numerical value of the risk Qualification: conveying the full nature of the risk (i.e. the severity and long-term burden of a disorder) Placing risks in context: this allows the individuals concerned to independently decide the extent of a risk (i.e. if the risk is high or low) 3. Discussing the options: The counsellor must ensure that the individuals concerned are provided with all of the information necessary for them to make an independent informed decision Ignore the risk: if the risk is low/moderate or if the condition is treatable Have no (further) children Adoption Artificial insemination using donor sperm (AID) Use of donor ova Pre-implantation genetic diagnosis Prenatal diagnosis followed by selective termination of pregnancy Consanguinity: Consanguineous relationship: occurs between blood relatives who have at least one common ancestor no more remote than a great-great grandparent Consanguinity presents a problem in genetic counselling: there is an increased risk for an autosomal recessive disorder in future offspring In the offspring of consanguineous marriages: there is an increased incidence of congenital abnormalities and late-onset conditions (i.e. conditions that present later in life) In the offspring of first cousins: the incidence of congenital abnormalities is twice that in the general population (incidence ~3%) Interpretation of standard genetics laboratory reports (cytogenetic and molecular genetic) Parameters governing population genetic screening, current screening programmes and guidelines for the introduction of such screening programmes Criteria for a screening programme: Disease: should have A high incidence in a target population (i.e. the disease should be sufficiently common) Potentially serious effects on health that are amenable to prevention or amelioration (treatment) Test: should be Accurate and reliable Highly sensitive Sensitivity: the proportion of cases that are detected Measurement: determining the proportion of false negative results Highly specific: Specificity: the extent to which the test detects only affected individuals Measurement: determining the proportion of false positive results Programme: should Be offered in a fair and equitable manner and be widely available Involve voluntary participation Be morally acceptable to a substantial proportion of the target population to which it is offered Provide readily-available information and counselling Be relatively inexpensive Screening: involves prenatal screening, neonatal screening and population carrier screening Prenatal screening: (see Genetics 4) Neural tube defects: screening by assay of maternal serum α-fetoprotein and by ultrasound scans Trisomy 21: screening by maternal age, biochemical markers in maternal serum and increased nuchal fold translucency in ultrasound scans Neonatal screening: Widespread newborn screening programmes have been introduced for: PKU, galactosaemia and congenital hypothyroidism Early treatment of these disorders prevents the development of learning difficulties Guthrie test: a blood test which is carried out at 7 days to identify ~10 conditions including PKU Duchenne muscular dystrophy: widespread screening is still not available Cystic fibrosis: national screening is available; early diagnosis allows early treatment which leads to an improved prognosis Population carrier screening: Involves widespread screening for carriers of autosomal recessive disorders in high-incidence populations Disorder Ethnic group with high incidence α-Thalassaemia China and eastern Asia ß-Thalassaemia Indian subcontinent and Mediterranean countries Sickle-cell anaemia Afro-Caribbeans Tay-Sachs disease Ashkenazi Jews Cystic fibrosis Western European Caucasians Summary of genetic services within the NHS: Genetic services within the NHS cover a large geographical area There are ~22 genetic service centres within the UK Regional Genetics Services Clinical and laboratory services Teaching/university hospital services Genetics 7: Population Genetics Describe allele frequencies in a population based on the Hardy-Weinberg Equilibrium Hardy-Weinberg principle: the relative frequencies of the different genotypes remain constant from one generation to the next E.g. in an ‘ideal’ population: there is an autosomal locus with 2 alleles, A and a, which have frequencies of p and q respectively (before reading this example think about what frequency actually means) p+q=1 The frequency of each genotype can be determined by a Punnett square: Male gametes Female gametes A A a (p) (q) AA Aa 2 (p) (p ) (pq) a Aa aa (q) (pq) (q2) p2 + 2pq + q2 = 1 For an autosomal recessive disorder: 2pq: carrier frequency q2: frequency of affected homozygotes Hardy-Weinberg equilibrium: the maintenance of allele frequencies in a large randomly mating population in which there is no disturbance by external factors I.e. dominant traits do not increase at the expense of recessive traits A population is in Hardy-Weinberg equilibrium for a particular genotype if the relative frequencies of each genotype remain constant with frequencies of p2, 2pq and q2 Population: a group of individuals present in the same area Allele frequency: the relative number of alleles at a particular locus within a population External factors disturb the Hardy-Weinberg equilibrium by changing the allele frequencies o Selection for or against a particular genotype o Mutation o Migration (gene flow) o Small population size o Non-random mating: proceeds by 2 mechanisms (1) assortative mating and (2) consanguinity Mutation: If a particular locus shows a high mutation rate: there is a steady increase in the frequency of mutant alleles The introduction of mutant alleles is balanced by the loss of mutant alleles due to reduced reproductive fitness of affected individuals For a population in Hardy-Weinberg equilibrium: these two opposing factors have ~ equal effects Explain founder and migration effects in a population Migration: gene flow Migration and subsequent intermarriage introduce new alleles into a population This leads to a change in the allele frequencies Gene flow: the slow diffusion of alleles across a racial or geographical boundary E.g. B blood group allele: originated in Asia and slowly spread west Small population size: population isolation Random genetic drift: in a small isolated population a particular allele may be transmitted to a high proportion of offspring by chance This leads to a marked change in allele frequency from one generation to the next Founder effects: A small group of people create a new isolated population Some individuals of the group are carriers of a defective allele The defective allele may become established at high frequency in the population Several rare autosomal recessive disorders have a high incidence in small populations due to a founder effect combined with genetic isolation E.g. Hopi Indians in Arizona: high incidence of albinism Affected males do not do farming due to susceptibility to bright light; they stay indoors They have greater opportunity for reproductive activity in the absence of unaffected peers Therefore the relative frequency of the defective allele increases Explain consanguinity and assortative mating Non-random mating: may lead to an increase in the relative frequency of affected homozygotes Assortative mating: The tendency for individuals to chose partners who share characteristics (e.g. height, intelligence, racial origin) E.g. if there is assortative mating among individuals with autosomal recessive deafness, there will be a small increase in the relative frequency of affected homozygotes Consanguinity: Marriage between blood relatives who have at least one common ancestor no more remote than a great-great-grandparent Consanguinity leads to an increase in the relative frequency of affected homozygotes and a decrease in the relative frequency of heterozygotes Explain how selection affects disease occurrence; using two examples explain the basis of heterozygous advantage Fitness (biological/reproductive): the ability of an individual to survive and produce fertile offspring Individuals with advantageous characteristics have increased fitness and are selected for Individuals with deleterious characteristics have reduced fitness and are selected against Negative selection: Individuals with deleterious characteristics have reduced reproductive fitness (i.e. they produce less offspring compared with unaffected control members of the same population) Negative selection: this leads to a gradual decrease in the frequency of the defective allele and hence a reduction in the frequency of affected homozygotes Heterozygote advantage: Carriers of a recessive disease allele have slightly increased fitness compared with unaffected homozygotes Serious autosomal recessive disorders have a high incidence in large populations due to a heterozygote advantage E.g. 1: Sickle-cell anaemia: Affected homozygotes (sickle-cell disease): severely anaemic; persistent ill-health Heterozygotes (sickle-cell trait): immune to malarial infection because their red blood cells undergo sickling and are destroyed if they are invaded by the parasite In areas where malaria is endemic: heterozygotes have increased biological fitness compared with unaffected homozygotes Therefore the relative frequency of heterozygotes tends to increase E.g. 2: Cystic fibrosis: The disease is lethal before reproductive age and affected males are sterile Therefore a gruel decline in the incidence of cystic fibrosis would be expected; this is not the case Speculative advantage for carriers: resistance to a previously endemic gastrointestinal disease Calculate the carrier frequency for a recessive disease Estimation of the carrier frequency of an autosomal recessive disease in H-W equilibrium: Incidence = frequency of affected homozygotes = q2 Carrier frequency ≈ 2×√q2 Calculation of the carrier frequency of an autosomal recessive disease in H-W equilibrium: Incidence = frequency of affected homozygotes = q2 p+q=1 Carrier frequency = 2pq Calculate the risk of having an affected child in a family where a relative has a known disease Genetics 8: DNA Mutations and Genetic Diseases Understand the different consequences of somatic and germline mutations Mutation: a heritable change in the structure/amount of genetic material in an organism Mutations are caused by mutagens or occur spontaneously Mutagens: chemical/physical agents which greatly increase the mutation rate (e.g. ionising radiation, certain chemicals) Spontaneous mutations: occur as a result of errors in DNA replication and repair Somatic mutations: Occur in somatic cells Somatic mutations are not inherited by the next generation Synonymous/silent mutations: no phenotypic effect (i.e. the mutation does not cause a change in the encoded polypeptide) Non-synonymous: there is a phenotypic effect (i.e. the mutation causes a change in the encoded polypeptide) Synonymous mutations occur much more frequently compared with non-synonymous mutations Ageing: may occur due to the accumulation of somatic mutations Cancer: occurs when a mutation stimulates uncontrollable cell division Germline mutations: Occur in germ cells/gametes during gamete formation Germline mutations can be inherited by the next generation once established in the germline They are inherited in a Mendelian fashion Each individual carries a set of mutated genes Understand the genetics of cystic fibrosis and Duchenne/Becker muscular dystrophy as examples of autosomal recessive and X-linked recessive disease Cystic fibrosis: Genetics: autosomal recessive disease High incidence in Western European Caucasians: 1 in 2000 to 1 in 3000 Most common autosomal recessive disease in children of Western European origin This is most likely due to heterozygote advantage (increased heterozygote resistance to enteric diseases) Clinical features: Commonly affected organs: lungs and pancreas Chronic lung disease: caused by recurrent infection which eventually leads to lung failure and secondary cardiac failure Treatment: antibiotics and physiotherapy; heart-lung transplant (for lung and heart failure) Impaired pancreatic function: reduced enzyme secretion due to blockage of pancreatic ducts Treatment: oral supplements of pancreatic enzymes Salty sweat Sticky viscous secretions of the lungs, pancreas and other secretory organs Meconium ileus: perinatal gut obstruction caused by thickening of the meconium Male sterility: caused by congenital bilateral absence of the vas deferens Average life expectancy: ~30 years Mapping of the CF gene: Linkage analysis: allows single-gene disorders to be mapped by studying the co-segregation of genetic markers with the defective disease allele The segregation of a disease is studied over several generations in large families with polymorphic markers from each chromosome Eventually a polymorphic marker will be identified which co-segregates with the disease allele more often than would be expected by chance: i.e. the marker and the disease allele are linked Molecular linkage analysis: lots of nearby markers are used to follow the segregation of a disease This allows the gene responsible for any genetically-determined phenotype to be found since the marker allele which segregates with the disease is positioned near the disease allele on the same chromosome Markers used in molecular linkage analysis include: Restriction fragment polymorphisms (RFPs) Single nucleotide polymorphisms (SNPs) CFTR protein: CFTR (CF transmembrane conductance regulator) gene: codes for the CFTR protein Locus of the CFTR gene: chromosome 7q31 The CFTR protein is an ATP Binding Cassette (ABC) transporter Primary function of the CFTR protein: ATP-dependent chloride channel Normal mode of action of the CFTR protein: When CFTR proteins are activated by cAMP: chloride channels open and Cl- ions leave the cell This stimulates closure of epithelial sodium channels and intracellular Na+ absorption is reduced This reduces the intracellular NaCl concentration Normal mucous is produced Mode of action of the CFTR protein in CF: The CFTR protein does not function Therefore Cl- ions remain inside the cell Na+ ions diffuse into the cell down the electrochemical gradient The intracellular NaCl concentration increases; therefore water moves into the cell down the water potential gradient This results in the secretion of sticky mucous Mutations in the CFTR gene: result in CF There are over 1000 mutations in the CFTR gene which cause CF Mutations in the CFTR gene are predominantly point mutations Mutations include: missense, frameshift, splice-site, nonsense and deletion (rare) Missense mutation: a point mutation which codes for a different amino acid Nonsense mutation: a substitution which results in the generation of a stop codon Frameshift mutation: a mutation (insertion/deletion of 1 or more bases) which changes the reading frame of the codon triplets Mutations in the CFTR gene reduce the functional activity of CFTR proteins In heterozygotes: 1 copy of the CFTR gene is mutated Phenotypic effect: there is no disease phenotype since enough CFTR proteins are made for normal cell function In homozygotes/compound heterozygotes: both copies of the CFTR gene are mutated Phenotypic effect: CF symptoms are present since the mutation significantly reduces normal CFTR protein activity; therefore ion transport is disrupted o Homozygote: the mutations on both alleles are identical o Compound heterozygote: the mutations on each allele are different Different classes of CFTR gene mutations have different effects on CFTR gene expression (i.e. different phenotypic severities) Phenotypic severity: depends on the functional activity of CFTR proteins CFTR protein activity: < 3%: severe CF (characterised by male sterility, lung disease and impaired pancreatic function) 3-8%: mild CF (characterised by male sterility and lung disease) 8-12%: mildest CF (characterised by male sterility) ∆F508: the most common CFTR gene mutation; it is caused by a missense mutation It prevents the CFTR protein from being transported from the ER to the cytoplasmic membrane Homozygotes for the ∆F508 mutation have severe CF Clinical applications and future prospects: Prenatal diagnosis is offered for CF No curative treatment is available for CF yet Symptomatic treatment: supplements of pancreatic enzymes; physiotherapy; antibiotics; heart-lung transplant Experimental treatment: drugs which traffic the ∆F508 CFTR protein, activate residual mutated protein and inhibit Na+ reabsorption; gene therapy Functional effects of mutations on a protein: Loss-of-function mutations: Consequences: either reduced activity of the protein or complete loss of the protein Haploinsufficiency mutations: loss-of-function mutations in the heterozygous state in which half normal levels of the protein result in phenotypic effects; result in autosomal dominant disorders Gain-of-function mutations: Consequences: either increased levels of gene expression or development of a new function(s) of the protein (e.g. toxicity) Gain-of-function mutations: result in dominant disorders Huntington disease: autosomal dominant disease Symptoms: late onset, neurodegenerative disease which leads to premature death The mutation in Huntington disease: trinucleotide expansion Cause: expansion of a CAG (polyglutamine) repeat sequence (i.e. large CAG repeat sequences) CAG codon: codes for glutamine CAG trinucleotide repeat sequence: codes for huntingtin Huntingtin: expressed in cells of the CNS; unknown function Expansion of the CAG repeat sequence: results in aggregation of huntingtin in the CNS Anticipation: expansion of the triplet repeat sequence increases in subsequent generations Therefore autosomal dominant diseases tend to manifest at an earlier age and/or increase in severity in subsequent generations Repeat expansion: causes the age of onset to decrease and penetrance to increase I.e. the longer the CAG repeat sequence, the earlier the onset of disease and the more likely the onset of disease (Other diseases involving repeat expansion include: fragile X, fragile 16 and myotonic dystrophy) Duchenne muscular dystrophy: Clinical features: severe progressive myodegenerative disease At birth: clinically normal At 3-5 years: slowly progressive muscle weakness- difficulty in running and climbing stairs At 11 years: most patients have to use a wheelchair due to severe proximal muscle weakness Average life expectancy: ~18 years Cause of death: cardio-respiratory failure due to intercostal and diaphragm muscle weakness and due to respiratory infection Prognosis: respiratory care and assisted respiration allow survival into late 20s Becker muscular dystrophy (BMD): milder condition than DMD; age of onset ~11 years; much longer life expectancy Muscle histology in DMD-affected individuals: There is a variation in the size of muscle fibres Necrosis of muscle fibres occurs followed by phagocytosis of necrotic (dead) fibres In early stages: active regeneration of muscle occurs to replace/repair lost/damaged fibres In later stages: the replication capacity of muscle stem cells is exhausted; muscle fibres are replaced by fat and connective tissue (pseudohypertrophy) Genetics: X-linked recessive disease Incidence of DMD: 1 in 3500 DMD gene: DMD (or dystrophin) gene: codes for dystrophin; largest known human gene Locus of the DMD gene: Xp21 Predominantly expressed by 3 promoters in skeletal and heart muscle and in the brain Dystrophin: Size: 427 kDa Location: at the cytoplasmic side of the muscle membrane Structure: dimer composed of 4 domains (actin-binding domain, central and rod domain, cysteine-rich domain and –COOH terminal domain) Function: links intracellular actin with extracellular laminin via dystroglycan (DGC) Mutations in the DMD gene: result in DMD or BMD Mutation rate: 1 in 10,000; 1/3 of DMD cases are caused by a new mutation 2/3 of mutations: result from deletions of all or part of the DMD gene Deletions (and duplications) arise due to unequal crossing over during maternal meiosis 1/3 of mutations: result from point mutations Point mutations arise due to an error in DNA replication during paternal meiosis Deletions in DMD/BMD: whole exons are removed and the flanking exons are spliced together; therefore a functional protein may be produced if there is an in-frame fusion of exons DMD mutations: deletions disturb the translational reading frame; this results in complete absence of dystrophin or production of non-functional dystrophin BMD mutations: deletions do not alter the reading frame since there is an in-frame fusion of exons; there is a reduction in dystrophin production which has residual function Understand how different mutations are associated with different disease severities in both diseases Understand the concept of X-inactivation Male and female cells have the same level of expression of X-linked genes because each female cell has one active and one inactive copy of the X chromosome X-inactivation: Occurs during embryonic development (~1000 cells) One X-chromosome is inactivated in each cell: this exists as a Barr body Thereafter the same X chromosome remains inactivated in all subsequent daughter cells X-inactivation is usually random: i.e. there is an equal chance of either of the two X chromosomes in the cells of a heterozygous female being inactivated Skewed inactivation: abnormal X chromosomes are usually preferentially inactivated In manifesting heterozygotes: X-inactivation is skewed towards the normal X chromosome Clinical manifestation: carrier females who are manifesting heterozygotes show symptoms of the disorder Homozygous females: XmXm Generally show the same phenotype severity as affected males Female carriers: XmX Female carriers are usually asymptomatic since there is either random inactivation or skewing of Xinactivation towards the abnormal X chromosome E.g. haemophilia A and B; enzyme deficiency diseases (G6PDH deficiency, OTC deficiency) Manifesting heterozygotes: show the disease phenotype since there is skewing of X-inactivation towards the normal X chromosome Female-DMD carriers: Random inactivation: the normal X chromosome is inactivated in ~50% of cells Muscle fibres are multinucleate; therefore there is no clinical phenotype as long as 1 nucleus expresses the normal dystrophin gene Manifesting heterozygotes: the active X chromosome in most of the cells is an abnormal X chromosome; therefore clinical manifestation occurs Understand the importance of genetics for diagnosis and treatment of genetic disease and disease caused by genetic factors Genetics 9: The Genetics of Complex Traits Monogenic inheritance: controlled by a single gene Single-gene disorders: result from 1 mutated gene All affected individuals have the mutated gene The gene product is either defective or absent Polygenic inheritance: controlled by many genes Phenotype expression is determined by many genes (polygenes) at different loci Each gene involved exerts a small additive effect: i.e. the effects of the genes are cumulative Polygenes generate a normal distribution (e.g. height, body mass, IQ) Normal distribution: a symmetrical bell-shaped curve distributed evenly about a mean Polygenic inheritance is the genetic component of multifactorial inheritance Multifactorial inheritance: controlled by the combined effects of many genes (polygenes) and environmental factors Multifactorial disorders: not caused by a single gene Threshold effect: there is a non-linear relationship between the number of genes and expression of the disease phenotype I.e. a threshold exists above which the abnormal phenotype is expressed Low penetrance: genetically predisposed individuals may not actually be affected by the disorder Epistasis: genes at different loci interact with each other to amplify the genetic signal Multiple genes give the potential for a continuously variable phenotype since the phenotype is determined by the interaction between genes and the environment Disease susceptibility genes: Disease susceptibility genes: polymorphic alleles which may function slightly differently Genes promote susceptibility to a disease; they do not code for a defective protein Combination of susceptibility genes gives predisposition to a disease Predisposition is caused by the number of interacting genes, not by a specific combination of genes Environmental factors trigger the disease (e.g. viral infection, diet) Disease may develop only on exposure to certain environmental factors (e.g. smoking) Demonstration of the genetic component of a complex trait: Population/migration studies: Migrants moving from a population with low incidence of a particular disease to one with a high incidence: If the incidence of the disease in the migrant group rises: environmental factors are more significant to the cause of disease If low incidence of the disease is maintained in the migrant group: genetic factors are more significant to the cause of disease Family studies: If there is a higher frequency of disease in relatives of an affected individual than in the general population, this suggests that there is genetic susceptibility to the disease Families share a common environment; therefore family studies cannot prove genetic susceptibility λs: the ratio of the risk to siblings of patients to the population incidence The greater the λs value, the greater the contribution of genetic susceptibility to the disease Twin studies: Comparison of the frequency of a disease between monozygotic (identical) and dizygotic (non-identical) twins: Concordance: either both members or neither member of a pair of twins is affected If monozygotic twins have higher concordance rates than dizygotic twins: genetic factors are more significant to the cause of disease If monozygotic and dizygotic twins have similar concordance rates: environmental factors are more significant to the cause of disease Adoption studies: Comparison of the frequency of a disease in individuals who remain with their biological parents with those who are adopted out of their biological family If frequency of disease is in adopted individuals is similar to their biological parents: genetic factors are more significant to the cause of disease If frequency of disease in adopted individuals is similar to their adoptive parents: environmental factors are more significant to the cause of disease Association studies: (case-control study) Comparison of the frequency of a particular polymorphic allele in an affected patient population with that of a healthy, control population: If the frequency of the polymorphism is significantly different in the 2 populations: this provides evidence for a positive or negative association Candidate gene: a gene which is thought to play a role in the disease Factors which influence choice of the candidate gene: Function Location Expression The control population must be carefully selected to control for the affected patient population: this allows the difference in allele frequency in the 2 populations to be attributed to disease Control factors include: Age Sex Ethnicity Environment E.g. HLA histocompatibility complex on chromosome 6: There is a strong HLA association between ankylosing spondylitis and the B27 allele 98% of patients with ankylosing spondylitis have the B27 allele vs. 5% of controls Therefore the following inferences can be drawn: o There is a strong association between having the B27 allele and developing ankylosing spondylitis; however… o The B27 allele is not an absolute requirement for developing ankylosing spondylitis o The B27 allele does not cause disease on it is own Autoimmune disease: involves development of an immune response against the ‘self-antigen’ The immune response cannot be resolved since the self-antigens are always present Therefore there is a continuous immune response (which leads to inflammation) Many autoimmune diseases are linked to a particular locus Therefore family history of a disease is not only relevant for that particular disease since another autoimmune disease may be linked to the same locus as the disease which has a family history