USimaging(NA)3
advertisement

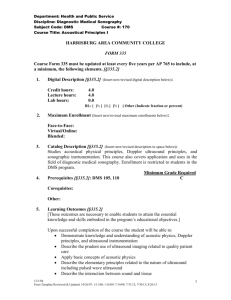
Ultrasound Imaging
Prepared by Dr. Ali Saad,
Department of Biomedical Technology,
College of Applied Medical Sciences,
King Saud University.
1
contents
1-Introduction to ultrasound
Overview
Some Advantages of US
Ultrasound is used for most field of imaging
History
2- Basic Ultrasound Physics
Sound Wave
Wave equation
Speed of Sound
Sound propagation media
Compressions, Rarefactions and Acoustic Pressure
Interaction of Ultrasound with tissue
Transmission
Reflections
Refraction
Scattering
Attenuation
Amplitude and Intensity
Wave Interference
Acoustic Impedance
3- Doppler Ultrasound physics
The Doppler Effect
Doppler Equation
Continuous wave doppler
Transducer design
CW Doppler unit
Pulsed wave Doppler
PW vs. CW Doppler
4-Directional detectors -Discrimination of the direction
of flow
Overview
single sideband detector
Offset carrier demodulation -Heterodyne detector
Quadrature phase detector
Autocorrelation method
2
5-Basic of Ultrasound Instrumentation
Overview
Piezoelectric properties
Piezoelectric Transducer Construction
Transducer Characteristics
Transducer Beam Characteristics
Focusing
6-Static Image Generation Using Ultrasound
Generating an A-Mode scan
Time gain compensation
Generating a B-Mode Image
7- Real Time Imaging (RTI)
Principle of RTI
Electronic Array scanner
Electronic focusing
Phased array
Mechanical scanner
Generating an RTI image
8- Doppler imaging
Generating a Doppler Image history
Duplex Scanner
Color Flow Imaging
Power Doppler or Angio Mode
Time Domain Correlation
9-M-Mode imaging
principle
Generating a 3D Image
10- artifacts in Ultrasound imaging
Some useful definitions In Diagnostic US Physics
Some useful definitions in Doppler US
3
1-Introduction to ultrasound
Overview
The field of medical ultrasound has expanded rapidly over the past decade.
Although the basic physic principle are unchanged. Significant advances in
ultrasound instrumentation have led to increase clinical use of diagnostic
ultrasound. Motion imaging techniques, particularly real time and Doppler have
advantages over B-Mode scanners. Duplex Scanners that incorporate real-time
imaging with Doppler capabilities are now in common use diagnostic US.
Computer processing techniques have enabled the superimposition of blood flow
images with real time images.
Some Advantages of US
Non-invasive imaging - Most ultrasound scans are performed on the
surface of the body.
Safe - Ultrasound uses non-ionizing energy. Non-ionizing energy does not have
sufficient energy to remove electrons from the outer shells of atoms.
Diagnostic ultrasound has been in use since the late 1950's . No confirmed
adverse biological effects on patients resulting from this usage have ever been
reported. Although no hazard has been identified that would preclude the prudent
and conservative use of diagnostic ultrasound in education and research,
experience from normal diagnostic practice may or may not be relevant to
extended exposure times and altered exposure conditions. It is therefore
considered appropriate to make the following recommendation:
In those special situations in which examinations are to be carried out for
purposes other than direct medical benefit to the individual being examined, the
subject should be informed of the anticipated exposure conditions, and of how
these compare with conditions for normal diagnostic practice. "
Real-time imaging - Ultrasound provides a continuously updated image
or "live" image.
Mobile - Ultrasound systems are portable.
Cost effective - The cost of an ultrasound scan is inexpensive compared
to x-ray or CT. The cost of an individual ultrasound unit is also inexpensive
relative to other diagnostic imaging equipment.
4
Main differences between Ultrasound and X-rays
Diagnostic Ultrasound
X-rays
(radiology)
wave type
longitudinal mechanical waves
electromagnetic waves
transmission
requirements
elastic medium
No medium
generation
stressing the medium
accelerating electric charges
velocity
depends on the medium through
which it propagates
It is relatively constant:
299,792.456.2 m/s
similar waves
seismic, acoustic
radio, light
Ultrasound is used for most field of imaging
General radiology
Superficial organs
o Breast
o Testes
o Scrotum
o Prostate
o Thyroid
Obstetrics
Gynecology
Urology
Biopsies
Vascular
Cardiology
Musculoskeletal
History
First use of diagnostic ultrasound
Dr. Karl Dussik, a psychiatrist, at the hospital in Bad Ischl, Austria was the first
person publishing a medical use of diagnostic ultrasound.
He was trying to locate brain tumors with a new method consisting of an
ultrasound emitter at one end and an ultrasound receiver at the other. The
patient stayed between the two devices. He measured the ultrasound beam
5
transmission through the patient's head. The outbound ultrasound beam power
was known and he calculated the receiving power, defining ultrasound
attenuation and reinforcement. He also tried to visualize the cerebral ventricles
by measuring the ultrasound beam modification through the head. Dr. Dussik
published his technique in 1942 with the name of "Hyperphonography of the
Brain."
1916 sound is used in war in order to locate submarines
1952 Mechanical transducer with B_mode scanners.Pulse echo imaging with
direct contact with patient.
1960 real time imaging
1961 A mode scan for gynecological purpose
1968 phase array scanners
1970 doppler imaging endocavity transducer
1974 first digital scan converter
1980 duplex mode systems B-mode and Doppler
1981 doppler color flow imaging
1996 3D imaging,
2000 4D imaging
6
2- Basic Ultrasound Physics
Sound Wave
Sound is a mechanical energy transmitted through a medium. Periodic changes
in the pressure of the medium are created by force acting on the molecules
causing them to oscillate about their mean or average positions, oscillation could
be longitudinal or transverse it depend on the medium. The periodic changes in
pressure when vibrating molecule interact with neighbor molecules are convoyed
from one molecule to another. The term propagation describe this transmittal to
a distant region from the sound source. As the sound waves are of mechanical
nature they can propagate through different types of medium except the vacuum.
Frequency of a wave is the number of vibration that a molecule do in one
second. Sound wave having frequencies that a human can hear, the range of
sound wave is [20 Hz to 20Khz]
Ultrasound waves is defined as high frequency sound waves they are grater than
20khz, which human cannot hear. Sound ultrasound have the same physical
properties.
Longitudinal wave
a waveform transmitted through a medium where the particles of the medium
oscillate in the direction of the wave propagation. Sound propagates as
longitudinal waves. A longitudinal wave is produced when a vibrator, e.g. a
piezoelectric crystal in an ultrasound transducer, transmits its back and forth
oscillation into a continuous, elastic medium (Fig. 1). The particles of the medium
are made to oscillate in the direction of the wave propagation, but are otherwise
stationary. The wave propagates as bands of compression and rarefaction. One
wavelength is the distance between two bands of compression, or rarefaction.
Maximum compression corresponds to maximum pressure (Fig. 1, bottom).
Longitudinal wave, Fig. 1The propagation of the first three bands of compression (1-3) are shown. The longitudinal wave
at the bottom is also shown as a sinusoidal curve.
Wave equation
The wave equation can be expressed as follow :
7
A=A0Sin(2ft).
Where A is the amplitude at time t, A0 is the peak amplitude and f is the
frequency.
Period is the time taken by one cycle of the wave is defined by T=1/f.
Wavelength is the distance taken by a cycle of the wave which is defined by
=T.C,
where T is the period of the wave and C is the velocity of the wave in the
medium.
Frequency and Resolution (axial resolution)
This is for linear array transducers with parallel beams
MHz
Axial
resolution
Lateral
resolution
Resolution %
3.0
1.1 mm
2.8 mm
35.89%
4.0
0.8 mm
1.5 mm
60.86%
5.0
0.6 mm
1.2 mm
77.77%
7.5
0.4 mm
1.0 mm
100%
10.0
0.3 mm
1.0 mm
107.69%
For harmonic imaging the input frequency doubles the output
frequency (it works just for low frequencies)
Speed of Sound
The speed at which a wave propagates through a medium is called acoustic
velocity ( C ). The velocity depends on the density and compressibility of the
medium.
The sound is inversely proportional to the square root of the compressibility,
the propagation speed of a sound wave (e.g. ultrasound) through a medium. The
propagation speed is determined by the physical properties of the medium, and
is independent of the (ultra)sound frequency. The major parameters affecting the
speed of sound (c) are the elasticity (K) and density () of the medium, their
relationship being c = (K/). High elasticity implies large elastic forces between
the particles of the medium and a high resistance against compression (low
compressibility). Speed increases with decreasing compressibility (increasing
elasticity) because less compressible media have more densely packed
molecules which need to move only a small distance before their motion is
transmitted to the neighboring molecules. Speed decreases with increasing
density because dense materials tend to have large, heavy molecules that are
difficult to start and stop in the rhythmic motion involved in the propagation of
sound. Tissues may be considered liquids, and in liquids, compressibility and
8
density are generally inversely proportional. The speed of sound is therefore very
similar in all tissues, the average speed in human soft tissue being approximately
1 540 m/s.
Velocity of sound in some Biological Materials
Velocity of sound in some Biological Materials
Material
Velocity of Sound (m/s) Impedance (Rayl x 10 -6)
Air
330
0.0004
Fat
1450
1.38
Water
1480
1.48
Average Human Soft Tissue
1540
1.63
Brain
1540
NA
Liver
1550
1.65
Kidney
1560
1.62
Blood
1570
1.61
Muscle
1580
1.7
Lens of eye
1620
NA
Skull Bone
4080
7.8
Sound propagation media
Ultrasound propagation properties
Velocity of sound in “soft tissue” is nearly constant = 1540 m/sec.
Velocity of sound in bone and air differ greatly from soft tissue.
Velocity = Frequency x Wavelength
“Ultra”sound implies f > 1 MHz
Wavelength = Velocity/Frequency
Wavelength < 1.5 mm
Compressions, Rarefactions, and Acoustic Pressure
A term used for all forms of volume reduction. Ultrasound travels through tissue
as a longitudinal wave with bands of compression and rarefaction.
9
In X-ray imaging, compression methods are used to reduce the irradiated
volume. Mechanical compression of the part of the body that is irradiated serves
two purposes: 1) the exposure can be reduced, thereby minimizing exposure
time and patient dose, and 2) reduction of the volume being irradiated, giving
less scattered radiation and better image contrast
Interaction of Ultrasound with tissue
Transmission
Ultrasound transmission properties
Frequency of ultrasound remains constant during propagation.
Wavelength changes in proportion to changes in the velocity of sound.
Sound “bends” at interfaces between tissues with different velocities of
sound.
Bending increases as deviation from “normal” incidence increases.
Intensity of ultrasound decreases during propagation, measured in dB/cm.
Transmission: muscle/fat
vmuscle = 1585 m/s
vfat = 1450 m/s
10% Change in wavelength
Reflections
Reflection ,in ultrasound, is the return of an ultrasound wave from an interface between
two media. Reflection of ultrasound is dependent on a difference in acoustic
impedance between the two media and also on the size and shape of the reflector.
When the interface is smooth and large as compared to the ultrasound wavelength (e.g.
the surface of an organ), specular reflection may occur. Specular reflection follows
the law of reflection stating that the angle of incidence is equal to the angle of
reflection. When the incident ultrasound is perpendicular to the reflecting interface, i.e.
when the angle of incidence is 0, the fraction of ultrasound intensity being reflected (R) is
given by the formula:
R = ((Z - Z2) / (Z + Z2))2
where Z and Z2 represent the acoustic impedances of the two tissues on each side of the
interface. The reflection coefficient (R) is in the order of 0.01 (1%) at soft tissue
interfaces (0.011 for fat/muscle), 0.410 at skull/brain interfaces, and 0.999 at muscle/air
10
interfaces, i.e. practically total reflection. Generally, perpendicular, specular reflection
gives the strongest echoes (Fig.1, a).
Reflection, Fig. 1:Examples of different kinds of reflection of ultrasound.
When the ultrasound incidence is non-perpendicular, the above formula no
longer applies. Pure specular reflection which is not perpendicular will not give
rise to any detectable echoes, the reflected ultrasound being directed at an angle
to the ultrasound beam (Fig. 1, b). Depending on the acoustic properties of the
two tissues at an interface, i.e. their density and ultrasound propagation velocity,
reflection may or may not occur.
Small structures with sizes in the order of the ultrasound wavelength, e.g. the
interior of organs or rough surfaces, will cause diffuse reflection, with reradiation
of the ultrasound in several directions (Fig. 1, c). The detectable echoes will
therefore be relatively weak. The backscattering of ultrasound from blood is
referred to as Rayleigh Tyndall scattering. The "reflectors" in blood are point
scatterers, much smaller than the ultrasound wavelength, reradiating the
ultrasound as spherical wavelets (Fig. 1, d).
Specular reflection
reflection of a waveform from a smooth surface, i.e. a surface having irregularities that
are much smaller than the wavelength of the waveform. Light is reflected from a mirror
as specular reflection. In ultrasound, specular reflection may occur from smooth
structures such as the surface of solid organs and vessel walls.
Diffuse reflection
scattered, non-specular reflection of ultrasound caused by rough surfaces or irregular
boundaries where the surface or boundary variations are of the same order of magnitude
or larger than the ultrasound wavelength.
Refraction
In ultrasound, a change in direction and velocity of a transmitted ultrasound beam after
having crossed the interface between two media. Refraction requires non-perpendicular
incidence of the beam, and different propagation speeds in the two media. The change in
direction is caused by a change in wavelength to accommodate the change in speed (Fig.
1). A difference in acoustic impedance does not cause refraction if the propagation
11
speeds of the two media are equal. At perpendicular incidence, there is no change in
direction, even though there may be a change in speed.
Refraction, Fig. 1The wavelength of the refracted ultrasound beam is shorter than that of the incident
beam due to a decrease in propagation speed
The angle of refraction is determined by the propagation speeds of the two media,
according to Snell's law:
sin θt = sin θi·ct/ci
where θt is the angle of refraction (or transmission), θi is the angle of incidence, ci is the
propagation speed of the incident medium, and ct is the propagation speed of the
transmitting medium. ci/ct is called the refractive index of the transmitting medium with
respect to the incident medium.
Note that the laws of refraction are common to all kinds of waves, including
electromagnetic waves at all frequencies.
Scattering (Rayleigh Tyndall scattering).
Rayleigh, and Tyndall discover the backscattering of ultrasound from blood.
The echoes detected from blood (e.g. in Doppler ultrasound) are created through
interference between scattered wavelets from numerous point scatters (small
homogeneities in the red blood cell concentration). The intensity of the
backscattered echoes is proportional to the total number of scatters, which
means that the echo amplitude is proportional to the square root of the total
number of scatters (see intensity of sound). At normal blood flow, the number of
point scatters in blood is proportional to the number of red blood cells (i.e. the
amount of blood). When blood flow is turbulent, or accelerating fast (e.g. in a
stenosis), the number of homogeneities in the red blood cell concentration will
increase, thus giving rise to stronger echoes than can be accounted for by
merely the amount of blood. The intensity of the backscattered ultrasound is also
12
proportional to the fourth power of ultrasound frequency. Doubling the ultrasonic
frequency makes the echoes from blood 16 times as strong. (On the other hand,
higher frequency ultrasound suffers from higher attenuation in the tissues.)
Attenuation
The Process by which radiation loses power as it travels through matter and
interacts with it is called attenuation. Beam attenuation is the basis of the
contrast observed in all X-ray based imaging methods, and it is at the basis of
the varying penetration depth of sound waves in ultrasonography
Wave Interference
Interference is the interplay of two or more waveforms. When two or more waves
with equal frequency and wavelength interfere, a new wave is created whose
amplitude at any point in time and space is the sum of the amplitudes of the
original waves at the same point in time and space. When two waves of equal
frequency are in phase, their amplitudes will always be in the same direction, and
the waves will combine to produce a stronger one. This is called constructive
interference. If the waves have opposite phases, i.e. if the phase difference is
180, their amplitudes will always be in opposite directions and their sum is a
weaker wave. This is destructive interference. Two equally strong waves (of the
same amplitude) that are 180 out of phase will cancel each other out.
Constructive and destructive interference play a role in the production of
ultrasound beams and in the backscattering of echoes from blood in Doppler
ultrasound applications (Rayleigh Tyndall scattering).
Amplitude and Intensity
The intensity of sound is the acoustic power per unit area, measured in W/m 2.
The intensity is determined by the amplitudes of the particles conducting the
waves; the larger the amplitudes of oscillation, the higher the intensity. The
actual relationship is I = p2/2z, where I is intensity, p is pressure amplitude, and z
is acoustic impedance. Acoustic energy (joule) per unit time (second) and unit
area (square meter). Acoustic power is acoustic energy per unit time and is
measured in watts (W), 1 W being 1 joule/s.
13
Intensity of sound, Fig. 1High-intensity
(top) and low-intensity (bottom) longitudinal ultrasound waves.
The relationship between acoustic intensity and particle excursions is illustrated
in Fig.1. The upper part of the figure shows an ultrasound transducer crystal
oscillating with wide excursions (high-amplitude vibration), thus producing a highintensity longitudinal wave with large differences in particle density between the
compression and rarefaction bands. The lower part of the figure shows a
transducer crystal oscillating with small excursions, therefore producing a low
intensity longitudinal wave. Here, there are small differences in particle density
between the bands of compression and rarefaction. The longitudinal waves are
also illustrated graphically as sinusoidal pressure waves. Maximum pressure
amplitudes correspond to the regions of maximum compression.
Acoustic Impedance
Acoustic impedance is the property of tissue causing resistance to the
propagation of ultrasound. Acoustic impedance is defined as Z = c, where
is the tissue density, and c is the propagation velocity of ultrasound in
the tissue. Ultrasound propagation is dependent partly upon the particle
mass (which determines the density of the tissue), partly upon the elastic
forces binding the particles together (which determine the propagation
speed of sound). A fraction of the ultrasound is reflected whenever there is a
change in acoustic impedance. The larger the change in acoustic
impedance, the larger the fraction reflected.
Z = acoustic impedance
Z=v
Z1 = 1v1
Z2 = 2 v2
R = [(Z1-Z2)/(Z1+Z2)]2
14
3- Doppler Ultrasound physics
The Doppler Effect
Johann Christian Doppler, 1803-1853 discover the general phenomenon that, the
frequency of a wave form is dependent upon the relative velocity between the emitter and
the receptor of the wave. The effect is applicable to any kind of wave, whether
electromagnetic (e.g. light) or mechanical (e.g. ultrasound).
Doppler effect, Fig. 1The Doppler effect as seen in Doppler ultrasonography.
The Doppler effect is used, in Doppler sonography, to measure blood flow
velocity. Ultrasound reflected from red blood cells will change in frequency
according to the blood flow velocity. When blood flow is directed towards the
Doppler transducer, the echoes from blood reflected back to the transducer will
have a higher frequency than the one emitted from the transducer, and when
blood flow is directed away from the transducer, the echoes will have a lower
frequency than those emitted (Fig.1). The difference in frequency between
transmitted and received echoes is called the Doppler frequency shift, and this
shift in frequency is proportional to the blood flow velocity.
Doppler Equation
Shift in frequency is termed “Doppler shift.”
Doppler Shift equation is given by:
fD = 2fvcos(θ)/c.
o
f = frequency of transmitted wave
15
o
o
o
v = source velocity
c= velocity of sound
θ = angle between “view” direction and direction of motion.
Continuous Wave Doppler Ultrasound
In the field of continuous wave Doppler ultrasound the source and receiver are
Stationary. In addition the transmitting and receiving transducers may not be in
line. Modern pulsed Doppler however uses the same transducer to transmit and
receive. Let t be the angle of the transmitter to the direction of motion and let r
be the angle of the receiver to the direction of motion. Then the velocity of the
scatterer relative to the transmitter will be
v cos(t)
and the velocity of the scatter relative to the receiver will be
v cos(r)
The Doppler shift arising from a moving object can be calculated, by the Doppler
equation which is given by.
fD = 2fvcos(θ)/c.
where v cos() is the velocity of the reflector(object) relative to the
receiver/transmitter.
This equation shows
_ fD ∞ fS.
_ increased ultrasound attenuation with frequency
_ increased back-scatter signal power with increasing frequency
_ desired beam width are taken into account fS is chosen to be 2 -20 MHz.
_ fD ∞ v.
_ fD ∞1/c.
_ fD is dependent on the angles the transmitter and receiver beams make with
the velocity vector. In particular if the receiver and transmitter beams are
16
perpendicular to blood flow fD = 0.
Continues wave instrumentation
Fig.1 Block diagram of CW Doppler
Pulsed wave Doppler
There are problems associated with conventional continuous wave (CW) Doppler
instrumentation, particularly when used as a flow detector. The most important
one being that CW is unable to provide depth of reflected object. In other words
CW is not able to separate Doppler signals arising from different points along the
transmitted ultrasound beam. The use of Pulsed Doppler is able to overcome this
problem.
A Doppler ultrasound technique for measurement of blood-flow velocity uses the
pulse echo method. Short pulses of ultrasound are transmitted with a certain
frequency, the pulse repetition frequency PRF, between pulses transmissions,
echoes are continuously returning to the transducer, but most of them are not
analyzed. A receiver gate opens only once between each pulse transmission to
allow estimation of the Doppler frequency shift from only one predetermined
range along the ultrasound beam, the sample volume.
The Doppler technique is based upon measurement of small changes in
ultrasound frequency from transmission of the pulse to reception of the echo (see
17
Doppler Effect). It is therefore important that the transmitted pulse contains a
uniform, narrow bandwidth frequency (i.e. small frequency range). The longer the
pulse, the narrower the bandwidth, and the spatial pulse length is therefore
usually longer than the one used in B mode imaging.
Transmission of ultrasound is achieved by an oscillator (Fig.1) delivering a
voltage that varies as the resonant frequency of the transducer.
Pulsed Doppler ultrasound, Fig. 1:Block
diagram of pulsed Doppler ultrasound instrument.
Pulsing of the transmission at the correct frequency (PRF) is determined by an
electric transmission gate. The oscillator also delivers electrical signals with the
transmit frequency to the quadrature detector, where the received echo signals
undergo demodulation (see quadrature detection for more details). Only small
samples of the demodulated signals are fed through the receiver gate once
between pulse transmissions, to ensure that the signals originate only from the
small sample volume. The time delay from pulse transmission to opening of the
receiver gate is regulated by the range delay, and the time period the gate is
open, is regulated by the length delay. The small samples of the demodulated
Doppler signal that pass the receiver gate once per pulse repetition period PRP ,
are fed to the sample-and-hold unit where the demodulated Doppler signal is
"recreated" from the small samples. A low-pass filter removes frequencies above
the maximum frequency (fmax= PRF/2). PRF=2fmax is the Nyquist rate in case
of sampling below it aliasing will occur. A high-pass filter (wall filter) is added to
remove unwanted high-amplitude, low-frequency signals such as those from
vessel walls. The filtered Doppler signal is then fed to speakers, and may finally
18
be visually presented as a time - velocity spectrum after analysis by e.g. a digital
FFT analyzer.
PW vs. CW Doppler
The significant differences between CW Doppler and Pulsed Doppler are
_ a single transducer is used for transmission and reception as transmission
and reception are separated in time.
_ pulsed Doppler is often incorporated as an additional signal processing step
in conventional pulse echo ultrasound (often known as duplex scanning).
_ periodic bursts of ultrasound (e.g a few cycles) are used.
_ pulsed Doppler in general is only sensitive to flow within a region termed
the sampling volume.
Range resolution in pulsed Doppler is achieved by transmitting a short burst
of ultrasound. Following the burst the received signal is mixed with a delayed
version of the transmitted burst as a reference signal. The transit time of the
transmitted pulse to the region of interest and back again is equal to this delay.
Thus the sampling volume can be moved to different positions along the beam by
changing this delay. The implications of this are clear: Flow at different depths or
at different points within a vessel can be selectively monitored. The width of the
sampling volume will be proportional to the width of the transmitted ultrasound
beam, whereas the length of this sampling volume will be proportional to the
duration of the transmitted burst of ultrasound.
4-Directional detectors -Discrimination of the direction
of flow
Overview
The Doppler instrument described so far is unable to provide us with any information
regarding the direction of motion. In instances where Doppler ultrasound is used to assess
blood flow the direction of blood flow may have diagnostic significance. The directional
information can be preserved in a number of ways
_ side-band _filtering
_ offset carrier demodulation
_ in-phase/quadrature demodulation
We will consider each of these techniques in turn. In the descriptions that follow
it must be remembered that
19
_ fD > 0 implies that velocity vector components along the beam are directed
towards the probe.
_ fD < 0 implies that velocity vector components along the beam are directed
away from the probe.
single sideband filtering detector
This method is probably the simplest. The received rf signal is passed to two
filters, one passing frequencies over the range S < < S + m and the other
passing frequencies over the range S - m < < S. The output of each filter
passes to a multiplier and bandpass filter.
Offset carrier demodulation( Heterodyne detector)
In this method of determining the direction of flow the received signal is multiplied
by a reference signal m + S. Thus as before the received signal is given by
xr(t) = r cos([ S + D]t + 1)
20
the reference signal is given by
x1(t) = 1 cos([ S + m]t)
Multiplying these two signals together gives
x1(t)xr(t) =(1r/2){cos([ m + D]t +1) + cos([2S + m + D]t + 1)}
where m is chosen such that m >=| Dmax|. As before this multiplied signal is
low pass filtered to remove the 2S component.
Thus
m + D > m
>>
+ve shifted doppler
m + D < m
>>
-ve shifted doppler
Note our tissue movement rejection filter is now a band-stop filter with a centre
frequency of m.
In-phase/quadrature demodulation ( Quadrature phase detector)
The received signal is passed to two separate multipliers, one, the in phase reference,
multiplies the signal by
xip(t) = t cos(St)
whereas the second, a +/2 phase-shifted reference, multiplies the signal by
xps(t) = t cos(St +/2)
= t sin(St)
The in-phase signal, i(t), is given as before, as
i(t) = xr(t)xip(t)= (rt/2){cos(Dt + 1) +cos([2S + D]t + 1)}
and the quadrature phase signal , q(t), is given by
q(t) = xr(t)xps(t)= (1 2/2){sin(Dt + 1) +sin([2S + D]t + 1)}
Both i(t) and q(t) are band-pass filtered and amplified as before to give
if (t) = cos(Dt + 1)
qf (t) = sin(Dt + 1)
21
The direction of the Doppler shift, and hence the direction of flow, is determined
by noting the phase relationship between if (t) and qf (t), i.e
D > 0 then qf (t) is /2 phase retarded with respect to if (t).
D < 0 then qf (t) is /2 phase advanced with respect to if (t).
In-phase/quadrature demodulation
In-phase/quadrature demodulation
Autocorrelation method
Commonly used method of estimating the mean Doppler frequency shift and hence the
mean blood-flow velocity as well as the variance of the Doppler signal in color flow
imaging. The autocorrelation method is schematically illustrated in Fig.1. Demodulated
Doppler signals from the various depths along a scan line (va, vb, etc.) are first fed
through special high-pass filters (delay line cancellers, DLCs) which remove lowfrequency signals from slowly moving objects like pulsating vessel walls or cardiac valve
leaflets. The filtered Doppler signals are then fed to the auto-correlation. Here each signal
is compared (multiplied) with a signal from the same depth derived from the previous
pulse - echo sequence, i.e. obtained one pulse repetition period, T, earlier. This is
accomplished by delaying the signal for a time period of T.
Motion of a reflector (e.g. blood flow) at a particular depth during the time interval T will
lead to a change in phase between the delayed and undelayed signals from that particular
depth. The phase difference indicates the mean velocity and velocity direction (away
from or towards the transducer) during the time interval. Registers store the product of
the delayed and undelayed signals from each depth location (a, b, etc.), and when this
procedure is repeated several times (typically 4 - 8), mean velocity and variance may be
22
calculated. This information is color coded along the particular scan line at the
appropriate depth in the final image.
Autocorrelation, Fig. 1Block diagram of
the autocorrelation method used in color flow Doppler
instruments. See text for explanation.
23
5-Basic of Ultrasound Instrumentation
Overview
Transducer is a device which can produce ultrasound by converting electrical into
mechanical energy, and detect ultrasound by converting mechanical into electrical
energy. In ultrasound instruments, the transducer has a dual function; it acts both as a
transmitter of the ultrasound beam, and as a receiver of the ultrasound echoes. There is
a wide variety of transducer configurations.
Piezoelectric properties
Piezoelectric or piezoelectric effect is the phenomenon that certain crystals change their
physical dimensions when subjected to an electric field, and vice versa; when deformed
by external pressure, an electric field is created across the crystal (from the Greek word
piezein = pressure). Piezoelectric crystals are used in ultrasound transducers to transmit
and receive ultrasound.
Effect of applied electric field
The piezoelectric crystal in ultrasound transducers has electrodes attached to its front and
back for the application and detection of electrical charges(Fig.1). The crystal consists of
numerous dipoles, and in the normal state, the individual dipoles have an oblique
orientation with no net surface charge (Fig. 1, middle). An electric field applied across
the crystal will realign the dipoles due to repulsive or attractive electric forces resulting in
compression or expansion of the crystal (Fig. 1, left and right, respectively), depending
on the direction of the electric field. (For transmission of a short ultrasound pulse, a
voltage spike of very short duration is applied, causing the crystal to initially contract and
then vibrate for a short time with its resonant frequency.)
Effect of external pressure
When echoes are received, the longitudinal ultrasound waves will compress and expand
the crystal(Fig.2). This deformation realigns the dipoles, creating net charges on the
crystal surface (Fig. 2, left and right). Note that the changes in dimensions of the
transducer crystal have been vastly exaggerated in Figs 1 and 2. In practice, the
compression and expansion only amount to a few microns.
24
Piezoelectric Transducer Construction
The main components of a simple single-element transducer are shown in Fig.1.
The front and back faces of the disk-shaped piezoelectric crystal are coated with
a thin conducting film to ensure good contact with the two electrodes
that supply the electric voltage that makes the crystal vibrate. The front electrode
is earthed to protect the patient from electric shock, and is also covered by a
matching layer, which improves the transmission of ultrasound into the body. The
back face of the crystal contain a thick backing block. The backing block will
absorb the ultrasound transmitted into the transducer and dampen the vibration
of the crystal (thereby reducing the spatial pulse length in pulsed ultrasound
transmission). An acoustic insulator of cork or rubber prevents the ultrasound
from passing into the plastic housing.
Matching Layer
25
A thin layer of material placed on the front surface of an ultrasound transducer to
improve the transfer of ultrasound into the medium of propagation (e.g. soft
tissue). The thickness of the layer should be equal to one fourth the wavelength
of the ultrasound in the matching layer (quarter-wave matching) and the acoustic
impedance should be about the geometric mean of the impedances on each side
of the matching layer:
Zm = √(Zt·Zst)
where Zm is the impedance of the matching layer and Zt and Zst are the
impedances of the transducer and soft tissue, respectively. The small amount of
ultrasound that is reflected from the distal surface of the matching layer back to
the proximal surface of the layer, will have traveled 1/2 wavelength, and will
therefore be 180° out of phase with the transmitted ultrasound. The reflected part
is thus cancelled out due to destructive interference. (The same principle applies
to the antireflex coating of optical lenses.) The matching layer increases the
amount of sound energy transmitted into the tissue and increases the bandwidth
of the ultrasound pulse. Use of two or more matching layers will reduce the
difference in acoustic impedance at the boundaries even further and will also
give a further increase in bandwidth. The increased bandwidth improves the axial
resolution by shortening the spatial pulse length.
Backing block,
Essential part of an ultrasound transducer, intimately coupled to the piezoelectric
crystal. Backing blocks are generally made of tungsten and rubber powder in an
epoxy resin. Their purpose is to mechanically dampen the vibrations of the
crystal and to shorten the transmitted ultrasonic pulse. The backing block must
absorb all sound waves from the crystal. To avoid reflections at the surface of the
backing block, the acoustic impedance of the backing block should be similar to
that of the crystal.
Transducer Characteristics
The confined, directional beam of ultrasound travels as a longitudinal wave from the
transducer face into the propagation medium. Two separate regions along the beam can
be identified, the near field or Fresnel zone, and the far field or Fraunhofer zone. Fig.1
shows the ultrasound beam as transmitted from a non-focused, single element transducer.
26
A confined, slightly converging beam shape is maintained in the near field owing to
constructive and destructive interference patterns of individual sound wavelets emitted
from the surface of the transducer crystal. The length of the near field is equal to r2/ =
d2/4, where r is the radius and d the diameter of the transducer crystal, and is the
ultrasound wavelength in the medium of propagation. Maximum ultrasound intensity
occurs at the near field - far field interface. Beam divergence in the far field results in a
continuous loss of ultrasound intensity with distance from the transducer. The angle of
divergence in the far field, , is approximately equal to arcsin(1.22/d) (or sin =
1.22/d). Note that with increasing transducer frequency (decreasing wavelength), the
length of the near field increases and the angle of divergence in the far field decreases.
Both changes improve lateral resolution in deep structures, but this beneficial effect of
high transducer frequency is counteracted by the decrease in penetration. An increase in
the diameter of the transducer crystal will also increase the length of the near field and
decrease the angle of divergence, but with the drawback of a wider ultrasound beam and
therefore decreased lateral resolution in the near field.
Radial expansion of the transducer crystal may result in unwanted side lobe formation.
Near field
Also called Fresnel zone (Augustin Jean Fresnel, 1788-1827, French physicist), the
proximal part of an ultrasound beam characterized by a confined, slightly converging beam
shape. The length of the near field is equal to r2/ = d2/4, where r is the radius and d the
diameter of the transducer crystal, and is the ultrasound wavelength in the medium of
propagation.
Far field
Also called the Fraunhofer zone (Joseph von Fraunhofer, 1787-1826, German physicist),
the distal part of an ultrasound beam characterized by a diverging shape and continuous loss
of ultrasound intensity with distance from the transducer. The angle of divergence
increases with lower transducer frequency and with smaller transducer diameter.
Focusing
A transducer transmits a focus ultrasound beam either by means of the concave
shape of the transducer itself or an acoustic lens, or through electronic focusing. The
material of acoustic lenses (usually polystyrene or an epoxy resin) propagates sound at a
higher speed than water or body tissues, and converging lenses are therefore concave
27
Focused transducer, Fig. 1:Unfocused
(top) and focused (bottom) ultrasound transducer. The ultrasound
beam is focused by means of a concave acoustic lens.
The focal point is not sharply defined; rather it is a zone in which the minimum diameter
of the beam is fairly well maintained (Fig.1). A close approximation of the focal length
is the diameter of curvature of the lens. The acoustic lens of linear transducers will focus
the beam only in the plane perpendicular to the image plane (it decreases the "slice
thickness"). Linear array transducers may focus the beam in the image plane as well
through electronic focusing. Focusing shortens the near field and the focal zone, but it
increases the divergence of the beam in the far field. See also focusing and ultrasound
beam.
28
6-Static Image Generation Using Ultrasound
Generating an A-Mode scan
Amplitude mode is called A-mode. A-mode is represented as one-dimensional
ultrasonic display showing echoes along the ultrasonic beam as vertical spikes
on a horizontal time axis indicating the depth of the reflectors. The amplitudes of
the spikes reflect the echo strengths after time gain compensation TGC, and the
left-right position of the spikes is determined by the time lag between
transmission of the ultrasonic pulse and arrival of the echo at the transducer. The
horizontal axis represents the time of the returning echo and the vertical axis
represents the amplitude of the echo.
A-scope (A-mode scan)
A-scope is an ultrasound pulse-echo system for generation of A-mode images.
An A-scope is schematically shown in Fig.1. The rate generator triggers the
transmitter, the time gain compensator and the time-base generator
approximately PRF= 1000 times/second. At this rate, an ultrasound pulse is
transmitted from the transducer. Echoes arriving at the transducer between
pulses transmission, induce electric currents (voltages) in a piezoelectric crystal,
and these voltages are amplified by the receiver.
A-scope, Fig. 1. Block diagram of
A-scope.
The user-adjustable time gain compensator (time gain control) compensates for
the attenuation of the ultrasound with time (travel distance) by increasing the
amplification factor with time from pulse transmission. The receiver output is
connected to the vertical (y) deflection plates of the cathode ray tube CRT and
deflects the time-base line. The time-base generator is connected to the
horizontal (x) plates of the CRT and makes the time-base line sweep across the
monitor.
29
Time gain compensation
TGC increases amplification of deep ultrasound echoes in order to compensate
for the progressive attenuation of the deeper echoes. TGC (also named swept
gain) is performed by the time gain control.
Time gain control.
A manual operation of gain control in ultrasound imaging provides an increasing
amplification of echoes from increasing depths. The purpose of the time-gain
control is to create a uniform grey-scale appearance throughout the ultrasound
image.
Gain control
In ultrasound imaging, Gain control is a set of manually operated controls that
regulate the echo intensities from various depths the monitor. The coarse gain control
(or main gain control) regulates echo amplitudes from all depths equally; the time
gain control (or time gain compensator) TGC provides an increasing amplification of
the echoes with increasing depth to create a uniform grey-scale appearance
throughout the image; the reject control selectively rejects echo amplitudes below a
certain threshold to enhance the clarity of the stronger echoes; the near gain control
is primarily used to diminish the strong superficial echoes; the delay control
regulates the depth at which the TGC starts; the far gain control is used to enhance
all distant echoes; and the enhancement control may be used to selectively enhance
echoes from a specific depth range.
Generating a B-Mode Image
An early B mode ultrasound instrument with a single transducer mounted on an
articulating arm (Fig.1). The scanning arm had three joints, and measurement of
the joint angles (by potensiometers or optical digital encoders) made it possible
to determine the vertical and horizontal position of the transducer, and also the
direction of the ultrasound beam. The transducer was moved manually across
the body surface in a compound fashion, all movements being restricted to a
single imaging plane determined by the position of the rigid scanning arm. In this
way, tomographic images of the body were gradually built up on the monitor. In
early versions of the static B-mode scanner, the image was created on a direct
viewing storage cathode ray tube.
30
Static b-scanner, Fig. 1:Single
transducer mounted on an articulated arm with three joints (1, 2, 3). Echoes
from a single point (P) in the body are displayed in the same position on the monitor, irrespective of the
transducer position (A or B).
On such a tube the image could be viewed for 10 minutes before it disappeared.
The storage tubes had a very limited ability to display shades of grey; some of
them could only show black and white, producing a so-called bi-stable image.
Grey-scale imaging was introduced in 1972 with the scan conversion memory
tube replacing the direct viewing storage cathode ray tubes.
Scan line
In ultrasound imaging, the position of the ultrasound beam axis during one pulse
- echo sequence. B mode images are produced by sweeping the ultrasound
beam in a plane across the region of interest while transmitting ultrasound pulses
and detecting the echoes. When a pulse is transmitted, the ultrasound beam
remains stationary until all echoes from the displayed field of view are received.
The beam then moves on to the next position. The echoes received at each
position are displayed along scan lines in the image, corresponding to the beam
axis positions. The density of the scan lines (line density) affects the lateral
resolution in the image.
31
7- Real Time Imaging (RTI)
Principle of RTI
An RTI is an ultrasound imaging system with high frame rate in order to follow
physiological motion. A flicker-free display requires at least 16 frames per second. Realtime ultrasound images are produced by two basic types of instruments, 1) the
mechanical scanner, and 2) the electronic array scanner.
Electronic Array scanner
Real-time B-mode ultrasound transducer assembly consisting of 100 or more (often 120240) rectangular shaped transducer elements (about 5-10 cm) arranged side by side (Fig.
1). Each single element is too narrow (about 2 mm) to transmit a well-defined beam and
5-10 adjacent elements are therefore driven simultaneously, working as a single
transducer. Scanning is done by first activating a group of elements at one end of the
array. The central axis of the resulting ultrasound beam, i.e. the scan line, corresponds
to the central element in the group. When all the echoes along the line have been received
and stored, the end-most element is deactivated, the nearest new element is activated, and
another transmit - receive sequence is initiated. The new scan line is parallel to the
previous one, but has been shifted one element in position along the array. In this way,
the ultrasound beam sweeps through the rectangular field of view (Fig. 1).
Linear array, Fig. 1
: Linear array transducer with multiple crystal elements.
Electronic focusing
Focusing of the ultrasound beam in the image plane during electronic array
scanning is the electronic focusing. Focusing may be done both at pulse
transmission and at echo reception.
32
During pulse transmission, focusing is accomplished by applying small time
delays to the excitation pulses driving the individual transducer elements (Fig.1).
The ultrasound beam is formed by constructive interference of the wavelets from
the individual transducer elements. When a group of elements are excited
simultaneously, the wavelets will create a wavefront that is parallel to the array of
transducer elements, and the resulting beam will be non-focused in the image
plane (Fig. 1, left). If different time delays to the excitation of the individual
elements within the group are introduced, the resulting wavefront becomes
curved, thus creating a beam that is focused in the image plane (Fig. 1, right).
The degree of focusing, and thereby the focal zone, may be controlled by the
operator.
Electronic focusing, Fig. 1Electronic focusing of the ultrasound beam during pulse transmission
In linear array transducer systems, where only a small group (e.g. 5-10) of all the
transducer elements (e.g. 120 - 240) are involved in creating the ultrasound
beam at any point in time, the time delays are applied to this small group of
elements. In phased array systems, where all of the transducer elements (e.g.
64-120) contribute to the ultrasound beam at any point in time, the time delays
are applied to the whole set of elements.
33
Electronic focusing, Fig. 2Electronic focusing during echo reception
During echo reception, focusing may be done by introducing small time delays
among the echo signals received by the individual transducer elements (Fig.2).
Echoes from a single reflector will reach the group of transducer elements that
are active during echo reception, and the echo signals from the individual
elements are summed to form a net signal that is further processed for display of
the reflector. Different time delays align the individual signals so that they are in
phase before summation. The appropriate time delay arrangement is dependent
upon the distance to the reflector, and this delay may be changed dynamically
during echo reception to optimize focusing from shallow (Fig. 2, left) and deeper
(Fig. 2, right) reflectors. Dynamic focusing has also been termed "dynamic
tracking lens”.
Phased array
It is a Real time ultrasound electronic array transducer assembly where the
ultrasound beam is both steered and focused by electronic means. Phased
array transducers usually consist of an array of 64-128 transducer elements. All
elements are involved in the formation of each beam and scan line. When all
elements transmit simultaneously, the beam travels perpendicular to the array
surface. The beam is steered at an angle by firing the individual elements
sequentially with precisely controlled time delays between the excitation pulses
(Fig.1). By varying the time delays from one pulse-echo sequence to the
34
Phased array, Fig. 1Phased array with steered, unfocused ultrasound beam.
next, the ultrasound beam is made to sweep through the sector-shaped field of
view. Adjustment of the time delays may also accomplish focusing of the
ultrasound beam in the image plane (Fig.2). Focusing in the "slice thickness"
plane is done with acoustic lenses
Phased array, Fig. 2 Phased array with steered and focused ultrasound beam
Mechanical scanner
Real-time ultrasound instrument in which the ultrasound beam is made to sweep
through the patient by mechanical means (as opposed to electronic means; see
electronic array). There are a number of different types:
Single-element transducers
The transducer itself may be driven by a motor to oscillate, or wobble, through an
angle. The oscillating transducer element may be located at the surface of the
transducer housing to produce sector-shaped images, or the element may be
withdrawn several centimeters from the front, within a bath of water or oil, to
produce trapezoidal images. The arc of the sector-shaped or trapezoidal images
is usually in the order of 45 to 90. Some mechanical scanners have a fixed
single-element transducer, and the ultrasound beam is swept through a sector by
reflection from an oscillating mirror within the transducer housing.
35
Mechanical scanner, Fig.
1The sector scanner has four transducer elements (1 - 4) mounted on a wheel that
rotates clockwise within the transducer housing.
Rotating wheel transducers
This method usually have three or four transducer elements mounted 120 or 90
apart on a wheel (Fig. 1). The wheel diameter may be 25 cm. A motor rotates the
wheel with a constant speed in one direction. The rotational frequency may be in
the order of 510 rotations per second. The transducer housing has an acoustic
window, and only the transducer that is behind the window is allowed to transmit
and receive ultrasound. The active element transmits ultrasound pulses and
receives echoes along each of perhaps 100-120 scan lines within the sectorshaped field of view. Rotating transducer systems may also be combined with
reflecting mirrors.
Generating an RTI image
Brightness mode, a two-dimensional ultrasound image display composed of
bright dots representing the ultrasound echoes. The brightness of each dot is
determined by the echo amplitude (after time gain compensation TGC ). A Bmode image is produced by sweeping a narrow ultrasound beam through the
region of interest while transmitting pulses and detecting echoes along a series
of closely spaced scan lines. The scanning may be performed with a single
transducer mounted on an articulating arm that provides information on the
ultrasound beam direction ( static B scanner), or with a real-time scanner such as
a mechanical scanner or an electronic array scanner. Real-time scanning of a
schematic "anatomical section" containing bone, an echo soft-tissue lesion
("solid"), and a fluid-filled cyst is illustrated in Fig.1, (top).
36
B-mode, Fig. 1:Linear array scanning of a schematic anatomical section (top) and the resulting B-mode
image (bottom).
A linear array transducer with multiple crystal elements is used. At each scan line
position, one ultrasound pulse is transmitted and all echoes from the surface to
the deepest range are recorded before the ultrasound beam moves on to the
next scan line position where pulse transmission and echo recording are
repeated. In the B-mode image (Fig. 1, bottom), the vertical (depth) position of
each bright dot is determined by the time delay from pulse transmission to return
of the echo, and the horizontal position by the location of the receiving transducer
element. A shadowing artifact (distal to the bone and to the lateral edges of the
fluid-filled cyst), and an enhancement artifact (distal to the cyst) are also shown.
37
8- Doppler imaging
Generating a Doppler Image history
A group of ultrasound techniques exploiting the Doppler effect to measure or
image blood flow velocity. The major techniques are pulsed Doppler ultrasound,
continuous wave (CW) Doppler, color Doppler sonography, and power Doppler
sonography.
Short historical review
The Doppler effect was first described by the Austrian mathematician and
physicist, Johann Christian Doppler (1803-1853). In his famous article of 1842,
he describes how the phenomenon affects the observed light waves from stars
having a movement relative to the observer. If the star is moving towards the
observer, the frequencies of the observed light waves are slightly higher than the
emitted frequencies, and vice versa. The change in frequency can be used to
estimate the speed of the star relative to the observer. This Doppler effect is,
however, applicable to any kind of wave, whether electromagnetic and
mechanical, and thus also to ultrasound.
The first use of ultrasound for medical diagnosis, came in the 1940s with
attempts at ultrasonographic cross-sectional imaging. In 1954, H.P. Kalmus
described how flow velocity in fluids could be determined by measuring the
phase difference between an upstream and downstream ultrasonic wave. His
"upstream - downstream" method was further developed by D.L. Franklin et al.
who in 1959 produced a flowmeter that could be mounted directly on blood
vessels. Short ultrasound pulses were transmitted through the vessel lumen
between two piezoelectric crystals, and the difference in transit time between
upstream and downstream ultrasound pulses was used for measurement of
instantaneous flow velocity.
The fact that the Doppler frequency shift could be used for the detection of blood
velocity patterns, was shown by S. Satomura in 1959. By means of
transcutaneously applied ultrasound he could visualize the patterns of flow
velocity in superficial peripheral arteries.
In 1964, D.W. Baker and H.F. Stegall presented the first Doppler instrument
intended for the transcutaneous measurement of blood flow velocity in man.
They used the continuous wave Doppler principle with two piezoelectric crystals,
one continuously transmitting ultrasound, and the other continuously receiving
the echoes. The change in frequency from emission to reception of the echoes
was used for the estimation of blood flow velocity. Approximately five years later,
pulsed Doppler instruments were introduced, allowing blood flow velocity
measurements at predetermined depths.
38
In 1974, F.E. Barber et al. described the first combined use of B-mode
ultrasonography and pulsed Doppler velocity detection, introducing the term
duplex scanning. By means of a multi-gated system, the Doppler signals were
used for production of a two-dimensional image, bright spots on the monitor
indicating presence of blood flow velocity above a certain threshold. The Doppler
image was superimposed on the B-mode image, thus producing a "duplex
image". Flow velocity was not measured.
In the late 1970s, combined real-time B-mode imaging and pulsed Doppler blood
flow velocity measurement became available, and this is the method which today
is referred to as duplex scanning. Color Doppler sonography with its color coding of
blood flow velocities, was introduced in the 1980s, followed by power Doppler
sonography in the early 1990s. The combination of duplex scanning and color
Doppler sonography is sometimes called "triplex scanning". Recently, Doppler
techniques have also been used to measure tissue velocity. Tissue Doppler imaging of
the myocardium can estimate myocardial strain and strain rate.
Duplex Scanner
Duplex scanner is the combination of real-time B-mode sonography and pulsed
Doppler ultrasound. The B-mode image gives visual guidance to the vessel of
interest for correct placement of the Doppler sample volume. The Doppler angle
may be measured by manually placing an electronic cursor parallel to the
longitudinal axis of the blood vessel (Fig.1). The scanner computer may then
automatically calculate the true blood flow velocity by means of the Doppler
equation.
Duplex scanning, Fig. 1B-mode
real-time image (top) with Doppler sample volume (two horizontal lines)
placed in the splenic vein. The broken line along the vein indicates the Doppler angle (35). The time velocity spectral display (I) is shown (bottom).
39
Duplex instruments may have several configurations. Mechanically steered
systems with multi-element transducers must switch between the imaging and
Doppler modes. During pulsed Doppler measurement, the B-mode image is
shown as a still frame ("frozen" image). There is no upgrade of the image during
Doppler acquisition. Phased array scanners can provide duplex scanning by
switching between a group of transducer elements used for B-mode imaging and
one or more elements used for Doppler acquisition. During pulsed Doppler
measurement, the B-mode image may be upgraded at variable intervals
Color Flow Imaging
Ultrasound technique producing grey-scale B-mode images with superimposed
colors indicating blood-flow velocity and direction (Fig. 1). Unlike pulsed Doppler
ultrasound techniques, which acquire Doppler signals at restricted predetermined
depths only, color Doppler sonography acquires Doppler information at multiple
locations along each scan line, i.e. at each position of the ultrasound beam
during scanning. A commonly used method for measuring blood-flow velocity in
color Doppler sonography is autocorrelation, which involves repeating the pulse echo-sequence several times (typically 4 to 8) along the same scan line, and
comparing the phase of the echo signal at each depth from one pulse - echo
sequence to the next. For stationary reflectors, the phase is the same from one
echo to the next. For moving reflectors, like red blood cells,
the phase of the signal will vary from echo to echo according to the flow velocity
and direction. The autocorrelation technique estimates the mean velocity and
variance at each depth location and places this information in a color image
memory, a process which provides data for a single scan line. The ultrasound
beam is then moved to the next scan line position, and the procedure repeated.
In the final image, each pixel containing flow information is color-coded according
to blood flow direction and mean velocity. To obtain more exact flow information
such as Doppler wave form, maximum velocity, spectral broadening, resistance
index etc., color Doppler sonography must be combined with pulsed Doppler
sonography. Since color Doppler sonography requires multiple pulse - echo
sequences at each scan line, the scanning frame rate is lower than in standard
40
B-mode imaging. To improve time resolution, the color-coded field may be
restricted to only a part of the entire image (rectangle in Fig. 1).
Power Doppler or Angio Mode
Angio Mode of Doppler ultrasound technique exploit the total power in the
Doppler signal to produce color-coded real-time images of blood flow. The
technique is also named amplitude Doppler sonography, color Doppler energy
(CDE), color amplitude imaging (CAI), and ultrasound angiography. Power
Doppler sonography is an option in color Doppler sonography instruments, and
just as in color Doppler, the Doppler signal is sampled at multiple locations along
each scan line. The technique differs from conventional color Doppler in the way
the Doppler signals are processed; instead of estimating mean frequency and
variance through autocorrelation, the integral of the power spectrum is estimated
and color coded. The colors in the power Doppler image indicate only that blood
flow is present; they contain no information on flow velocity.
Power doppler sonography, Fig. 1Two vessels, A and B, are interrogated by an ultrasound
beam (left). The time - velocity spectral displays of vessel A and B, respectively, are shown
(middle) as well as the corresponding power spectra (right). V: relative blood-flow velocity, P:
power, f: transmitted ultrasound frequency.
The principle of power Doppler sonography is illustrated in Fig.1. In the left
section of the figure, two vessels, A and B, are interrogated by an ultrasound
beam. Both vessels have approximately the same flow velocity, but the Doppler
angle is small in A and nearly 90 in B. The pulsed Doppler ultrasound time
velocity spectral display of vessel A and B, respectively, is schematically shown
(middle section, top and bottom). Due to the small Doppler angle, the relative
velocity measured in A is high (close to the true velocity). In a color Doppler
display, the vessel would show up with a bright color. The relative velocity
measured in B, is close to zero; the diastolic velocity is hardly visible above the
cut-off of the high pass filter (shaded area above and below the baseline). This
vessel would be difficult to see in color Doppler sonography. The power spectra
of these Doppler signals are schematically shown (right). The total power is the
area under the power (P) versus frequency curves. Since the acoustic power of
41
the Doppler signal from blood is proportional to the total number of scatterers, i.e
to the amount of blood at the particular location (see Rayleigh Tyndall scattering),
the power of the Doppler signals from vessel A and B will be equal, provided the
sample volume in vessel A contains the same number of red blood cells as that
in vessel B. In vessel A, the centre frequency of the Doppler signal is relatively
far from the centre transmit frequency of the Doppler transducer (f 0), and in
addition the Doppler signal has a broad spectrum of frequencies, reflecting the
broad spectrum of Doppler frequency shifts (or velocities) seen in the time velocity spectral display. (The Doppler frequency shifts are actually the
differences between the frequencies in the Doppler signal and the transmit
frequency, f0.) In vessel B, the centre frequency of the Doppler signal is very
close to the centre transmit frequency, and the frequency spectrum is narrow.
However, the areas under the power versus frequency curves, i.e. the integrals
of the power spectra, are the same for the two vessels which are therefore
equally well shown in a power Doppler image. Note that echoes from stationary
tissue will have the same frequency as the transmit frequency, and therefore no
Doppler signal.
As can be seen from Fig. 1, the total power of the Doppler signal from blood is
independent of blood-flow velocity and Doppler angle, provided the Doppler
frequency shift is different from zero. Further disturbing multicolored background.
The random noise has a fairly uniform low power, however, and is therefore
displayed with a uniform dark color (e.g. dark blue) in the power Doppler image,
clearly separated from the high-power Doppler signals from blood flow (displayed
in yellow to red). High gain settings are therefore possible with power Doppler.
Motion is a severe problem, however. Echoes from moving body organs, for
example, may have high power levels, and give bright flash artifacts. A
combination of gas micro-bubble contrast media, may solve the problem.
Power doppler sonography, Fig. 2Power
Doppler image (a) shows cortical perfusion in right
kidney; color Doppler (b) shows only the larger vessels.
42
Time Domain Correlation
It is an ultrasound non-Doppler method of estimating blood-flow velocity. The method,
which is used in some color flow instruments, is based upon measurement of reflector
(blood cell) displacement from one pulse - echo sequence to the next.
The echoes from an entire scan line are analyzed and compared (correlated) with the
echo wave-train from the previous pulse - echo sequence along the same scan line.
Fig.1A shows parts of the echo wave-trains being observed after two consecutive pulse
transmissions, pulse 1 and 2. The echoes of two stationary reflectors (S) and one moving
reflector (M) are shown. The echoes from the two stationary reflectors are detected at the
same time delays following the two pulse transmissions; there is no change in their return
time. The echo from the moving reflector (e.g. blood cells) is detected a time, t,
following pulse 2 earlier as compared to the time of detection following pulse 1; the echo
return time is shifted t to the left on the time axis.
Time - domain correlation, Fig. 1Echo trains from two consecutive pulses are shown (A). The echo
segment from the moving reflector is correlated with the echo train following the previous pulse (B). S:
stationary reflector, M: moving reflector
The difference in return time, t, is estimated by the method called time-domain
correlation. The echo wavetrain is divided into numerous segments, representing echoes
from various depths. Each echo segment from pulse 2 is correlated to the wavetrain from
pulse 1 by shifting the segment back and forth along the time axis (Fig. 1B). The shift in
echo return time is the time shift for which there is maximum overlap in shape between
the segment and parts of the previous wavetrain. Fig. 1B shows the segment containing
43
the echo from the moving reflector, M, and this segment has to beshifted t to the right to
obtain the best overlap with the corresponding segment of the previous echo wavetrain.
When all the necessary time shifts along the scan line have been found, the ultrasound
beam moves on to the next scan line, etc.
Knowing the shift in echo return time (t), the displacement (x) of the red blood cells
can be calculated:
x = c t
where c is the speed of sound. (The distance ct is divided by 2 because the ultrasound
pulse is travelling back and forth.) The blood-flow velocity relative to the ultrasound
beam axis (v') is simply the displacement (e.g. in cm) divided by the time (t) between the
two echo observations:
v' = x / t
As in Doppler ultrasound, the true blood-flow velocity v can be calculated if the angle
() between the ultrasound beam and the direction of blood flow is known:
v = v' / cos
Compared to standard Doppler ultrasound, the time-domain correlation method has at
least two advantages. 1) The axial resolution is better because shorter duration
ultrasound pulses may be applied. Doppler ultrasound requires relatively long duration
pulses to achieve a narrow bandwidth transmit frequency. In time-domain correlation,
essentially the same short transmission pulses as in B mode imaging may be used. 2)
Higher velocities may be measured without aliasing. Frequencies are not measured, only
shifts in echo return time
44
9-M-Mode imaging
principle
Motion mode, also called time motion (TM) mode. An ultrasonic display showing
data (echoes) as dots along a vertical depth axis, as opposed to the normal Amode presentation of spikes along a horizontal depth (time) axis. The brightness
of the dots is determined by the echo strength . For each Pulse repetition period
a new set of vertical A-mode data is acquired and the old A-mode data are
pushed to the left on the monitor to make room for the new data that are
appearing on the right side of the screen. In this way, the dots are made to scroll
across the screen (or alternatively on a strip of paper), thus creating bright curves
indicating vertical positional changes of the reflectors with time. The M-mode
curves provide very detailed information on the motional behaviour of reflecting
structures along the ultrasound beam and the method is especially popular in
cardiology to show the motion patterns of the various cardiac valve leaflets
Generating a 3D Image
Acquisition and presentation of ultrasound data from a three-dimensional (3D) volume.
The 3D data are obtained from sequential acquisition of two-dimensional (2D)
ultrasound images. Grey-scale B-mode imaging as well as color Doppler sonography
and power Doppler sonography may be performed in 3D. Common to all acquisition
methods is that 3D data are best obtained during a breath-hold period to avoid distortion
of anatomy due to respiratory movements. 3D acquisitions of the heart must be ECGtriggered to show the heart at different time points during the cardiac cycle without
blurring from cardiac motion. 3D ultrasound of the heart is therefore too timeconsuming for breath-holding, and is usually performed with respiratory gating. The
respiratory phases may be detected by changes in electric impedance registered by the
ECG electrodes, and acquisition may then be restricted to the expiratory phases. In
general, 3D ultrasound data may be acquired by means of mechanical localizers, remote
localizers, or mechanical 3D transducers.
Mechanical localizers
Here the ultrasound transducer is mounted on an articulating arm, similar to the ones
used in the static B-scanner. The exact position of the transducer in space is determined
by potensiometers located at the joints of the arms. The operator may move the
transducer himself, or make the transducer move under motor control, with simultaneous
recording of position and angle of the scan plane. The sequentially obtained 2D images
may be recorded on videotape and later digitized and stored in a computer for image
processing, analysis and display.
Remote localizers
Special devices emitting acoustic, optical or magnetic signals may be mounted on the
transducer, and these signals may be detected by sensors placed in the vicinity of the
45
patient. In this way, the position of the hand held transducer may be continuously
monitored.
Mechanical 3D transducers
These transducer assemblies may be hand held or mounted on a stand for external use, or
they may be mounted on an endoscope, e.g. for transoesophageal echocardiography.
The transducer may be mechanical or more often phased array. A computer controlled
motor in the assembly makes the transducer translate or rotate around an axis, thereby
defining the 3D volume. When the transducer assembly is hand held, it requires that the
operator holds the transducer completely still during the 3D acquisition period. Variants
of the mechanical 3D transducer are small motorized rotating transducers mounted on
intravascular catheters. These produce images perpendicular to the long axis of the
catheter, and when the catheter is slowly withdrawn, a stack of 2D images are obtained,
which may later be used for 3D reconstruction.
Image presentation The 3D data may be visually presented in different ways. A
common presentation is multiplanar reconstruction, showing three orthogonal planes
simultaneously; the acquisition plane, the transverse plane (perpendicular to the
acquisition plane) and the so-called C-plane, which is a plane parallel to the transducer
surface. The 3D volume may also be displayed by surface rendering, showing e.g. the
shaded surface of a fetal face or cardiac valve leaflets, or volume rendering, showing the
3D volume e.g. as a cube of voxels which may be rotated, and where layers may be
peeled away to see deeper structures (see three-dimensional rendering).
10- artifacts in Ultrasound imaging
Display of incorrect anatomy or velocity in ultrasound applications. In B mode imaging,
artefacts may appear whenever there is a violation of the following assumptions :
1. The ultrasound beam is narrow with uniform width.
2. The speed of sound is 1 540 m/s in soft tissues.
3. The attenuation of ultrasound is uniform.
4.
The ultrasound travels in a straight line directly to the reflecting object and back to
the transducer.
5.
Echoes from all depths are allowed to reach the transducer before the next ultrasound
pulse is emitted.
46
Assumption 1) may be violated by a wide beam, which causes image smearing
of echogenic objects that are smaller than the beam diameter (beam width
artifact), or by side lobes or grating lobes (side lobe artifact).
Assumption 2) that the speed of sound is constant at 1 540 m/s, is true for most
soft tissues, but it is lower in fat (1 450 m/s) and especially in silicone implants
(600 m/s). This causes errors in range and distance, and may cause the socalled speed artifact. Variations in attenuation
Assumption 3) may cause artificially increased image brightness (enhancement
artifact) or decreased image brightness (shadowing artifact).
Several artifacts are caused by violation of assumption 4, such as the mirror
image artifact or multipath reflection artifact, the reverberation artifact (also
named ring-down artifact or comet tail artifact), and split image artifact.
Assumption 5 may be violated by a too high pulse repetition frequency PRF ,
giving rise to the ambiguity artifact.
In Doppler ultrasound applications, artifacts appear whenever the Doppler
frequency shift exceeds the Nyquist limit. This causes aliasing, which may be
seen as frequency fold over or frequency wrap around in spectral Doppler, or as
a mosaic effect in color Doppler sonography. Use of gas microbubble contrast
media (see ultrasound contrast media) may cause bubble noise and blooming
artifact.
reverberation artifact
An artifact in ultrasound imaging caused by the reflection of ultrasound several
times back and forth between two closely spaced interfaces. The multiple echoes
thus created reach the transducer before the next pulse transmission, and give
rise to multiple copies of the anatomy at the interface.
47
Some useful definitions in regard to Diagnostic Ultrasound Physics
This section provides some useful definitions or information in regard to important terms
not easily found on the Internet:
Absorption is the transfer of energy from the ultrasound beam to the tissue. It is
proportional to frequency
Apodization is a method for reducing side lobes in some arrays. It gradually
decreases the vibration of the transducer surface with distance from its center. It is
usually accomplished by using more power to excite the innermost elements.
Axial resolution is the minimum separation between two interfaces located in a
direction parallel to the beam so that they can be imaged as two different
interfaces
Decibel is a way to express the ratio of two sound intensities: dB=10log10I1/I2
being I1 the reference. For instance: +3 dB = I multiplied by 2 and -3 db = I
divided by 2
Diffraction is the change in the directions and intensities of a group of waves after
passing by an obstacle or through an aperture
Duty factor is the lapse of time the transducer is actively transmitting sound
Echo ranging is the relationship between transit time and reflector depth
expressed as t = 2d/c
Grating lobes as side lobes are secondary ultrasound beams projecting off-axis at
predictable angles to the main beam. Side lobes are too small to produce
important artifacts.
Half Value Layer (HVL) is the distance the sound beam penetrates into a tissue
when its intensity has been reduced to one half of its initial value
Huygens' principle states that an expanding sphere of waves behaves as if each
point on the wave front were a new source of radiation of the same frequency and
phase
Impedance is the product of the density of a material and the speed of sound in
that material
Pulse average intensity I(PA) is the average intensity during the pulse
Lateral resolution is the minimum separation of two interfaces aligned along a
direction perpendicular to the ultrasound beam. It depends on the beam width
Partial Volume Artifact (slice thickness or volume averaging artifact), that occurs
when the slice thickness is wider than the scanned structure
Q-value means the degree that a transducer is finely tuned to specific narrow
frequency range. For instance: Low Q means wide bandwitdh and High Q means
narrow bandwidth
Range resolution is the ability to determine the depth of reflectors
Rayleigh scatterers are objects whose dimensions are much less than the
ultrasound wavelength. Scattering increases with frequency raised to the 4th
power and provides much of the diagnostic information from ultrasound
Refraction is the bending of a wave beam when it crosses at an oblique angle the
interface of two materials, through which the waves propagate at different
velocities
48
Snell's law governs the direction of the transmitted beam when refraction occurs:
sin qt = (c2/c1) x sin qi (qt and qi are transmit and incident angles respectively)
Spatial Average Intensity (SA) is the acoustic power within the beam, divided by
the beam area
Spatial Peak Intensity (SP) is the point in the sound field with maximum intensity
Side lobes are energy in the sound beam falling outside the main beam
Spatial resolution means how closely two reflectors -or scattering regions, can be
to one another while they can be identified as different reflectors
Subdicing is a technique used to overcome grating lobes: each major transducer
element is divided into smaller parts, each one being a half wave length
Temporal (instantaneous) Peak Intensity I(TP) or I(IP) is the maximum intensity
during the pulse
Time Average Intensity I(TA): average intensity calculated over the time between
pulses:
ITA= I(PA) x Duty factor
Wavelength is l=c/f (c = propagation speed; f = frequency)
Some useful definitions in Doppler US
Aliasing is an artifact that lowers the frequency components when the PRF is less
than 2 times the highest frequency of a Doppler signal
Beat frequency, for CW Doppler, is the Doppler shift
Doppler shift is the change in the perceived frequency relative to the transmitted
frequency. Doppler shift frequency: fD = fr - f0 = 2fv/c
Doppler shift frequency with incident angle: fD = 2fv cos /c
Ensemble length -packet size, shots per line- is the number of pulses per scan line.
In color Doppler, each line of sight most be pulsed several times
FFT. Fast Fourier Transform analyzer is a common device that performs spectral
analysis in ultrasound instruments. In this case, it displays different quadrature
Doppler frequencies, or reflector velocities when a sample volume cursor is used
(Doppler frequency is proportional to reflector velocity) along time
High pass filter is the wall filter
Nyquist Frequency is the maximum frequency that can be sampled without
aliasing. NF = PRF/2 (PRF stands for Pulse Repetition Frequency)
Quadrature detection is a signal processing method for directional Doppler in
which the signal reference frequency for two channels differ in phase by 1/4
period. The output Doppler signal phase for both channels also depends on the
Doppler shift, whether positive or negative
Spectral analysis is the quantitative analysis to display the distribution of
frequencies
Variance is the variation of Doppler frequencies within each pixel during a pulse
packet, effective to detect turbulence with color Doppler
49



![Jiye Jin-2014[1].3.17](http://s2.studylib.net/store/data/005485437_1-38483f116d2f44a767f9ba4fa894c894-300x300.png)