WG-09_2010-10-15_Minutes_SanFrancisco
advertisement
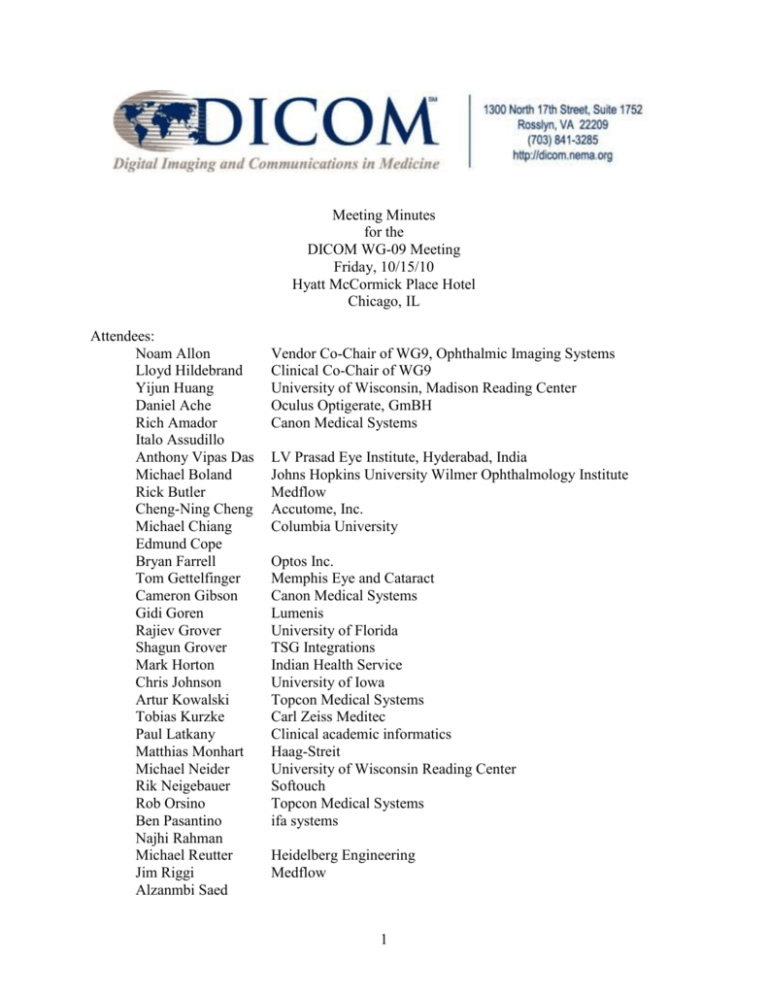
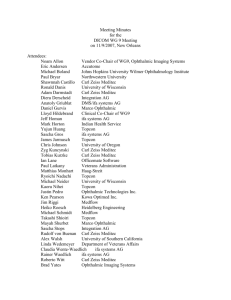
Meeting Minutes for the DICOM WG-09 Meeting Friday, 10/15/10 Hyatt McCormick Place Hotel Chicago, IL Attendees: Noam Allon Lloyd Hildebrand Yijun Huang Daniel Ache Rich Amador Italo Assudillo Anthony Vipas Das Michael Boland Rick Butler Cheng-Ning Cheng Michael Chiang Edmund Cope Bryan Farrell Tom Gettelfinger Cameron Gibson Gidi Goren Rajiev Grover Shagun Grover Mark Horton Chris Johnson Artur Kowalski Tobias Kurzke Paul Latkany Matthias Monhart Michael Neider Rik Neigebauer Rob Orsino Ben Pasantino Najhi Rahman Michael Reutter Jim Riggi Alzanmbi Saed Vendor Co-Chair of WG9, Ophthalmic Imaging Systems Clinical Co-Chair of WG9 University of Wisconsin, Madison Reading Center Oculus Optigerate, GmBH Canon Medical Systems LV Prasad Eye Institute, Hyderabad, India Johns Hopkins University Wilmer Ophthalmology Institute Medflow Accutome, Inc. Columbia University Optos Inc. Memphis Eye and Cataract Canon Medical Systems Lumenis University of Florida TSG Integrations Indian Health Service University of Iowa Topcon Medical Systems Carl Zeiss Meditec Clinical academic informatics Haag-Streit University of Wisconsin Reading Center Softouch Topcon Medical Systems ifa systems Heidelberg Engineering Medflow 1 Peter Scherer Joe Warnicke Linda Wedemeyer Katrina Winter Stephen Zhou Integration AG DARC Reading Center Department of Veterans Affairs Duke University Eye Center Aarenine . Staff: Flora Lum American Academy of Ophthalmology I. Welcome and Introductory Remarks; Introduction of Participants Dr Lloyd Hildebrand welcomed the participants. Everyone introduced themselves and described their interest in a special interest workgroup. Dr. Hildebrand noted that there were more clinicians involved in this meeting than in previous meetings. The Meaningful Use incentive program has enhanced interest in this area and this will continue to accelerate. II. Approval of Previous Meeting Minutes The minutes of the October 2009 WG9 meeting in San Francisco were approved. III. Biometry Subgroup Dr. Wedemeyer reported that the Supplement on Axial Length Measurements was approved for final text in June 2010. To benefit clinicians, this will not only provide the axial measurement data but also the IOL calculations. Dr. Hildebrand noted that this will have a significant impact, given the 2.9 million cataract procedures being performed in the United States each year. Also, this will have great utility, because axial length measurements are needed in multiple places, e.g., operating room, patient exam areas. Dr. Chiang remarked that these Supplements provide the vehicle to collect the data which is the first step to creating a data source that can be used for clinical decision support to inform decisionmaking and improve patient outcomes. VI. Visual Field Subgroup Dr. Boland reported that Supplement on Visual Fields (Static Perimetry) was approved for final text in August 2010. This will provide useful data that previously was available mostly as a printout that needed to be scanned into the electronic health record. Dr. Hildebrand noted that this will also have a significant impact because of the high frequency of visual field reporting. VII. Ophthalmic Mapping Subgroup 2 Yijun Huang reported that this group has focused on retinal thickness mapping: a set of measures that are distributed topographically and are typically presented in pseudo-color representation. This is expected to go out for public comment in a couple of weeks and be available as final text by end of summer of 2011. Yijun Huang also reported that the Ophthalmic Thickness Mapping (OPM) Information Object Definition (IOD) is well complement with the OPT IOD in the real-world use case. The OPT Information Object Definition (IOD) does provide a tremendous amount of information about the OCT image, while the OPM together with the Structured Report for Macular Grid Thickness and Volume, covers the quantitative analysis results for OCT macular scans. It is also noted that the OCT analysis and reporting for glaucoma applications are not well covered comparing to those for the retinal applications. VIII. Adoption in the Marketplace The group discussed at length the barriers to adoption in the marketplace. There has been progress over the past year. Yijun Huang reported that the University of Wisconsin Reading Center has strived to become a DICOM-centric reading center and to embrace the DICOM standard. It was suggested that the Wisconsin Reading Center submit a clinical paper describing the standardization of clinical images to help foster dissemination. Jim Riggi reported that Medflow had 10 practice sites with DICOM implementation, and another 15 sites with planned DICOM implementation. Noam Allon noted that eventually the marketplace would sort out and DICOM integration would be the solution, given the current legacy equipment base. It was also pointed out that hospital IT departments are increasingly requiring DICOM capability, understanding the need for integration. Members of the group reported that the biggest challenge is for physicians to understand the value of DICOM integration enough to undertake the purchase of upgraded equipment that has this capability. The installed base of equipment consists mainly of legacy equipment that does not have the DICOM integration capability. One option is to provide the encapsulated pdf, which is good enough for image viewing and can enhance workflow efficiency. However, clinicians pointed out that this is only the first step, and most clinicians would like to go further, having the data to be able to manipulate and to help in clinical decision making. Also, a capture station may have multiple steps involved in obtaining the encapsulated pdf versus a more streamlined approach to obtain the native DICOM object. This raw data is also important for meaningful use because it can be utilized for clinical decision support. This is important for device manufacturers because with the meaningful use incentives, there is a need to provide data to the EHR for clinical decision support. IV. Summary of IHE Eye Care 3 IHE Eye Care starts with DICOM modality worklist. Images and measurements are stored automatically along with the metadata. All of the current DICOM modalities are supported, including ophthalmic photography, ultrasound, ophthalmic tomography, refractive measurements, and encapsulated pdf. This means that validated patient demographics are received electronically, eliminating errors. The format is standardized and vendor-independent for data migration and interoperability. This year, there are 10 vendors who participated in the October Connectathon and Showcase, which is more than last year. There are educational materials to provide guidance to ophthalmologists on how to specify IHE compliance and DICOM conformance in their RFPs. A user handbook is being worked on and can be circulated to the vendors for comment. VIII. New Work Items and Action Steps The group agreed to form two new workgroups. One workgroup is to explore reporting, led by Michael Chiang, MD. Other interested members include Ben Pasantino, Linda Wedemeyer, MD, Mark Horton, OD, MD, Paul Latkany, MD and an individual (TBD) from Medflow. The first item of business will be to explore different formats of reporting, including DICOM Structured Report (SR). The clinical requirements need to be the driver of this process but this will be technology-enabled. It was thought that the initial reports should focus on interpretations of specific imaging modalities, i.e., a diabetic retinopathy report based on a fundus photograph. This would be separate from an overall clinical impression or summary report which would synthesize the patient history, clinical findings upon examination with all of the diagnostic testing results. Specific subgroups may be needed to tackle the different types of reports, e.g., OPT, VF, OP, Axial Length Measurements, etc. The group believed that summary reports and progress reports would be more difficult to tackle because of the significant need for structured terminology and the longer standard-setting process involved in HL7. The other workgroup is to focus on open source software development to facilitate DICOM implementation by different vendors. This group is being led by Yijun Huang, and other interested members include Paul Latkany, MD, Gidi Goren, Edmund Cape, Cheng-Ning Chang and Joe Warnicke. Another possible interested individual might be Peter Kuzmak because of his work within the VA. Another potential work item is for OCT in glaucoma-related applications. Another important area is for corneal topography and wavefront technology. However, these device manufacturers are not currently represented in the WG9. Lloyd Hildebrand, MD and Flora Lum, MD will try to identify companies and solicit their participation for the next WG9 meeting. IX. Next Meetings of the Working Group 9 A. ASCRS, March 2011, San Diego B. Friday, October 24, Academy Annual Meeting, Orlando 4 Reported by: Flora Lum, Secretary November 2, 2010 Reviewed by counsel: November 3, 2010 5
![[#MIRTH-1930] Multiple DICOM messages sent from Mirth (eg 130](http://s3.studylib.net/store/data/007437345_1-6d312f9a12b0aaaddd697de2adda4531-300x300.png)