Appendix 1. Principles of photoacoustic tomography 1
advertisement

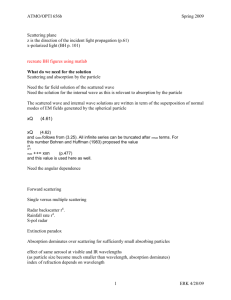
Appendix 1. Principles of photoacoustic tomography 1. Photoacoustic (or optoacoustic) imaging Optoacoustic (or photoacoustic) imaging is a hybrid method where the image contrast is determined primarily by optical absorption, while image resolution is determined by ultrasound [1,2]. Optoacoustic tomography is becoming useful for small animal imaging in preclinical studies [3,4]. It might also help in assessing human breast cancer where it could be used for high-resolution anatomical and molecular imaging [3,4]. The optoacoustic (or photoacoustic) effect was first described by Adam Graham Bell in 1880 [1]. Wilhelm Conrad Röntgen has also published about this theme [2]. In principle, if a short near-infrared (NIR) light pulse is absorbed by a small target, then the target's initial thermoelastic expansion generates exponentially decaying broadband acoustic pressure waves that can be measured by ultrasound detectors for generating images (Appendix Fig. 1). Appendix Fig. 1: Principle of photoacoustic imaging A short light pulse from a pulsed Laser is partially absorbed by a target within the tissue. Due to the photoacoustic effect this target slightly expands. This thermoelastic expansion causes broadband ultrasound waves that can be measured by a broadband ultrasound detector. This principle allows for molecular imaging, where high-resolution ultrasound images carry information about the target's light absorption characteristics. These spectral characteristics depend on the target's molecular composition. The NIR-light pulses in optoacoustic imaging are usually generated by a pulsed laser with pulse durations of about 10 nanoseconds, which fulfills the stress confinement [5]. The higher the target's NIR-light absorption, the higher is the amplitude of the emitted acoustic wave [5]. 1 In biological tissue any NIR-light imaging is complicated by light scattering. The NIR photons are diffusively scattered by small tissue particles (Mie-scattering) and therefore need more time to travel through a volume element (voxel) [6,7]. This prolongation of the mean photon pathway causes that the voxel's molecules can absorb more NIR-light than if the NIRlight would pass straight through that voxel only once. Noteworthy, within the range of 6501100 nm the scattering decreases smoothly at increasing wavelength, which may be utilized in reconstruction algorithms [6,7]. The effective NIR-light absorption depends on absorption, scattering, and anisotropy of the tissue [5]: eff = (3 a (a + s'))1/2, with s' = s (1 g) (formula 1) where eff is the effective absorption (cm1); a is the absorption coefficient (cm1); 's is the reduced scattering coefficient (cm1); s is the scattering coefficient (cm1); g is the anisotropy factor (dimensionless, about 0.9 in biological tissue). Typical values in the breast are a = 0.05 cm1 and s' = 10 cm1 at 800 nm [8]. The reduced scattering coefficient 's is much larger than the absorption coefficient a, allowing for a simplification: eff = (3 a s')1/2, with s' = s (1 g) (formula 2) For imaging purposes the optoacoustic measurements must be performed spatially-resolved. Light (speed ~3108 m/s) travels much faster through the tissue than acoustic waves (speed ~1.54103 m/s), so that the propagation time of the NIR-light is negligible when measuring acoustic waves. The time delay between the laser pulse and the arrival of the sound wave at the ultrasound detector is used to estimate the depth of the tissue voxel where the optoacoustic effect occurred. The three-dimensional position of this voxel is determined by using a sufficiently large two-dimensional array of acoustic detectors and tomographic reconstruction. Among the reconstruction algorithms for the three-dimensional map of optoacoustic sources are filtered back-projection and iterative image reconstruction [9,10]. The latter requires more computation time but can result in more accurate images [11]. Similar to all other noninvasive imaging methods, some imaging artifacts must be considered. For example, artifacts may be caused by internal reflection or scattering of acoustic waves but can be reduced by the reconstruction algorithm [10]. 2 2. Reconstruction of absorption coefficients from photoacoustic tomographic measurements In scattering media the light transport at wavelength is modeled by the light diffusion equation [12]: D(r) U(r) + a(r) U(r) = q0 (formula 3) where r is the tomographic position of interest; D(r) = 3 (s' + a) is the spatially-dependent diffusion coefficient of the medium; s' is the reduced scattering coefficient at position r; a is the absorption coefficient at position r; U(r) is the photon fluence rate at position r; q0 is the source term of the isotropic light source. Optoacoustic tomography provides images of the NIR-light energy that was converted to the ultrasound energy by the optoacoustic effect. At each wavelength and at each voxel r, the locally absorbed light energy H(,r) is proportional to the local absorption coefficient a(,r) and the local light fluence U(,r) [13,14]: H(,r) ~ a(,r) U(,r) (formula 4) As an example for U, according to DIN EN 60 825-1 the maximum permissible light fluence at the skin surface is U = 20 mJ/cm2 at 700 nm and U = 100 mJ/cm2 at 1050 nm [15]. In tissue the light fluence U diminishes exponentially with depth due to attenuation of the NIR-light. In formula (3) two variables (a and U) must be determined by one equation, which requires further information about a and/or U. While a solely depends on the measured object, the tomographic map of U depends on several factors such as intensity of the incident light, measurement geometry, way of light propagation, and the effects of scattering and absorption on the photon pathway from the light source to the place of the optoacoustic effect. Different methods have been developed for modeling the spatial distribution of U, such as iterative approaches [12], sparse signal decomposition [13], and analytical normalization [16]. Sparse signal decomposition utilizes that U varies at a larger spatial frequency than a [13]. 3 3. Multispectral optoacoustic tomography (MSOT) In-vivo imaging with NIR light utilizes the 650900 nm spectral range where the light can travel several centimeters through biological tissues due to the relatively low light absorption in this spectral window. A further smaller spectral window exists around 1064 nm, where the scattering is about 30% lower and the maximum permitted laser illumination is 5-fold higher than at 700 nm (see section 4 below) [6,7,15]. In the wavelength range of 6501100 nm the dominant natural NIR-light absorbers in the human breast are water, lipids, oxyhemoglobin and deoxyhemoglobin[1719]. There also is some background absorption from other tissue components. The spectral range of 650900 nm is most useful for differentiation of oxyhemoglobin and deoxyhemoglobin. Also, most exogenous optical contrast agents such as indocyanine green have their characteristic spectral signatures in this wavelength range. The spectral range of 9001100 nm is suitable for differentiating water and lipids [17,18]. In multi-spectral optoacoustic tomography (MSOT) several optoacoustic measurements are performed sequentially at multiple wavelengths. The major NIR light absorbers within each tomographic voxel are then obtained by spectral decomposing [20,21]. 4. Maximum permitted laser illumination of the skin The skin's maximum permitted laser illumination according to DIN EN 60 825-1 is summarized in Table 1. Per second a single laser pulse (in mJ/cm2) may contribute up to 10% to the average illumination (in mW/cm2), i.e. it may be repeated at a frequency of 10 Hz. At higher repetition frequencies the single pulse's maximum illumination is reduced correspondingly for considering the skin's maximum average illumination. Table 1: Maximum permitted laser illumination of the skin 1 in the near-infrared (NIR) range of 6501100 nm Single Average laser pulse, illumination, duration duration wavelength, 1100 ns, 500 min, nm mJ / cm2 mW / cm2 650 20 200 700 20 200 750 25 251 800 31 316 850 39 399 900 50 502 950 63 632 1000 79 796 1050 100 1000 1100 100 1000 1 according to DIN EN 60 825-1 [15] 4 References of Appendix 1 1. Bell AG (1880) On the production and reproduction of sound by light. Am J Sci 118:305–324 2. Röntgen WC (1881) On tones produced by the intermittent irradiation of a gas. Philosophical Magazine (Series 5) 68:308–311 3. Ntziachristos V (2010) Going deeper than microscopy: the optical imaging frontier in biology. Nat Methods 7:603614 4. Ntziachristos V, Razansky D (2010) Molecular imaging by means of multispectral optoacoustic tomography (MSOT). Chem Rev 110:27832794 5. Oraevsky AA, Jacques SL, Tittel FK (1997) Measurement of tissue optical properties by time-resolved detection of laser-induced transient stress. Appl Opt 36:402415 6. van Staveren HJ, Moes CJ, van Marie J, Prahl SA, van Gemert MJ (1991) Light scattering in Intralipid-10% in the wavelength range of 400-1100 nm. Appl Opt 30:45074514 7. Pogue BW, Jiang S, Dehghani H et al (2004) Characterization of hemoglobin, water, and NIR scattering in breast tissue: analysis of intersubject variability and menstrual cycle changes. J Biomed Opt 9:541552 8. Leff DR, Warren OJ, Enfield LC et al (2008) Diffuse optical imaging of the healthy and diseased breast: a systematic review. Breast Cancer Res Treat 108:922 9. Kostli KP, Frenz M, Bebie H, Weber HP (2001) Temporal backward projection of optoacoustic pressure transients using fourier transform methods. Phys Med Biol 46:18631872 10. Dean-Ben XL, Ma R, Razansky D, Ntziachristos V (2011) Statistical approach for optoacoustic image reconstruction in the presence of strong acoustic heterogeneities. IEEE Trans Med Imaging 30:401408 11. Renker M, Nance JW Jr, Schoepf UJ et al (2011) Evaluation of heavily calcified vessels with coronary CT angiography: Comparison of iterative and filtered back projection image reconstruction. Radiology 260:390399 12. Jetzfellner T, Razansky D, Rosenthal A, Schulz R, Englmeier KH, Ntziachristos V (2009) Performance of iterative optoacoustic tomography with experimental data. Appl Phys Letters 95:013703. 13. Rosenthal A, Razansky D, Ntziachristos V (2009) Quantitative optoacoustic signal extraction using sparse signal representation. IEEE Trans Med Imaging 28:19972006 5 14. Ma R, Taruttis A, Ntziachristos V, Razansky D (2009) Multispectral optoacoustic tomography (MSOT) scanner for whole-body small animal imaging. Opt Express 17:2141421426 15. DIN EN 60 825-1 (VDE 0837-1): 200111. 16. Razansky D, Ntziachristos V (2007) Hybrid photoacoustic fluorescence molecular tomography using finite-element-based inversion. Med Phys 34:42934301 17. Hale GM, Querry MR (1973) Optical constants of water in the 200-nm to 200-microm wavelength region. Appl Opt 12:555563 18. van Veen RL, Sterenborg HJ, Pifferi A, Torricelli A, Chikoidze E, Cubeddu R (2005) Determination of visible near-IR absorption coefficients of mammalian fat using timeand spatially resolved diffuse reflectance and transmission spectroscopy. J Biomed Opt 10:054004 19. Kuenster JT, Norris KH (1994) Spectrophotometry of human haemogobin in the near infrared region from 620 to 2500 nm. J Near Infrared Spectrosc 2:5965 20. Glatz J, Deliolanis NC, Buehler A, Razansky D, Ntziachristos V (2011) Blind source unmixing in multi-spectral optoacoustic tomography. Opt Express 19:31753184 21. Razansky D, Buehler A, Ntziachristos V (2011) Volumetric real-time multispectral optoacoustic tomography of biomarkers. Nat Protoc 6:11211129 6