The Cardiovascular System: The Blood

The Cardiovascular System: The Blood
Blood contributes to homeostasis by transporting oxygen, carbon dioxide, nutrients, and hormones to and from the body’s cells. It helps regulate body pH, provides protection against disease through phagocytosis and the production of antibodies.
The cardiovascular system consists of three interrelated components: blood, the heart, and blood vessels.
Most cells of a multicellular organism cannot move around to obtain oxygen, nutrients, eliminate carbon dioxide and other wastes. These needs are met by two fluids: blood and interstitial fluid. Blood is a connective tissue composed of a liquid extracellular matrix, the blood plasma that dissolves and suspends various substances and suspends various cells and cell fragments. Interstitial fluid is the fluid that bathes body cells.
Functions of Blood
Blood, a liquid connective tissue, has three general functions:
1.
Transportation. Blood transports oxygen, carbon dioxide, nutrients, and hormones. Blood also transports heat and waste products to various organs for elimination from the body.
2.
Regulation. Circulating blood helps maintain homeostasis of all body fluids.
Blood regulate pH through its buffing activities. The blood adjusts body temperature through its properties of the water and as it flows through the skin, excess heat can be lost from the blood to the environment. Blood osmotic pressure influences the water content of cells mainly through dissolved ions and proteins in the blood plasma.
3.
Protection. Blood can clot, protects against its excessive loss from the cardiovascular system after an injury. White blood cells protect against disease by carrying on phagocytosis and production of antibodies. Several types of blood proteins help protect against disease as they are the antibodies.
Physical Characteristics of Blood
Blood is thicker than water and has a slightly alkaline pH ranging from 7.35 to 7.45. Blood constitutes about 20% of extracellular fluid. Blood is 8% of the total body mass. The blood volume is 5 to 6 liters. Several hormones ensure that blood volume and osmotic pressure remain relatively constant and regulate how much water is excreted in the urine.
1
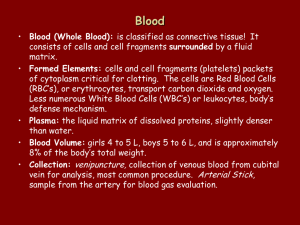
Components of Blood
Blood has two components:
1. Blood plasma, a watery liquid extracellular matrix that contains dissolved and suspended substances;
2. Formed elements, which are cells and cell fragments.
Blood is about 45% formed elements and 55% plasma. 99% of the formed elements are red blood cells (RBCs). Pale, colorless white blood cells (WBCs) and platelets (Plts) occupy less than 1% of total blood volume. The WBC and Plts form a very thin buffy coat layer between the packed RBCs and plasma in centrifuged blood.
Blood Plasma
When the formed elements are removed from blood, a straw-colored liquid called blood plasma (plasma) is left. Blood plasma is about 91.5% water and 8.5% solutes (7% by weight are proteins). Proteins in blood are the plasma proteins. Proteins play a role in maintaining proper blood osmotic pressure.
Plasma proteins are albumins (54% of plasma proteins), globulins and fibrinogen. Certain white blood cells develop into cells that produce gamma globulins also called antibodies or immunoglobulins.
Solutes in plasma include electrolytes, nutrients, and regulatory substances such as enzymes, hormones, gases, and waste products such as urea, uric acid, creatinine, ammonia, and bilirubin.
Formed Elements
The formed elements of the blood: red blood cells (RBCs), white blood cells (WBCs), and platelets (Plts). RBCs and WBCs are whole cells, platelets are cell fragments. RBCs and platelets have just a few functions, while WBCs have several specialized functions.
Types of WBCs: neutrophils, lymphocytes, monocytes, eosinophils, and basophils – each with a unique microscopic appearance and carry out specific functions.
.
The percentage of total blood volume occupied by RBCs is the hematocrit, which on average is 45%.
Anemia is when the percentage of RBCs is lower than normal. Polycythemia is when the percentage of RBCs is higher than normal.
2
Red Blood Cells
Red blood cells (RBCs) or erythrocytes contain the oxygen-carrying protein hemoglobin (Hb) which is a pigment that gives whole blood its red color. Healthy adult males have about 5.4 million red blood cells per microliter (uL) of blood. Adult females have about 4.8 million/µL.
The average RBC count is 5.0 million/µL. To maintain normal numbers of RBCs, new mature cells must enter the circulation at a rate of at least 2 million per second to balance the high rate of
RBC destruction.
RBC Anatomy
RBCs are biconcave discs. The shape increases surface area to hold hemoglobin. Their cell membrane is both strong and flexible, which allows the RBCS to deform without rupturing as they squeeze through narrow capillaries. Glycolipids in the cell membrane of RBCs are antigens that account for the various ABO and Rh blood groups. Mature RBCs lack a nucleus and other organelles and can neither reproduce nor carry on extensive metabolic activities. The RBCs cytosol contains hemoglobin molecules which are synthesized before loss of the nucleus during RBC maturation. The hemoglobin constitutes about 33% of the cell’s weight.
RBC Physiology
The mature RBCs are highly specialized for their O
2
transport function, because all organelles are lost all internal space is available for O
2
transport. Since RBCs lack mitochondria and generate ATP anaerobically, they do not use any of the O
2
they transport.
The biconcave disc shape increases surface area for the diffusion of gas molecules into and out of the RBC than would a sphere.
Each RBC contains 280 million Hb molecules. An Hb molecule consists of the protein globin. The globin is composed of 4 polypeptide chains, a ring-like nonprotein pigment, heme, which is bound to each of the 4 chains. At the center of the heme is ferrous ion (Fe +2 ) that can reversibly combine with one O
2
molecule in a reaction known as an oxygenation.
Each hemoglobin molecule can bind to 4 O
2
molecules. Hb also transports CO
2.
The CO
2 combines with amino acids in the globin part of the Hb.
RBC Life Cycle
The mature RBCs live only about 120 days. Ruptured RBCs are removed from circulation and destroyed by fixed phagocytic macrophages in the spleen and liver. Some of the breakdown products are recycled while other breakdown products are excreted in the urine and in the feces.
3
Erythropoiesis: Production of RBCs
Erythropoiesis is the production of RBCs in the red bone marrow. The precursor RBCs synthesizes the hemoglobin. The RBC near the end of the development ejects it nucleus.
Loss of the nucleus causes the center of the cell to indent, producing biconcave shape.
Erythropoietin (EPO) is a hormone produced in the kidneys that stimulates production of
RBCs. As the number of circulating RBCs increases more oxygen can be delivered to body tissues.
Types of WBCs
White blood cells or leukocytes have nuclei. WBCs are classified as either granular or agranular cells, depending on whether they contain chemical-filled cytoplasmic granules.
Granular leukocytes include neutrophils, eosinophils, and basophils; agranular leukocytes include lymphocytes and monocytes.
Granular Leukocytes
After staining, each of the three types of granular leukocytes displays conspicuous granules with distinctive coloration that can be recognized under a light microscope. Large uniformsized granules in eosinophils stain red-orange with the acidic stain (eosin). The granules usually do not cover or obscure the nucleus. The nucleus has two lobes connected by a thick strand of chromatin. The variable-sized granules of the basophils stain blue-purple with basic stain (methylene blue).The basophilic granules obscure the S-shaped nucleus. The granules of the neutrophil are smaller, evenly distributed and pale lilac in color. The nuclei of the neutrophils have two to five lobes, connected by very thin strands of chromatin.
Agranular Leukocytes
Lymphocyte
The nucleus of a lymphocyte is round or slightly indented and stains dark blue. The cytoplasm stains sky blue and forms a rim around the nucleus.
Monocytes
The nucleus of a monocyte is horseshoe shaped. The monocyte’s cytoplasm is blue-gray and has a foamy appearance. The color and appearance are due to fine azurophilic granules, which are lysosomes, scattered in the cytoplasm. On leaving the blood the monocytes can differentiate into macrophages. Some of these cells become fixed macrophages and reside in a particular tissue. Other macrophages become wandering macrophages, which roam the tissues and gather at sites of infection or inflammation.
4
Functions of WBCs
WBCs are far less numerous than RBCs; 5,000-10,000 cells per uL of blood (average
7, 500/µL of blood). The RBCs outnumber the WBCs 500-700:1. Leukocytosis an increase in the number of WBCs above 10,000/uL is a normal, protective response to stresses such as infection and inflammation. An abnormally low level of white blood cells (below 5000/uL) is termed leukopenia.
Once pathogens enter the body, the general function of white blood cells is to combat them by phagocytosis or immune responses. To accomplish these tasks, many WBCs leave the blood and collect at sites of pathogen invasion and inflammation. Granulocytes and monocytes leave the blood to fight injury or infection and these cells never return to the circulatory system. Lymphocytes, on the other hand, continually recirculate from blood to interstitial spaces of tissues to lymphatic fluid and back to blood.
Inflammation is a localized protective tissue response to injury or infection. Inflammation produces swelling, redness, heat, pain in the area of the injury or infection and even loss of function. Inflammation is designed to confine, dilute and destroy the infecting agent or injured tissue.
WBCs leave the blood by a process termed emigration or diapedesis, in which they roll along the endothelium, stick to it, and then squeeze between endothelial cells.
Neutrophils and macrophages are active in phagocytosis, they ingest bacteria, dispose of dead matter. Chemicals released by microbes and inflamed tissues by chemotaxis attract the phagocytes. Neutrophils respond most quickly to tissue destruction by bacteria. After engulfing a pathogen during phagocytosis, a neutrophil releases chemicals to destroy the pathogen.
Monocytes take longer to reach a site of infection than do neutrophils. They arrive in larger numbers and destroy more microbes. They enlarge and differentiate into macrophages, clean up cellular debris and microbes by phagocytosis after an infection.
At sites of inflammation, basophils leave the capillaries, enter tissues, and release granules that contain heparin, histamine, and serotonin. These substances intensify the inflammatory reaction.
Eosinophils leave the capillaries and enter interstitial tissue fluid to release enzymes, for example histaminase. This enzyme combats the effects of histamine which is involved in inflammation during allergic reactions. Eosinophils also phagocytize antigen-antibody complexes and parasitic worms.
Lymphocytes are the major cells in the immune system. Three main types of lymphocytes are B cells, T cells, and natural killer cells. B cells develop into plasma cells, produce antibodies are particularly effective in destroying bacteria and inactivating their toxins.
5
T cells attack viruses, fungi, transplanted cells. Natural killer cells attack a wide variety of infectious microbes and tumor cells.
A differential white blood cell count expressed as a percentage (%) is a count of each of the five types of white blood cells. The percentages of each type in the blood are:
Granulocytes – neutrophil 70%, eosinophil 2%, basophil 0.5-1%;
Agranulocytes – lymphocyte 25%, monocyte 3%.
Platelets
Megakaryocytes are large cells in the bone marrow that splinter into 2000 to 3000 fragments. Each fragment, enclosed by a piece of cell membrane, is a platelet (thrombocyte). Platelets after breaking off from the megakaryocytes then enter the circulation. There are 150,000 to 400,000 platelets/uL of blood (average 250,000/µL). Each platelet is disc-shaped, with no nucleus.
Platelets function to help stop blood loss from damaged blood vessels by forming a platelet plug. The platelet granules contain chemicals that promote blood clotting.
Complete Blood Count
A complete blood count (CBC) consist of RBCs, WBCs, and platelets counts per uL of whole blood, hematocrit, a differential white blood cell count and hemoglobin determination in grams per deciliter of blood (average 14.5g/100mL).
Hemostasis
Hemostasis, not to be confused with the homeostasis, is a sequence of responses that stops bleeding. When blood vessels are damaged or ruptured, hemostatic response must be quick, localized to the region of damage and controlled to be effective. Mechanisms that reduce blood loss are: (1) vascular spasm, (2) platelet plug formation, (3) blood clotting (coagulation).
Hemostasis prevents hemorrhage, the loss of a large amount of blood from the blood vessels.
Hemostatic mechanisms can prevent hemorrhage from smaller blood vessels, but cannot prevent hemorrhage from larger vessels.
Mechanical Changes
Vascular Spasm
When small arteries or arterioles are damaged, circular smooth muscle in their walls contracts immediately, a reaction called vascular spasm. This reduces blood loss during which time the other hemostatic mechanisms go into operation.
6
Platelet Plug Formation
Granules within the platelets release stored chemicals such as clotting factors, ADP, ATP, and
Ca
2 + , serotonin, enzymes and a hormone that proliferate cells to repair damaged blood vessels.
Platelet plug formation occurs as follows:
1. Platelet adhesion - The platelets contact and stick to parts of a damaged blood vessel;
2. Platelet release reaction - The platelets become activated by disintegrating and liberate their
granular contents. The liberated chemicals activate other platelets.
3. Platelet aggregation – The released chemicals makes the platelets sticky, causes them
to adhere to each other. Accumulation of platelets form a mass called a platelet plug.
A platelet plug is effective in preventing blood loss in a small vessel. Initially the platelet plug is loose; it becomes quite tight when reinforced by fibrin threads formed during blood clotting.
Chemical Changes
Blood Clotting
Normally, blood remains in its liquid form as long as it stays within its vessels. If it is drawn from the body, it thickens and forms a gel after a time. The liquid separates from the gel.
The separated straw-colored liquid, called serum is blood plasma minus the clotting proteins.
The gel, called the clot, consists of a network of insoluble protein fibers called fibrin in which the formed elements of blood are trapped. The process of gel formation, called clotting or coagulation is a series of chemical reactions that culminates in formation of fibrin threads.
Clotting involves several substances known as clotting (coagulation) factors. These factors include calcium ions (Ca
2+ ), inactive enzymes synthesized by hepatocytes (liver cells) and released into the blood as well as molecules released from platelets and from damaged tissues.
Clotting is a complex cascade of enzymatic reactions in which each clotting factor activates molecules of the next reaction in a fixed sequence. Finally, the insoluble protein fibrin is formed. Clotting can be divided into three stages:
1. Two pathways, the extrinsic pathway and the intrinsic pathway lead to the formation of
prothrombinase. Once prothrombinase is formed, the steps involved in clotting are the
same for both the extrinsic and intrinsic pathways and are referred to as the common
pathway.
2. Prothrombinase converts prothrombin into thrombin.
3. Thrombin converts soluble fibrinogen into insoluble fibrin. Fibrin forms the threads of
the clot.
7
The Extrinsic Pathway
The extrinsic pathway of blood clotting due to injury from cells outside (extrinsic to) blood vessels.
The Intrinsic Pathway
The intrinsic pathway due to injury within (intrinsic to) the blood vessels, the outside tissue damage is not needed.
The Common Pathway
Prothrombinase marks the beginning of the common pathway. Prothrombinase and Ca catalyze the conversion of prothrombin to thrombin. Thrombin in the presence of Ca 2+
2+
, converts fibrinogen to loose fibrin threads, which are insoluble. Thrombin also activates fibrin stabilizing factor, which strengthens and stabilizes the fibrin threads into a sturdy clot. Blood coagulation is a positive feedback mechanism.
Clot Retraction
Clot retraction is tightening of the fibrin clot. As the clot retracts, it pulls the edges of the damaged vessel closer together. Permanent repair of the blood vessel can then take place.
Role of Vitamin K in Clotting
Normal clotting depends on vitamin K. Vitamin K is not involved in clot formation. Vitamin
K is produced by bacteria in the large intestine. Vitamin K is required for synthesis of 4 clotting factors made in the liver. Vitamin K is a fat soluble vitamin absorbed into the blood.
Hemostatic Control Mechanisms
Fibrinolytic system dissolves small clots at a site of damage once the damage is repaired.
Dissolution of a clot is called fibrinolysis. When a clot is formed, an inactive plasma enzyme called plasminogen is incorporated into the clot. Blood contains substances, such as tissue plasminogen activator (t-PA) that can activate plasminogen to plasmin (fibrinolysin), the active plasma enzyme. Once plasmin is formed, it can dissolve the clot by digesting fibrin threads and inactivating clotting factors.
Clot formation normally remains localized at the site of damage. A clot does not extend beyond a wound site into the general circulation because fibrin absorbs thrombin into the clot. Due to dispersal of the clotting factors in the blood, concentrations of these clotting factors are not high enough to bring about widespread clotting.
8
Intravascular Clotting
Blood clots sometimes form within the cardiovascular system. Clots initiated by roughened endothelial surfaces of a blood vessel resulting from atherosclerosis, which is induce adhesion of platelets. Intravascular clots may form when blood flows too slowly (stasis).
Clotting in an unbroken blood vessel is called thrombosis.
Thrombolytic agents are chemical substances that are injected into the body to dissolve blood clots to restore circulation. These agents activate plasminogen. Streptokinase, which is produced by streptococcal bacteria, is used to dissolve clots in order to restore circulation. A genetically engineered version of human tissue plasminogen activator (t-PA) treat victims of both heart attacks and brain attacks (strokes) that are caused by blood clots.
Blood Groups and Blood Types
The surfaces of erythrocytes contain genetically determined antigens of glycoproteins and glycolipids. The antigens are called agglutinogens. Based on the presence or absence of various antigens, blood is categorized into blood groups. Within a blood group there are different blood types. There are two major blood groups – ABO and Rh. The percentage of
ABO and Rh blood types varies among different races of humans, most humans are type O,
Rh + .
ABO Blood Group
ABO blood group is based on two glycolipid antigens, A and B on the RBCs. People whose
RBCs display only antigen A has type A blood. Those who have only antigen B are type B.
Those individuals who have both A and B antigens are type AB. Those individuals who have neither antigen A nor B are type O.
Blood plasma usually contains antibodies called agglutinin that react with the A or B antigens on the RBCs if the two are mixed. The anti-A antibody reacts with antigen A; the anti-B antibody reacts with antigen B. You do not have antibodies in your blood plasma that react with the antigens on your own RBCs. You do have antibodies in your blood plasma for any antigens that your RBCs lack. If your blood type is B, you have B antigens on your red blood cells, and you have anti-A antibodies in your blood plasma.
Transfusions
A transfusion is the transfer of whole blood or blood components from a donor into the blood of a recipient (patient). Antigens on the donor’s RBC cell membrane can trigger damaging antigen-antibody responses in a transfused recipient. During an incompatible blood transfusion, antibodies in the recipient’s plasma bind to the antigen on the donated RBC’s, which causes agglutination or clumping of the donated RBCs. Agglutination is an antigen-antibody response in which donate RBCs become cross-linked to one another. (Note that agglutination is not the same as blood clotting.) When antigen-antibody complexes form, they make the cell membrane
9
of the donated RBCs leaky, causing hemolysis (rupture) of the RBCs and the release of hemoglobin into the recipient’s blood plasma.
Consider what happens if a person with type A blood receives a transfusion of type B blood.
The recipient’s blood (type A) contains A antigens on the RBCs and anti-B antibodies in the plasma. The donor’s blood (type B) contains B antigens and anti-A antibodies. First, B antibodies in the recipient’s plasma can bind to the B antigens on the donor’s erythrocytes. causing agglutination and hemolysis of the incoming red blood cells. Second, anti-A antibodies in the donor’s plasma can bind to the A antigens on the recipient’s RBCs, a less serious reaction because donor’s anti-A antibodies become so diluted in the recipient’s plasma that they do not cause significant agglutination and hemolysis of the recipient’s
RBCs.
People with type AB blood do not have anti-A or anti-B antibodies in their blood plasma.
They are universal recipients because they can receive blood from donors of all four blood types. They have no antibodies to attack antigens on donated RBCs. People with type O blood have neither A nor B antigens on their RBCs and are universal donors because they can donate blood to all four ABO blood types. Type O persons may receive only type O blood.
Rh Blood Group
The Rh blood group is so named because the antigen was discovered on RBCs of the Rhesus monkey. People whose RBCs have Rh antigens are designated Rh + (Rh positive). Those individuals who lack Rh antigens are designated Rh does not contain anti-Rh antibodies. If an Rh however, the immune system of the Rh -
-
(Rh negative). Normally, blood plasma person receives an Rh + blood transfusion,
person start to make anti-Rh antibodies that will remain in the blood. If a second Rh + blood transfusion is given later, the previously formed antibodies will cause agglutination and hemolysis of the RBCs in the incoming donated blood.
Hemolytic Disease of the Newborn
The most common problem with Rh incompatibility, hemolytic disease of the newborn
(HDN), may arise during pregnancy if a small amount of Rh + blood leaks from the fetus through the placenta into the blood of an Rh mother. The mother will start to make anti-Rh antibodies. The firstborn baby usually is not affected. If the mother becomes pregnant again, however, her anti-Rh antibodies can cross the placenta and enter the blood of the fetus. If the fetus is Rh , there is no problem, because Rh blood does not have the Rh antigen. If the fetus is Rh +, however, agglutination and hemolysis may occur in the fetal blood.
An injection of anti-Rh antibodies called anti-Rh gamma globulin (RhoGAM) can be given to prevent HDN. All Rh women should receive RhoGam soon after every delivery. These antibodies bind to and inactivate the fetal Rh antigens before the mother’s immune system can respond to antigens by producing her own anti-Rh antibodies.
10
Typing and Cross Matching Blood for Transfusion
To avoid blood-type mismatches on transfusion, blood bank laboratory technicians first type the patient’s (recipient’s) blood, then cross-match it to potential donor’s blood, for the presence of antibodies. The procedure for ABO blood typing, single drops of blood are mixed with different antisera that contain antibodies. One drop of blood is mixed with anti-A serum containing anti-A antibodies that will agglutinate RBCs that possess A antigens.
Another drop is mixed with anti-B serum, containing anti-B antibodies that will agglutinate
RBCs that possess B antigens. If the RBCs agglutinate only when mixed with anti-A serum, the blood is type A. If the RBCs agglutinate only when mixed with anti-B serum, the blood is type B. If the blood is type AB both drops agglutinate; if neither drop agglutinates, the blood is type O. To determine Rh antigen a drop of recipient’s blood is mixed with antiserum containing Rh antibodies. If the RBCs agglutinate, the RBCs have Rh antigens on their cell membrane, the blood is Rh + . If the blood does not agglutinate, it is Rh . Once the patient’s blood type is known, donor blood of the same ABO and Rh type is selected.
In a cross-match donor RBCs are mixed with the recipient’s serum. If agglutination does not occur, the recipient does not have antibodies that will attack the donor RBCs.
11