Chapter 10 Blood
advertisement

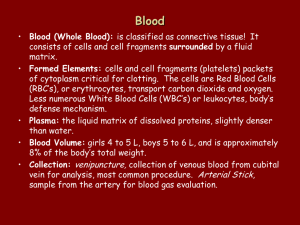
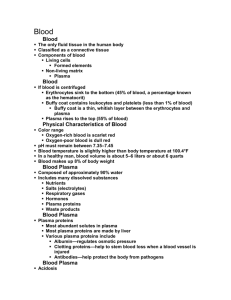
Chapter 10 Blood Blood is the "river of life" that surges within us. It transports everything that must be carried from one place to another within the body-nutrients, wastes (headed for elimination from the body), and body heat-through blood vessels. For centuries, long before modern medicine, people recognized that blood was vital (some believed "magical"), and its loss was always considered to be a possible cause of death. In this chapter, we consider the composition and function of this life-sustaining fluid. The means by which it is propelled throughout the body is discussed in Chapter 11. Composition and Functions of Blood Indicate the composition and volume of whole blood. o Being the only fluid tissue, blood contains both a complex connective tissue in which living blood cells, the formed elements, are suspended in a nonliving fluid matrix called plasma Contains – water, salts, plasma proteins, nutrients, waste products, respiratory gases, hormones, red blood cells, white blood cells, platelets Blood accounts for ~8% of body weight - ~6 quarts in a healthy male Describe the composition of plasma and discuss its importance in the body. o Plasma – 90% water – dissolved substances include nutrients, metal ions (salts), respiratory gases, hormones, plasma proteins, and various wastes and products of cell metabolism Plasma proteins – most abundant solutes in plasma – except for antibodies and protein-based hormones, most plasma proteins are made by the liver Albumin – contributes to the osmotic pressure of blood, acting to keep water in the bloodstream Clotting proteins – help stem blood loss when blood vessels are injured Antibodies – help protect the body from pathogens Plasma proteins are not taken up by cells to be used as food fuels or metabolic nutrients unlike other solutes such as glucose, fatty acids, and oxygen List the cell types making up the formed elements and describe the major functions of each type. o Erythrocytes – small, biconcave disks with depresses centers – red blood cells – ferry oxygen in blood cells to all cells in the body – anucleate (no nucleus when mature) with very few organelles Hemoglobin – iron-containing protein that transports the bulk of oxygen carried in the blood and to a lesser degree, carbon dioxide Each RBC contains ~250 million hemoglobin molecules, each capable of binding 4 molecules of oxygen No mitochondria so make ATP vie anaerobic mechanisms so they don’t use the oxygen they carry o Leukocytes – white blood cells – crucial to body defense against disease (bacteria, viruses, parasites, tumor cells, dead cells) – less than 1% of total blood volume – the only complete cells in blood with a nucleus and the usual organelles Not confined to the blood vessels like RBC are – are able to slip out of blood vessels via diapedesis to get to areas of tissue damage and infection – respond to chemicals that diffuse from the damaged cells in a process called positive chemotaxis – move to the area by ameboid motion following the diffusion gradient Granulocytes – granule-containing WBCs – lobed nuclei, which consist of several rounded nuclear areas connected by thin strands of nuclear material – granules stain with Wright’s stain Neutrophils – have a multilobed nucleus and very fine granules that respond to both acid and basic stains and the cytoplasm stains pink – phagocytes at sites of acute infection Eosinophils – blue-red nucleus and brick-red cytoplasmic granules – numbers increase during allergies and infections by parasitic worms Basophils – contain large histamine-containing granules that stain dark blue – histamine is an inflammatory chemical that makes blood vessels leaky and attracts other WBCs to the site Agranulocytes – lake visible cytoplasmic granules with normal looking nuclei Lymphocytes – large dark purple nucleus that occupies most of the cell volume – live in lymphatic tissue where they help in immune responses Monocytes – abundant cytoplasm and indented nucleus – change into macrophages to fight chronic infections such as tuberculosis o Platelets – not cells but fragments of multinucleate cells called megakaryocytes, which rupture, releasing thousands of anucleate pieces that quickly seal themselves off from surrounding fluids – appear as darkly staining, irregularly shaped bodies scattered among the other blood cells – normal platelet count is 300,000/mm3 – needed for the clotting process that occurs when blood vessels are broken Define anemia, polycythemia, leucopenia, and leukocytosis, and list possible causes for each condition. o Anemia – a decrease in the oxygen-carrying ability of the blood for any reason – a lowerthan-normal number of RBC or abnormal or deficient hemoglobin content in the RBCs such as sickle-cell anemia o Polycythemia – an excessive or abnormal increase in the number of erythrocytes – may result from bone marrow cancer or a normal physiological response to living at high altitudes where air is thinner and therefore less oxygen is available – excessive RBCs increases blood viscosity causing it to flow sluggishly in the body and impairs circulation o Leukocytosis – a total WBC count above 11,000 cells/mm3 – generally indicated that a bacterial or viral infection is stewing in the body Explain the role of the hemocytoblast. o All the formed elements arise from this common type of stem cell in a process called hematopoiesis that occurs in red bone marrow, or myeloid tissue Development differs for each type but once the cell is committed to a specific blood pathway, it cannot change Hemocytoblasts form two types of descendants that form all the other cells – lymphoid stem cells that result in lymphocytes and myeloid stem cells that result in all other types Rate of erythrocyte production is controlled by the hormone erythropoietin produced primarily by the kidneys and less by the liver Rate of leukocytes is stimulated by the hormones colony stimulating factor and interleukins, which are stimulated by chemical signals sent out by cells in danger Rate of platelets is accelerated by the hormone thrombopoietin Hemostasis Describe the blood-clotting process. o See figure 10.6 on page 316 o Platelet plug forms – platelets become sticky and cling to the damaged site and anchored platelets release chemicals that attract more platelets to the site so that a small mass called a platelet plug or white thrombus is formed o Vascular spasms occur – the anchored platelets also release serotonin which causes that blood vessel to go into spasms that narrow the blood vessel at that point, decreasing blood loss until clotting can occur o Coagulation events occur The injured tissues are releasing thromboplastin, a factor that plays a role in clotting PF3, a phospholipid that coats the surfaces of the platelets, interacts with thromboplastin, other blood protein clotting factors, and calcium ions (Ca 2+) to form an activator that triggers the clotting cascade This prothrombin activator converts prothrombin that is present in the plasma to thrombin, an enzyme Thrombin then joins soluble fibrinogen proteins into long hair-like molecules of insoluble fibrin, which forms a meshwork that traps the RBCs and forms the basis of the clot Within the hour, the clot begins to retract, squeezing serum (plasma minus the clotting proteins) from the mass and pulling the ruptured edges of the blood vessel closer together Name some factors that may inhibit or enhance the blood-clotting process. o Undesirable clotting – sometimes form in intact blood vessels, especially those in the legs – a clot that develops and persists in unbroken vessels is called a thrombus and if it is large enough, it may prevent blood flow to the cells beyond the blockage – may be caused by anything that roughens the endothelium of a blood vessel and encourages clinging of platelets such as burns, physical blows, or an accumulation of fatty material – treated with anticoagulants such as aspirin, heparin, and dicumarol If the clot is in the heart, a heart attack may occur killing heart tissue and/or the person If a thrombus breaks away from the vessel wall and floats freely in the blood stream, it becomes an embolus, which if it lodges in a small vessel in the brain could result in a cerebral embolus and cause a stroke Slowly flowing blood or blood pooling is another problem especially in immobilized patients because clotting factors are not washed away as usual and so they accumulate o Bleeding disorders – usually caused by platelet deficiency and deficits of clotting factors Thrombocytopenia – results from an insufficient number of platelets resulting in normal movements causing spontaneous bleeding from small blood vessels showing up as small purplish blotches called petechiae on the skin – can arise from any condition that suppresses myeloid tissue such as bone marrow cancer, radiation, or certain drugs Vitamin K deficiency – when the liver is unable to make its usual supply of clotting factors, abnormal bleeding may result as vitamin K is needed to make clotting factors – treated with vitamin K or with whole blood transfusions when the liver function is severely impaired Hemophilia – hereditary bleeding disorder – results from a lack of any of the factors needed for clotting – even minor tissue trauma results in prolonged bleeding and can be life-threatening – repeated bleeding into joints causes them to become disabled and painful – treated with transfusion of fresh plasma or injections of purified clotting factors they lack Blood Groups and Transfusions Describe the ABO and Rh blood groups. o ABO blood groups are based on which of two antigens, type A or type B a person inherits – absence of both antigens results in type O blood while presence of both antigens results in type AB blood, only A or B antigens leads to either type A or type B blood Antibodies are formed during infancy against the ABO antigens not present in your own RBCs o Rh blood groups – so named because one of the eight Rh antigens (agglutinogen D) was originally identified in Rhesus monkeys Rh+ people have RBCs that carry the Rh antigen while RH- people do not carry the Rh antigen Anti-Rh antibodies are not automatically formed and present in the blood of Rh people but once an Rh- individual receives Rh+ blood, their immune system begins producing antibodies so the second time they receive the wrong blood type, hemolysis (rupturing of the RBCs) will occur When an Rh- woman is carrying an Rh+ fetus the first time there is usually no problems and a healthy baby is delivered but the mother becomes sensitized to the Rh+ antigens that have passed through the placenta into her bloodstream and she will produce anti-Rh+ antibodies unless treated with RhoGAM shortly after giving birth RhoGAM is an immune serum that prevents the sensitization and her immune response If no treatment is given, and she becomes pregnant again with another Rh + baby, her antibodies will cross the placenta and destroy the baby’s RBCs, which produces a condition known as hemolytic disease of the newborn where the baby is anemic and hypoxic resulting in brain damage or the death of the baby Explain the basis for a transfusion reaction. o It is important to determine the blood group of both the donor and the recipient before blood is transfused because agglutination could occur killing the recipient o The plasma membranes of RBCs bear genetically determined proteins (antigens, which is a substance that the body recognizes as foreign and stimulates the immune system to release antibodies against it), which identify each person as unique therefore another person’s RBCs with foreign antigens on them will be attacked by the recipient’s immune system Agglutination occurs when the binding of the antibodies causes the RBCs to clump, which leads to the clogging of small blood vessels throughout the body The donor RBCs are lysed and their hemoglobin is released into the bloodstream where the released molecules could block the kidney tubules and cause kidney failure – treatment is aimed at preventing kidney damage by infusing alkaline fluids to dilute and dissolve the hemoglobin and diuretics to flush it out of the body in urine o The Rh factor must also match between the donor and recipient to further reduce the danger to the recipient Developmental Aspects of Blood Explain the basis of physiologic jaundice seen in some newborn babies. o Fetal hemoglobin (HbF) differs from the hemoglobin formed after birth in that fetal hemoglobin has a greater ability to pick up oxygen – after birth fetal blood cells are gradually replaced by RBCs that contain the typical hemoglobin A (HbA) o Physiologic jaundice occurs when the fetal RBCs are destroyed at such a rapid rate that the immature infant liver cannot rid the body of hemoglobin breakdown products in the bile fast enough Indicate blood disorders that increase in frequency in the aged. o Iron-deficiency anemia is common in women because of their monthly blood loss during menses o The young and old are particularly at risk for leukemia o With increasing age, chronic types of leukemia, anemia, and diseases involving undesirable clot formation are more prevalent, however, these are usually secondary to disorders of the heart, blood vessels, or immune system o The elderly are particularly at risk for pernicious anemia because the stomach mucosa (which produces intrinsic factor) atrophies with age