Lab 4
advertisement
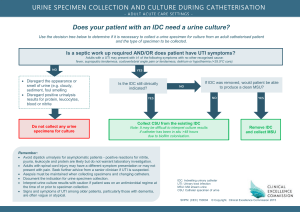
URINE CULTURE LAB Objectives: 1. Predict what organisms are likely to cause urinary tract infection 2. Distinguish between bacteria that are potential urinary tract pathogens and those that are not 3. List the normal urethral flora of the male and female\ 4. Describe the different types of urine specimens received in the laboratory and proper collection methods 5. Explain how to perform a quantitative urine culture 6. Explain how to interpret colony counts from the different specimen types 7. Describe how to work up bacteria with different colony counts from clean catch urine specimens 8. Explain the proper technique for gram staining urine and how to interpret the information derived from the stain 9. Explain the significance of low colony counts in urine specimens from symptomatic females Introduction The urinary tract is composed of the kidneys, ureters, bladder, and urethra. Infection of the lower urinary tract involves the bladder (cystitis) and the urethra (urethritis). Infection of the upper urinary tract involves the kidnes (pyelonephritis). Cystitis is the most common type of urinary tract infection (UTI) and occurs most frequently in women. It is usually caused by Escherichia coli and other members of the Enterobacteriaceae, which come from the individual’s own fecal flora. These organisms colonize the urethra and then ascend upward and infect the bladder. The exception is infection caused by Staphylococcus saprophyticus . This organism is a common cause of UTI in young females, but its reservoir has not been firmly established. Pyelonephritis usually occurs as a complication of cystitis when bacteria ascend the ureters from the bladder and invade the kidney. UTI is usually caused by only on organism, and mixed infections are rare. Symptoms of cystitis are urgency, frequency, dysuria (painful urination) and hematuria (bloody urine). Symptoms of pyelonephritis are chills, fever and flank pain. UTI is accompanied by bacteriuria (bacteria in the urine) and pyuria (leukocytes in the urine). UTI can sometimes by asymptomatic, which is called asymptomatic bacteriuria. The diagnosis of UTI is performed by culturing urine, with is normally sterile. The results of urine cultures are sometimes difficult to interpret because urine flows through the urethra, which is inhabited by normal flora that can contaminate urine specimens. In the female the normal urethral flora consist of diphtheroids, lactobacilli, coagulase-negative staphylocci, alpha streptococci and low numbers of Enterobacteriaceae. Lactobacilli, alpha streptococci, and diphtheroids are not urinary pathogens, but Enterobacteriaceae are potential urinary tract pathogens. The first protion of normally voided urine can contain up to 103 organisms per ml of noral urethral flora; therefore, especially in the female, the presence of members of the Enterobacteriaceae could indicate either contamination of infection. For this reason, guidelines using bacterial counts have been established to aid interpretation. These guidelines suggest that bacterial counts of more than 103 colony-forming units per milliliter (CFU.ml) indicate infection, and lower counts represent possible contamination. The guidelines are based on studies that show that UTI is associated with high numbers of bacteria in the urine infection, and lower counts represent possible contamination. The guidelines are based on studies that show that UTI is associated with high numbers of bacteria in the urine. The term significant bacteriuria is defined as bacteria in the urine in numbers greater than 105 CFU/ml. In the male, the normal urethral flora consists of diphtheroids, coagulase-negative staphylococci, and Enterococcus species. Normal urine can contain low numbers of these organisms, and guidelines described for females are also used to interpret urine cultures from males. Pathogens In nonhospitalized patients, the most common causes of UTI are: E. coli (most common), Klebsiella species, other Enterobacteriaceae, and S. saprophyticus. Streptococci and Yeast may also frequently be isolated. In hospitalized patients, the most common causes are E. coli (most common), Klebsiella species, Proteus species, other Enterobacteriaceae, Pseudomonas aeruginosa, and Enterococcus species Normal flora: Diphtheroids Alpha-streptococci Lactobacilli Coagulase-negative staphylococci E. coli and other Enterobacteriaceae Enterococcus species Specimen Types and Collection It is extremely critical that urine specimens be collected to avoid urethral contamination. There are several types of urine specimens, and the results of each type are determined by different guidelines. Therefore, it is essential that each urine specimen received by the laboratory be labeled as to the type of urine specimen. Clean catch Midstream Urine (routine, voided, ccm) The clean-catch is the most common type of urine specimen. The technique involved in collection is based on discarding the first portion of urine, which is most likely to be contaminated. It is recommended that the first voided morning specimen be collected so bacteria will have multiplied to high levels after overnight incubation in the bladder. ;if this is not possible, the urine should be allowed to incubate in the bladder as long as possible before collection. Indwelling catheter or Foley catheter Hospitalized patients who have indwelling or foley catheters are especially at risk for developing UTI. To avoid contamination, collect specimens by disinfecting a portion of the catheter tubing with alcohol. Puncturing the tubing directly with a sterile syringe and needle, and aspirating the urine. Place the specimen in a sterile container. Urine should never be collected from the drainage bag. Suprapubic Aspirate The suprapubic aspirate technique avoids urethral contamination but is invasive. It is usually reserved for infants, from whom it is difficult to obtain urine specimens. In this procedure, the skin above the bladder is disinfected and sterile needle and syringe are plunged into the bladder. Urine is aspirated and placed in a sterile container. Cystoscopy specimens Cystoscopy specimens are collected from the bladder or kidneys during cystocopy and avoid urethral contamination. Specimens transport Because urine is an excellent culture medium for bacteria, urine specimens must be sent to the laboratory as soon as possible. Specimens should be plated within 2 hours of collection or bacterial counts will not be valid. If this is not possible the specimen may be refrigered for a maximum of 24 hours before plating. Specimen processing Quantitative Cultures Quantitative cultures should be performed on all urine specimens so that the number of bacteria per milliliter of urine can be determined and expressed as CFU/ml. The most common method uses a calibrated platinum loop that delivers 0.001 ml or 0.01 ml of urine. Each plate is inoculated with one loopful of urine, and the colony count is determined by multiplying the number of colonies by the dilution factor. For example, if a 0.001 ml loop is used and 10 colonies are observed, the colony count would be 10 x 10000 or 10,000 CFU/ml (104 CFU/ml). If a 0.01 ml loop is used and 10 colonies are observed, the colony count would be 10 x 100 or 1000 CFU/ml (103 CFU/ml). Use the following procedure to perform a quantitative culture of urine sing a calibrated loop 1. Mix the urine well 2. Vertically insert a flamed and cooled calibrated loop into the specimen and immerse it just below the surface of the specimen. Only move the loop straight up and down 3. Remove a loopful of urine and inoculate each plate by making a straight line down the center and then a series of close perpendicular streaks throught the first line. Inoculate each plate with one loopful of urine Primary plates Inoculate the following media using a calibrated loop and incubate in an aerobic incubator for 24 hrs 1. Sheep blood agar 2. MacConkey or eosin-methylene blue (EMB) agar plate Interpretation of Culture Results To determine whether bacteria isolated from urine cultures are contaminants or clinically significant agents of UTI that should be worked up (id and AST), criteria must be considered, including the identity of the isolate, the number of bacterial types, the type of specimen, and the colony count. Type of organism Lactobacillus speices, alpha-stretococci, dna diphtheroids are not associated with UTI and should not be identified or have susceptibility tests performed. They are regarded as urethral or skin contaminants, no matter withat their colony count. Number of bacterial type 95% of all UTI infection are caused by one type of organism, and it is unlikely that 2 organisms are involved. It is almost impossible that 3 organisms are involved. Cultures containing 3 organisms are generally considered to be contaminated. Colony Counts and specimen type Suprapubic and Cystoscopy specimens Because suprapubic and cystoscopy specimens are collected by methods that by pass the urethra, contamination is unlikely. Perform identification, report colony counts, and perform susceptibility testing on all isolates (unless 3 or more are present, which indicates probable contamination) Clean catch or indwelling catheter specimens Because clean catch or indwelling catheter specimens are collected through the urethra, the urine is likely to be contaminated by normal urethral flora, and the colony counts are necessary for interpretation of culture results. In general, counts less than 104 CFU/ml indicate contamination, counts of 104 -105 CFU/ml indicate possible infection, and counts greater than 10 CFU/ml indicate significant bacteriuria and probable infection. Symptomatic Urinary tract infection in females with low bacterial colony counts There is a subpopulation of women who have symptomatic UTIs but whose urine cultures are negative (no growth) or have colony counts as low as 102 CFU/ml. this condition has been referred to as acute urethral syndrome. It is now known that these women have true bladder infections caused by low counts of bacteria. To diagnose these UTIs, it is necessary for the physician to alert the microbiology lab to work up bacteria with low counts. See ASM guidelines for Interpretation of Urine colony count Screening methods There are several screening methods available to detect urine specimens containing high levels of bacteriuria and pyuria. Gram stain of Uncentrifuged urine: The gram stain is the easiest and most sensitive screening method. One drop of uncentrifuged urine is placed on a slide and allowed to dry without spreading. The slide is than gram stained and examined under oil immersion. The presence of one or more bacterial per oil immersion field correlates with a bacterial count of greater than 105 CFU/ ml. the presence of one or more PMNs per oil immersion field indicates pyuria. The gram stain cannot detect bacterial counts of less than 105 CFU/ ml. Leukocyte esterase and dipstick Nitrate test The leukocyte esterase test detects pyuria, which correlates with bacteriuria. The test identifies the presence of the enzyme leukocyte esterase which is produced by leukocytes. The sensivitiy of the LE dipstick test can be increased by combining it with the nitrate test. The nitrate test detects the presence of nitrite in the urine, which theoretically correlates with the presence of members of the Enterobacteriaceae, which reduce nitrate to nitrite. The nitrate test is not sensitive enough to be used alone. Study Questions 1. How would you work up the following results from aclean catch urine plated with a 0.001 ml loop? A. 5 colonies of a gnr (1 type) B. 15 colonies of a gnr ( 1 type) C. 150 colonies of a gnr (1 type) D. 10 colonies: 5 colonies each of 2 different types of gnr E. 50 colonies: 25 colonies each of 2 types of gnr F. 150 colonies, 50 colonies each of 3 different organisms G. 120 colonies: 75 colonies of a gnr, 45 colonies of a gpc H. 100 colonies: 95 colonies of a gnr and 5 colonies of a gpc 2. What are the most common organisms causing urinary tract infections? 3. What bacteria make up the normal urethral flora 4. How long can a urine specimen site before it is plated? What can be done if it cannot be plated within this time period?