Behavior Management Plan (BMP):
advertisement

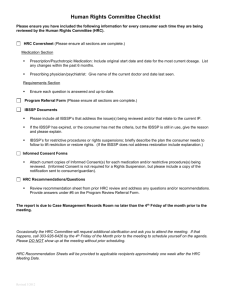
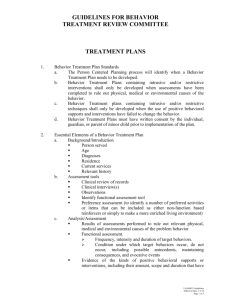
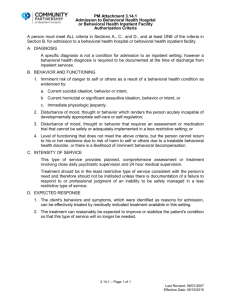
UNITY HOUSE OF CAYUGA COUNTY INC. BEHAVIOR PLAN POLICY 10/26/09 Updated 7/1/12; 3/22/13; 5/15/13 Policy It is the policy of Unity House to empower staff with the tools to effectively manage challenging behavior. It is the intent of Unity House to encourage and permit the full exercise of individual rights. There are instances when an individual threatens to harm or is dangerous to him/her, others, or property and it may be in the best interest of the individual to restrict movement or privileges. All staff with direct care responsibilities and their supervisors will be trained in emergency procedures (SCIP-R) within three months of their hire date. This policy will provide consistent procedures for the development and implementation of behavior plans that incorporate restrictive interventions and the development and implementation of behavior guidelines designed to assist the staff in effectively managing challenging behaviors on an individual basis. This policy emphasizes the utilization of non-restrictive procedures to address the behavioral needs of consumers. Table of Contents I. II. III. Behavior Support Plans Behavior Monitoring Plans Human Rights Committee a. HRC and ICC Process P. 2 P. 2 P. 3 P. 4 Criteria (Administrative Memorandum April 1, 2013 Person-Centered Behavioral Intervention) Functional Behavioral Assessment (functional assessment or functional analysis of behavior) must be conducted before a behavior support plan is developed. Functional Assessment must be completed by a clinician with training in assessment techniques. Behavior support/monitoring plans must be developed by a licensed psychologist or applied behavior sciences specialist, LCSW. Behavior management support plans will contain all the elements identified in the 04-01-13 OPWDD Administrative Memorandum. Plans must be reviewed by the HRC for clinical soundness, and alignment with PWDD regulation for restrictive plans. Support team with the clinician will review the plans semi-annually. All staff will receive training specific to the behavioral support plan before it is implemented. 1 Tools & Resources April 1, 2013 OPWDD Administrative Memo: Person-Centered Behavioral Intervention Behavior Data tracking form HRC Review form BSP/Monitoring Plan format document Procedures Behavior Support Plan (BSP): A behavior support plan is created to modify a person’s challenging behavior in order to increase his/her quality of life. A BSP includes pro-active and re-active (or rights restrictive) techniques for addressing the target behavior during a crisis. For the Behavior Support Plan format, see Appendices. When a prescription is written for a PRN medication that will alter a consumer’s behavior, the Program Manager in conjunction with the Program RN will develop administration guidelines for that PRN medication only (see Nursing Policy 200.8 Guidelines for the Administration of PRN Behavior Changing Medications). The Program Manager will be responsible for ensuring the PRN is identified in the IPOP. The administration guidelines will be included in the Behavior Support Plan that is developed and reviewed per this policy. A functional behavioral assessment must be completed by a clinician prior to the development of a behavior support plan. The plan needs to specifically include a description of the target behavior and include a hierarchy of behavioral approaches, strategies and supports to address the behavior(s) requiring intervention, with preferred methods being positive approaches, strategies and supports, include a plan for alternative adaptive behaviors, provide a methods for collection of behavioral data and a schedule to review the effectiveness of the plan. The behavior support plan must be developed by a clinician with training in behavior management techniques. All rights restrictive/intrusive behavior support plans are reviewed by the Unity House Behavior Management Committee. All plans are reviewed at least semi-annually by the plan author, in conjunction with the support team. Behavior Support Plans are maintained for 10 years. For specific information on purging and filing BSP’s, see the Historical File Policy. Behavior Monitoring Plan (BMP): A Behavior Monitoring Plan identifies the target symptoms of a diagnosed co-occurring psychiatric disorder which are to be prevented, reduced or eliminated. The plan shall specify interventions that will be used to address associated challenging behaviors that may occur and methods by which progress in symptom control and functional improvement will be measured, documented, and reviewed. 2 A functional behavioral assessment is not required for a Behavior Monitoring Plan; however, the Monitoring Plan must be completed by a clinician such as licensed psychologist, LCSW or Behavioral Intervention Specialist. All plans are reviewed at least semi-annually by the plan author, in conjunction with the support team. Behavior Support Plans are maintained for 10 years. For specific information on purging and filing BSP’s, see the Historical File Policy. The following types of Behavior Support/Monitoring Plans need to be reviewed by the HRC: Highly Restrictive plans which include: Restriction of rights; exclusionary timeout; required (forced) relaxation; and restrictive personal interventions as identified in the SCIP-R policy Minimally restrictive plans which include: planned ignoring; special supervision; locking devices; overcorrection; response cost; non-exclusionary time out; escorts; mechanical restraining devices; and psychotropic medication except for monitoring plans in which medication is used solely for the treatment of a cooccurring diagnosed psychiatric condition. Human Rights Committee: It is the policy of Unity House that all restrictive/intrusive behavior plans are reviewed by the Unity House Human Rights Committee. The HRC consists of a minimum of four members and must have a psychologist or BIS, a clinician, licensed, certified or registered in NYS, and an advocate, consumer, guardian or family member preferable with no ownership, relationship or interest in the agency. At least three of these participants must be available to approve a plan. The purpose of the Unity House HRC is to determine if the quality of the individual’s life is likely to be enhanced or made worse by the BSP’s implementation. The committee must verify that all required components are included in the BSP. The committee chair will verify that approval does not exceed 1 year and that written informed consent is obtained prior to the implementation of that approved BSP. The committee must specifically review plans that include the use of mechanical restraining devices that are not commercially available or modifications of available devices and any modifications of intermediate and restrictive physical intervention techniques. The committee shall review and make suggestions to the agency’s management and/or governing body about its policies, practices and programs as they relate to behavioral support. The IRA program manager and site nurse in conjunction with the plan author will collect and review behavioral data quarterly. The plan must be reviewed at each service plan review and updated accordingly (at least semi-annually). The program manager is responsible for ensuring this occurs. 3 Unity House HRC and ICC Process: There are seven documents that need to be submitted for approval. These documents need to be submitted for HRC and ICC, just HRC, or just ICC approval. Those documents are as follows: 1. Unity House HRC review form (see Appendices) 2. Capacity to give informed consent (see informed consent policy) 3. Informed consent for treatment (see informed consent policy) (make sure all restrictive interventions are listed, not just medications) 4. Behavior Support Plan 5. One year behavior data: Summarize behavior data in a monthly format, do not send all behavior data tracking or dates of each time target behavior was observed, overview of target behavior and progress only 6. Two year psychotropic medication history: Only include psychotropic medication history and DO NOT just print history from Foothold. List date, change and reason for changes to psychotropic meds 7. Most recent psychiatry consultation report NOTE: To obtain the “Capacity to Give Informed Consent” (#2) and Informed Consent for Treatment (#3), please refer to Unity House Informed Consent Policy. Once all the previously identified documents are gathered, the Program Manager is responsible for sending them to the HRC. The Program Manager will be identified as the primary contact person. Once the committee has responded, the Program Manager will be responsible for sending copies of the plan to all involved parties (parents, service coordinator, Day Hab, Employment…). 4