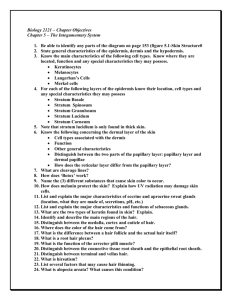
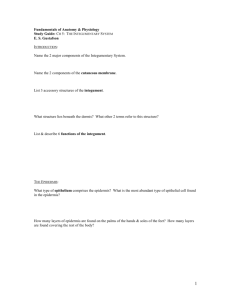
Block 2 Unit 1 Objectives
advertisement

© 2008 Mark Tuttle Integument – Crissman 1. List and describe the morphology and functions of the layers in the skin. a. Epidermis i. Most superficial layer; composed of stratified squamous keratinized epithelial tissue, derived from ectoderm, avascular and consists of 5 well-defined layers. The epidermis is hard, can be sloughed off and readily replenished, can protect the underlying tissues from damage and invasion, etc. b. Dermis i. Deepest layer of the skin; composed of connective tissues and fibers, blood supply is located here, glands and hair follicles extend down to this layer, etc. The dermis is derived from mesenchyme. c. Hypodermis i. Not actually a part of skin, but often discussed with it. The hypodermis is actually the subcutaneous fascia and is made up of loose areolar connective tissue. There is often a great deal of fat stored in this layer – subcutaneous fat is called panniculus adiposus. 2. List and describe the morphology and arrangement of the layers and components in the epidermis, dermis and hypodermis. a. Epidermis (5 Layers): Pages 28-29. b. Dermis (2 Layers, Vascularized): Pages 38-40 (section B). c. Hypodermis: Described in previous objective. 3. List and describe the morphological and functional changes in epidermal cells as they move from the basal lamina to be sloughed off at the surface of the stratum corneum. a. Epidermal cells are called keratinocytes. They begin their journey to the surface from the stratum basale (germinativum), which is directly superficial to the basal lamina. b. The cells in the stratum basale are arranged in a single layer and are cuboidal to columnar in shape. It is this layer in which mitosis is primarily occurring. Small bundles of keratin, called tonofilaments or cytokeratin, first appear in this layer. These cells have desmosomes to attach to each other and hemidesmosomes to attach to the basal lamina. The primary function of this layer is proliferation. c. The cells in the stratum spinosum are arranged in several layers and are irregularly shaped. The cells are crossed by intercellular bridges (desmosomes) that are visible in preparation because the processing leads to shrinkage of these cells away from one another. The spaces that appear between the cells are crossed by these intercellular bridges, which look like spines. The large number of desmosomes in this layer helps hold the cells together in a unified sheet. This layer produces more keratin, which begins to fill the cytoplasm. The tonofilaments become organized into bundles called tonofibrils. Lamellar granules also appear in the cytoplasm – these are membrane-bound packets of light and dark bands that are extruded as the cells approach the next layer. d. The cells in the stratum granulosum are arranged in a narrow layer that is approximately 3-5 cells thick. The cells in this layer are more flattened and the nuclei have begun to disappear © 2008 Mark Tuttle due to lack of nutrients. They stain darker due to the presence of numerous keratohyalin granules (not membrane-bound). The lamellar granules extruded from the cells as they enter this layer release a substance rich in glycolipids that surrounds the cells. This hydrophobic secretion forms a waterproof barrier between the cells – this also increases the intercellular space between cells. The tonofibrils are crosslinked by a protein called filaggrin in this layer. Involucrin, produced in the stratum spinosum, is crosslinked onto the cell membrane by the enzyme transglutaminase. This leads to the cell membrane becoming water impermeable, hastening cell death. e. The cells in the stratum lucidum are arranged in a thin layer that is 2-3 cells thick. Neither the individual cells nor the nuclei are visible, giving this layer a transparent (clear) appearance. This layer is actually the lower portion of the stratum corneum. The cells in this layer, which at this point are dead, are accumulating even more keratin in increasingly complex forms (such as eliden, a transformed keratohyalin granule). f. The cells in the stratum corneum are arranged in a very thick layer of dead cells that are completely filled with keratin. There are no visible nuclei in this layer, and these cells are sloughed off from the surface at reasonable regularity. The cells here are flattened and are called squames. They are arranged in tight proximity to one another to help facilitate the watertight barrier of the epidermis. The plasma membrane in this layer is also thickened with non-keratinous material, and no granules are visible in the squames. g. The stratum basale and spinosum are collectively known as the Stratum Malpighi. 4. List and describe the morphology and function of all cells in the epidermis. a. Keratinocytes are the principle cell type of the epidermis; they produce keratin and are derived from ectoderm. They change substantially as they process from the deepest layers up to the surface, and are responsible for maintaining the waterproof barrier of the epidermis. b. Melanocytes are the pigmented cells of the epidermis, and are found in the stratum basale with their processes projecting between neighboring cells. They are derived from the neural crest, and are involved in the conversion of tyrosine to melanin through a series of reactions using the enzyme tyrosinase. They are known as “clear cells” in light microscopy because they have no desmosomes and can form clear regions around themselves during preparation. There are approximately 800-1000 of these cells per mm2 in normal skin (1 in every 10 epidermal cells) and 2000 per mm2 in pigmented skin (about 1 in ever 4 epidermal cells). Pigmented skin is located on the face, forehead, areola and genitals. c. Langerhans cells are immune cells that are scattered throughout the stratum spinosum. They are stellate in shape and have many processes which project between neighboring cells (thus they are often called dendritic cells). They move freely within the stratum spinosum and are antigen presenting cells (they present antigens to T-helper cells) during hypersensitivity reactions such as contact dermatitis. d. Merkel cells are small, clear cells in the stratum basale. They contain dense core vesicles and are similar to the cells in the adrenal medulla (but do not contain catecholamines). They are individually innervated are function as slow-adapting cutaneous mechanoreceptors responsible for some of the sensation of light touch. © 2008 Mark Tuttle 5. Describe the morphology of the epidermis / dermis junction and its functional significance. a. The epidermal-dermal junction is irregular (not flat) due to dermal papillae, which interdigitate with the epidermal pegs and / or ridges, preventing shearing forces from separating the two layers. b. In thick skin, the primary dermal ridges are divided into 2 secondary ridges by the Interpapillary pegs (rete pegs) of the epidermis. Dermal papillae extend up from the secondary ridges and cause even more interdigitation (see page 40). c. In thin skin, there are simple rounded bumps or mounds of connective tissue extending up into small recesses in the epidermis. d. The primary dermal ridges correspond to the epidermal ridges that you can see on your fingers and toes (friction ridges). These improve grip and can be studied in forensic medicine and criminology using the science of dermatoglyphics. 6. Define and describe the cleavage lines of Langer and their clinical significance. a. These are the predominant directions of the bundles of collagen fibers in the reticular layer of the dermis in a region of the body. They are clinically important because in surgery (especially plastic surgery), if the incision is made parallel to LL (Langer lines), the wound will not gap open. If the incision is made across these cleavage lines, the wound will gap open and leave a large scar. b. See page 41. 7. Describe the arrangement of the blood supply to the skin and relate it to temperature regulation. a. The blood supply of the skin is arranged in three longitudinal plexuses, which run parallel to the surface of the skin primarily. The subcutaneous plexus is the deepest and is located in the subcutaneous fascia (hypodermis). The cutaneous plexus is located at the dermalsubcutaneous junction. The subpapillary plexus is located in the papillary layer of the dermis and contains capillary loops which run up into the individual dermal papillae. b. In skin, you have A-V shunts (glomuses) that run parallel to the capillaries-- a coil of small vessels running from the arterioles to the venules that connect the two most superficial plexuses. c. When partially closed (as occurs normally), blood will run up near the surface in moderate amounts, maintaining current temperature conditions of the body. d. In high temperatures, partial dilation occurs so blood can reach the surface and release heat. e. Cold temperatures cause sympathetic innervation to fire, clamping down on AV shunts so the blood cannot reach the surface. f. Apical skin: Covers ears, nose, etc. Process above occurs. In Non-Apical skin, there are no AV shunts: sympathetic nervous system causes release of norepinephrine, which prevents blood from reaching surface. In warm temperatures, acetylcholine release causes vasodilation. 8. List and describe the functions of the skin. a. The functions of the skin are listed on pages 27-28. 9. Integrate the morphology of the skin to its functions. © 2008 Mark Tuttle 10. 11. 12. 13. 14. a. Mechanical protection and maintenance of body fluids are provided by the junctions between cells, the numerous layers of cells and the secretions of hydrophobic materials into the intercellular spaces that help keep water out. This also helps prevent bacteria and other harmful agents from entering the body. b. Maintenance of body temperature is accomplished by sweat glands (water at the surface evaporates, cooling the body), blood vessels (AV shunts) and by adipose tissue (which provides insulation). c. The synthesis of vitamin D is accomplished by converting cholesterol in the superficial layers to precursors of the vitamin, which are transported to the liver and converted to another precursor, which is transported to the kidneys to finally produce vitamin D. d. Immunity is afforded by the Langerhans cells and by the ability of other wandering cells to enter the dermis and provide immunity. e. Sensory innervation and receptors provide us with feedback on stimuli of our environment and innervation along with vasculature change the appearance of the skin (embarrassment, cyanosis, jaundice, age and nerve damage). f. Repair is afforded by the ability of healing cells to come from the vasculature to the epidermis. List and describe the arrangement and location of skin appendages (hair, glands, nails). a. Hair covers most of our body and is located in hair follicles which extend down into the dermis and hypodermis. b. Glands are located in many places in our body in the skin and either insert into hair follicles or develop as invaginations of the epidermis into the dermis. c. Nails are produced at the distal ends of each of our 20 digits and are modified epithelial structures. List and describe the arrangement of the parts and layers of the hair and hair follicle. a. See section IV-A, pages 43-45. Relate the layers of the epidermis to those of the hair follicle and nails. a. Hair follicle: The external root sheath is an extension of the strata basale and spinosum down around the hair follicle. b. The matrix of the follicle is the equivalent of the stratum basale. c. Nails: The nail bed is continuous with the stratum basale & granulosum of the epidermis, while the nail plate is a structure that replaces the stratum corneum in the nail (these keratinocytes are full of hard keratin, while normal stratum corneum is full of soft keratin). Define and describe terminal, vellus and lanugo hair; give their distribution over the body. a. Terminal hairs are hard, large, coarse, long and dark – they cover the scalp and eyebrows, as well as the genital areas and are more common on males than females (95% of male body hair is this type). b. Vellus hairs are soft, fine, short and pale – they cover 65% of the female body and are located in the so called “hairless regions” of males. c. Lanugo hair is fine hair that is slightly thicker than vellus hair – it is present on the fetus and can also replace vellus hair in anorexics. List the parts and describe the growth cycle of hair. © 2008 Mark Tuttle a. Hair does not grow continuously and has 3 phases, making hair growth more complex than epidermal growth. It is cyclic in that hair is lost and replaced periodically. b. Growth Phase (Anagen): This involves the proliferation of the matrix; during this phase, the hair grows in length at a rate of about 0.4 – 0.5 mm per day. The growth phase is not the same length of time for all hair of the body – it is longest in the terminal scalp hair. c. Transitional Phase (Catagen): This short phase involves the stoppage of hair growth; the hair remains in the follicle for this stage. d. Resting Phase (Telogen): This short phase involves the hair shaft falling out of the follicle. e. Note that all individual hairs are in different phases of this cycle so that normally there is always some hair falling out. 15. List the parts and describe the process by which a hair shaft increases in length. a. The matrix of the follicle is where proliferation of the keratinocytes occurs, and cells are pushed superficially from this layer. b. As the cells make there way toward the surface, they pass through the keratogenous zone, where they become fully keratinized (with hard keratin). c. Melanocytes are also included in the medulla (center) of the hair, imparting pigment to the hair shaft. 16. Integrate the morphology of hair and its function. a. Hair is a hard, keratinous epithelial fiber. It is made up of a hair shaft, root and bulb which insert into the follicle of the skin. Hair is used to keep us warm and to keep things out of places where they shouldn’t go (such as keeping dust out of our eyes and nose). 17. List and describe the morphology, function and secretion of the 3 types of glands (sebaceous, sudoriferous (sweat), ceruminous). a. Sebaceous glands are attached to the follicles of hair. They can be simple or branched alveolar, and secrete using the holocrine method (the entire cell is filled with lipid substance, degenerates and becomes the secretion product). The sebum is them emptied into the upper hair follicle by a single duct. These glands can become infected by bacteria and lead to acne. b. There are two types of sudoriferous glands: i. Eccrine are the more numerous and secrete a serous secretion using the merocrine method. They are simple coiled tubular glands which are important for temperature excretion of ions, water, ammonia and urea. These glands can secrete up to 10 liters of sweat per day. Eccrine sweat glands contain clear cells (which secrete serous fluid), dark cells (which secrete mucous material) and myoepithelial cells (which have contractile ability and help expel the secretions from the gland). ii. Apocrine sweat glands are less numerous and open into the hair follicles above sebaceous glands on some terminal hairs. They are also simple coiled tubular glands, but are larger than eccrine sweat glands. They also secrete a serous secretion using the merocrine method (MISNOMER – NOT APOCRINE METHOD!). They don’t start functioning until puberty and bacteria that act on these glands and there secretions can lead to the characteristic odors of the armpit and other regions where these glands are present. © 2008 Mark Tuttle c. Ceruminous glands are modified apocrine sweat glands that secrete wax (cerumen) into the external auditory canal. 18. List the distribution of the different types of glands across the body. a. Sebaceous glands are located in areas where terminal hairs exist. b. Eccrine sweat glands are located all over the body (3-4 million in total). c. Apocrine sweat glands are located in the axilla, perineum (circumanal region) and pubic region. d. Ceruminous glands are located in the external auditory canal. 19. List and describe the morphology and function of the parts of nails. a. See pages 49-50. 20. List and describe the morphology, function and location of the sensory receptors of the skin (free epidermal nerve endings, Merkel endings, Pacinian corpuscles and Meissner’s corpuscles). a. See pages 51-52. 21. Define the describe the following terms: Stratum germinativum Another term for stratum basale. Stratum granulosum The middle layer of the epidermis, composed of granules, moderately keratinized. Keratinocytes The primary cells of the epidermis, these cells are the ones that become the squames and are sloughed off and constantly replenished. Langerhans cells These are immune cells of the epidermis which are usually in the stratum spinosum and are antigen-presenting cells. Keratinizing type Keratin type a cell produces – skin is soft, nails and hair hard. Intercellular bridges These are the “spines” in the stratum spinosum, and are actually just visible desmosomes processes between cells in this layer. Thick skin Also called glabrous skin, this skin has thicker epidermis (more than 1 mm thick) and is thickest on palms and soles. This skin lacks hair and sebaceous glands. Squames These are another name for the flattened squamous cells in the stratum corneum. Corneum Literally means leather – in Latin it refers to the dermis. Epidermal ridges These are raised lines on the skin that indicate the location of primary dermal ridges under the epidermis. Subpapillary plexus This is the most superficial plexus of capillaries in the skin, with loops that project into the dermal papillae. Root of hair This is the portion of the hair that reaches from the center of the follicle down to the bulb. Arrector pili muscle Muscle that attaches from the dermal papillae nearby to the follicle; during © 2008 Mark Tuttle contraction is stands the hair erect and causes goose bumps by pulling the dermal papillae down. Differentiation zone The zone just above the matrix of the hair follicle. Cuticle of hair This is the outermost layer of the hair shaft and is composed of hard keratin. Sebum This is the oily secretion produced by sebaceous glands. Stratum Basale This is the deepest layer of the epidermis and consists of a single layer of keratinocytes in constant mitotic division to produce more cells as the cells of the stratum corneum are sloughed off. Stratum Lucidum This is the deeper portion of the stratum basale where the cells appear clear and indistinct with no nuclei under light microscopy. They are full of keratin, however. Melanocytes These are cells of the epidermis that lie in the stratum basale and are responsible for converting tyrosine to melanin, which imparts color to the keratinocytes. Papillary layer This is the superficial layer of the dermis and is the portion where undulations of the dermis called dermal papillae exist. The connective tissue of this layer is modified areolar (loose) connective tissue. Prickle cells Name for a cell of the stratum spinosum, indicating its spiny appearance. Keratohyalin granules Basophilic, non-membrane-bound, irregularly shaped inclusions in the stratum granulosum. Thin skin Also called hairy or non-glabrous skin, this skin has hair and sebaceous glands, has a reduced stratum corneum, granulosum and spinosum and has no stratum lucidum. It is located everywhere in the body that does not have thick skin. Clear cells These are the cells in eccrine sweat glands that secrete serous solution. These can also be the name of Melanocytes at the LM level, because they produce a clear area around themselves. Interpapillary pegs These are the projections of epidermis that lie between the dermal ridges. Cutaneous plexus This is the plexus of capillaries that exists at the dermal-subcutaneous junction. Hair follicle Tubular invagination of the epidermis down through the dermis into the hypodermis, surrounded by connective tissue and containing the hair and the root sheaths. Dermal sheath The connective tissue surrounding the follicle. Outer (external) root sheath extension of the strata basale and spinosum down into the skin. Cortex of hair The part of the hair that makes up the bulk of the shaft and consists of hard keratin. Sweat Mixture of serous and mucous secretion from sudoriferous glands. © 2008 Mark Tuttle Contusion Another name for a bruise. Eczema Common skin disorder that is characterized by edema, exudation and crusting, along with severe itching (pruritus). The dermis is also affected and immune cells can infiltrate this region more than normal. For this reason, this disease is thought to have an immunological origin. Nail bed Portion of the epidermis over which the nail plate lies – composed of / continuous with the strata basale and granulosum. Eponychium Cuticle of the nail at the root (flap of skin that grows over nail). Stratum Spinosum Layer just superficial to stratum basale, consists of prickle cells that have intercellular bridges visible due to the numerous desmosomes. Stratum Corneum Most superficial layer, consisting of highly keratinized squames which are sloughed off and replaced from the bottom up. Merkel cells These are cells that exist in the stratum basale and are individually innervated to allow for the sensation of light touch. Reticular layer This is the deeper of the two layers of the dermis and is made up of irregular dense connective tissue. Desmosomes Intercellular junctions which bind the cells of the epidermis together and cause the cells to be tightly associated with one another. Keratin Large MW fibrous protein that is present in many of the integumentary cells and structures and imparts hardening and waterproofing of structures. Lamellar granules These are granules that are produced in the stratum spinosum that extrude their contents into the intercellular space to provide hydrophobic waterproofing. Melanosome Vesicles full of melanin on their way into the keratinocytes through the processes of the melanocytes. Dermal papillae Undulations of dermal tissue which stick up into the epidermis. Melanin Brown pigment produced by the skin from the action of tyrosinase. Hair shaft Portion of hair from the center of follicle up to the tip of the hair. Bulb The enlargement at the deep end of the hair follicle, with the dermal papilla (connective tissue) pushing into its deepest margin. Inner root sheath Area of the root that is derived from the outside region of the follicle matrix – it contains soft keratin and disappears half way up the follicle. Medulla of hair The center of the hair shaft, consisting of soft keratin. Solar elastosis Degeneration of the elastic tissue of the skin in sun-exposed patients, particularly older patients. UVA 320 nm, causes increased wrinkling and sagging of skin, increases chance of © 2008 Mark Tuttle skin cancer and does not burn the skin – thus, most tanning salons use this. UVB 370 nm, causes inflammation of the BVs in the dermis and causes sun burning. Most sunscreens block this wavelength, but they should block both. Nail plate (body) The main body of the nail, composed of keratinocytes containing large amounts of hard keratin. It replaces the stratum corneum. Nail matrix The portion of the nail root where keratinocytes proliferate. Nail root The proximal portion of the nail. Decubitus ulcers Also known as bedsores, these are ulcers of the skin that are caused by compromised circulation to an area of skin. Basal cell carcinoma Most common type of all skin cancers, affecting only the keratinocytes in the basal layer of the epidermis. These carcinomas destroy local tissue but do not readily metastasize. Acne Inflammation of sebaceous glands and associated hair follicles due to bacterial infection of them. Lunula The whitened crescent of the nail at the proximal end, where proliferation is occurring. Hyponychium Portion of epidermis growing under the distal end of the nail plate. Psoriasis Chronic skin condition characterized by patches of red-brown area with whitish scales – the cause is complex. The direct cause is proliferation of keratinocytes – they reach the surface far too quickly. The integrity of the epidermis is compromised because lamellar granules are not secreted. Squamous cell carcinoma Second most common skin cancer, this carcinoma affects the squamous keratinocytes and can be caused by a variety of factors such as exposure to UV radiation, X-rays, chemical agents and arsenic. It readily metastasizes. Malignant melanoma Carcinoma of the melanocytes and extremely malignant. Sunburn Burn of the skin caused by excessive exposure to UV radiation, leading to inflammation of the blood vessels in the dermis of the exposed skin. Nevus Benign localized overgrowth of melanocytes arising during early life. Phemphigus Potentially fatal skin disease caused by autoimmune disorder targeting desmosome proteins in epidermis – severe blistering and loss of fluids, as well as easy infection. Melanin-epidermal unit Single melanocyte and its associated keratinocytes. Vitiligo Depigmentation disorder which is genetically inherited defect in skin an hair – characterized by scattered patches of white skin and hair (from destruction of melanocytes). Can be treated cosmetically or using hydroquinone to reduce formation of melanin in normal skin. © 2008 Mark Tuttle Albino Person without tyrosinase but with normal number of melanocytes – has unpigmented skin, hair and eyes. Striae Stretch marks, caused by tearing of the dermis with the epidermis remaining intact. This leads to the gap being repaired with scar tissue and the tear showing through the epidermis as a cosmetic defect. EPU One stem cell in the basal layer and the 10-11 basal cells it produces that migrate to the periphery. Keratogenous zone This is where the cells become fully keratinized in the hair follicle as they move upward. © 2008 Mark Tuttle Integument: Embryology – Crissman 1. List the embryological origin of the epidermis, dermis and skin appendages. a. Epidermis: ectoderm i. Starts as Vernix caseosa: greasy laer ii. Forms Stratum Corneum by week 21 b. Dermis: mesoderm c. Appendages: 2. Relate the types of wound healing and burns to the morphology and function of the skin. 3. Define and describe the periderm and vernix caseosa. Be able to describe their origin, formation and function. a. Periderm i. Secretes amniotic fluid ii. Will become Stratum Corneum b. Vernix caseosa: greasy layer i. Protects fetus from amniotic fluid 4. Describe the origin and usual destination of melanocytes. Describe what occurs if migration and proliferation fail. Be able to describe what determines skin color. a. Neural crest cells migrate from neuroectoderm at 6 weeks to form melanocytes b. Number of melanocytes peaks at end of 3rd month at about 2,300/mm3 5. Describe the process of hemangioma formation. a. A congenital benign tumour or vascular malformation of endothelial cells (the cells that line blood vessels). b. In infancy, it is the most common tumor 6. Describe the formation of the sweat glands, sebaceous glands and mammary glands. Relate the causes of polythelia and polymastia. a. Eccrine Sweat glands i. Start forming at 18-20 weeks ii. Bud elongates down into dermis iii. Solid cord of cell forms coil iv. No more eccrine sweat glands are formed after birth b. Mammary glands i. Develop from apocrine sweat glands c. Polythelia: supernumary nipple d. Polymastia: supernumary breast 7. Describe the formation of the hair folicle and hair shaft. a. Stage I: Invagination of epidermis into dermis (week 12) b. Stage II: elongation of bud into hair bud (week 13) c. Stage III: Hair bulb forms (week 18) 8. Describe the formation of a fingernail/toenail. a. Start at 10 weeks for fingernails b. Toenails lag behind c. Starts on palmar side © 2008 Mark Tuttle d. e. f. g. h. Hypertrichosis Migrates to dorsal side almost immediately Drags innervations with it Forms primary nail field By 14 weeks the nail plate can be seen stil covered by periderm/epidermis Nail plate reaches end of digit by 32 weeks Excessive hairyiness due to the formation of excessive follicles or persistence of hair follicles that normally disappear during development superficial wound healing Only the epidermis is affected deep wound healing Both the epidermis and dermis are affected hirsutism Excessive hairiness with terminal hair in females. Usually a result of androgens abrasion Superficial damage to the skin, usually only to the epidermis erythema Redness of the skin caused by capillary congestion basal cell carcinoma Rarely metastatic acne Blockage in follicle psoriasis Excessive production of keratinocytes lamellar ichthyosis Hyperkeritinization of skin, usually with scale-like appearance pruritus Itch sensation first, second & third degree First: only epidermis is affected burns Second: epidermis and dermis affected Third: No sensation in middle, only painful on periphery. Usually systemic effects are more life-threatening as opposed to local effects squamous cell carcinoma Readily metastatic malignant melanoma sunburn Results from UVB rays nevus Mole phemphigus Autoimmune disease where immune system attacks desmosomes of epidermis. Large blisters. © 2008 Mark Tuttle Embryology 1: Bilaminar Embryo (Ch. 3,7) 1. Describe the formation of the bilaminar embryonic disc from the inner cell mass. a. Amnioblasts separate from the epiblast and form the amnion b. Epiblast froms the floor of the mniotic cavity c. Hypoblast is adjacent to the exocoelomic cavity 2. Describe the formation of the extraembryonic mesoderm. a. Extraembryonic coelomic spaces form and fuse to yield the extryembryonic coelom b. The extraembryonic somatic mesoderm lines the outside of the extraembryonic coelom as well as the amnion c. The extryembryonic splanchnic mesoderm lines the umbilicle vesicle 3. Describe the formation of the primary and secondary yolk sacs. a. The umbilical vesicle shrinks and pinches off the primary umbilical vesicle from the secondary umbilical vesicle as the extraembryonic coelomic space expands to fill the cavity 4. Describe the formation of the body (connecting) stalk. a. As the extraembryonic coelom forms, it seperates from the chorion everywhere except the region nearest to the amnion. b. This region that stays connected becomes the connecting stalk. 5. List three functions of the secondary yolk sac. 1. Role in the transfer of nutrients to the embryo during the second and third weeks when the uteroplacental circulation is being established 2. Blood development first occurs in the well-vascularized extraembryonic mesoderm covering the wall of the umbilical vesicle beginning in the third week and continues to form there until hemopoeitc activity begins in the liver during the sixth week 3. Incorporated as primordial gut in week 4, gives rise to epithelium of trachea, bronchi, lungs, and digestive tract 4. Primordial germ cells develop and eventually migrate to the developing gonads 6. Define and describe: a. Lacuna i. Cavities in syncitiotrophoblast ii. Contain a mixture of maternal blood from ruptured capillaries, cellular deris from eroded uterine glands iii. Fluid in the lacumar space helps nurish the developing embryo b. intervillous space i. space between villi on FETAL side of the equation ii. contains maternal blood, results from coalescence of lacunae iii. separated into invaginations by placental septum, but intervillous spaces are still communicative with each other because septae don’t reach all the way. c. decidua basalis i. layer of deciduas that is most deep to the embryo ii. Forms the maternal part of the placenta iii. eventually (4th month) it disappears entirely giving way to cotyledons © 2008 Mark Tuttle iv. The spiral arterial system supplying the decidua basalis directly beneath the implanting blastocyst, and ultimately the intervillous space surrounding the syncytiotrophoblast of the placenta, is altered remarkably. These spiral arterioles and arteries are invaded by the cytotrophoblasts, and during this process the walls of the vessels in the basalis are destroyed, leaving only a shell without smooth muscle or endothelial cells. As a consequence, these vascular conduits of maternal blood—which become the uteroplacental vessels—are not responsive to vasoactive agents. By contrast, the fetal chorionic vessels, which transport blood between the placenta and the fetus, contain smooth muscle and do respond to vasoactive agents d. decidua capsularis i. most superficial layer of deciduas overlying the conceptus ii. During the early weeks of pregnancy, there is a space between the decidua capsularis and decidua parietalis because the gestational sac does not fill the entire uterine cavity. iii. The blood supply to the decidua capsularis is lost as the embryo-fetus grows and expands into the uterine cavity. iv. expands into unterine cavity as conceptus enlarges v. eventually fuses with deciduas parietalis e. decidua parietalis i. lines the chorionic cavity on the maternal side ii. Eventually the decidual capsularis contacts and fuses with the deciduas parietalis, thereby slowly obliterating the uterine cavity. By 22-24 weeks the reduced blood supply to the deciduas capsularis cuases it to degenerate and disappear. After disappearance of the deciduas capsularis, the smooth part of the chorionic sac fuses with the deciduas parietalis. This fusion can be separated and usually occurs when blood escapose from the intervillues space. The collection of blood (hematoma) pushes the chorionic membrane away from the deciduas parietalis, thereby reestablishing the potential space of the uterine cavity. f. amnion i. Amnion is the top part of the embryonic disc including the amniotic cavity as well as the epiblast g. Chorion i. The syncitiotrophoblast, cytotrophoblast, and extraembryonic somatic mesoderm 7. Describe the formation of the amnion and the chorion. a. Amnioblasts separate from the epiblast and form the amnion b. The chorion consists of two layers: an outer formed by the primitive ectoderm or trophoblast, and an inner formed by the somatic mesoderm; with this latter the amnion is in contact. 8. List the functions of the placenta. © 2008 Mark Tuttle 9. 10. 11. 12. 13. 14. a. Metabolism (synthesis of glycogen) b. Transport of gasses and nutrients c. Endocrine secretion (ex. Human chorionic gonadotropin hCG) Describe the morphological changes that occur during the development of placental villi. a. Cytotrophic invaginations into the syncitiotrophoblast b. Induced by extraembryonic somatic mesoderm Describe the components of the placental membrane or “barrier”. a. Syncitiotrophoblast b. Cytotrophoblast c. Connective tissue of villus d. Endothelium of fetal capillaries Describe the maternal and fetal circulation in the placenta. a. Maternal blood is in inervillous spaces b. Fetal capillaries come up into villi Describe the formation of the amniotic fluid. a. Before keritinization of the skin occurs, a major pathway for passage of water and soutes in tissue fluid form the fetus to the amniotic cavity is through the skin b. Fetus can secrete part of the fluid from the respiratory and gastrointestinal tract c. Also, “urine” is contributed d. Water changes every ~3 hours List several functions of the amniotic fluid. a. Permits symmetric external growth of the embryo and fetus b. Acts as a barrier to infection c. Permits normal fetal lung development d. Prevents adherence of the amnion to the embryo and fetus e. Cushions the embryo and fetus against injuries by distributing impacts the mother receives f. Helps control the embryo’s body temperature by maintaining a relatively constant temperature g. Enables the fetus to move freely, thereby aiding muscular development in the limbs, for example h. Assists in maintaining homeostasis of fluid and electrolytes Define amniocentesis and list several indications for the procedure. a. Performed between 15-18 weeks i. There is relatively little amniotic fluid before the 14th week b. 22 gauge needle through mother’s anterior abdominal nad uterine walls c. Since amniotic fluid is ~150-200ml at this time, ~20ml can be safely withdrawn d. Can tell genetic disorders from this test © 2008 Mark Tuttle Embryology 2: Trilaminar Embryo (Ch. 4-5) 1. Define and describe: a. Hypoblast i. forms the roof of the exocoelomic cavity and is continuous with the thin exocoelomic membrane b. Epiblast i. thicker layer, consisting of high columnar cells related to the amniotic cavity c. primitive streak i. Forms during 3rd week ii. First sign of gastrulation iii. Thickened linear band of epiblast iv. Appears caudally in the median plane of the dorasal aspect of the embryonic disc d. primitive node i. cranial component of primitive streak (separate) e. notochordal process i. Process extending from primitive node onward, but is deep to the ectoderm, whereas the primitive streak had a fold ii. Soon forms a lumen, becomes notocordal canal f. prochordal plate i. Where the notocordal process will connect ii. No mesoderm here iii. Ectoderm and endoderm are in direct contact g. cloacal plate i. future site of the anus ii. caudal to the primitive streak iii. embryonic disc is still bilaminar here 1. only ectoderm and endoderm h. notochord i. notochordal canal fuses with the enderlying endoderm ii. fused layers degenerate, form openings in the floor of the notochordal process iii. brings notochordal canal into communication with the umbilical vesicle iv. notochordal plate develops v. folds over on itself to form the notochord vi. directs cell differentiation around it i. ectoderm j. mesoderm k. endoderm. 2. Describe the formation of the bilaminar embryonic disc from the inner cell mass. a. Amnioblasts separate from epiblast and form the amnion, which encloses the amniotic cavity 3. Describe the formation of the notochord. © 2008 Mark Tuttle a. notochordal canal fuses with the enderlying endoderm b. fused layers degenerate, form openings in the floor of the notochordal process c. brings notochordal canal into communication with the umbilical vesicle d. notochordal plate develops e. folds over on itself to form the notochord f. directs cell differentiation around it 4. Describe the formation of the intraembryonic mesoderm. a. Primitive streak forms primitive pit b. Cells from epiblast flow down in between epiblast and hypoblast c. Become mesoderm 5. List the derivatives of each of the three basic germ layers. a. Ectoderm i. CNS ii. PNS iii. Sensory epithelia of eye, ear, nose iv. Epidermis and its appendages v. Mammary glands vi. Pituitary gland vii. Subcutaneous glands viii. Enamel of teeth ix. Neural crest cells 1. Give rise to cells of spinal, cranial and autonomic systems 2. Ensheathing cells of peripheral nervous system 3. Pigment cells of dermis 4. Muscle, CT, bone of pharyngeal arch 5. Meninges b. Mesoderm i. Connective tissue ii. Cartilage iii. Bone iv. Striated and smooth muscles v. Heart, blood, lymphatic vessels vi. Kidneys vii. Ovaries viii. Testes ix. Genital ducts x. Serous membranes xi. Lining of body cavities (pericardial, pleural, peritoneal) xii. Spleen xiii. Cortex of suprarenal glands c. Endoderm i. Epithelial lining of GI and respiratory © 2008 Mark Tuttle 6. 7. 8. 9. ii. Parenchyma of tonsils, thyroid and parathyroid iii. Thymus iv. Liver v. Pancreas vi. Epithelial lining of urinary bladder and most of urethra vii. Epithelial lining of tympanic cavity viii. Tympanic antrum ix. Pharyngotympanic tube Describe a somite and its derivatives. a. The somite develops from the paraxial mesoderm toward the end of the third week b. Located on each side of neural tube c. 38 pairs of somites develop between days 20-30 d. Good way to tell age of an embryo e. Cranial somites are the oldest, caudal the youngest f. Forms: i. dermis (dermatome) ii. skeletal muscle (myotome) iii. vertebrae (sclerotome) Briefly describe the intraembryonic coelom and its formation. a. A horseshoe shaped cavity appears in the lateral mesoderm b. Somatic mesoderm and overlying embryonic ectoderm form the embryonic body wall or somatopleure c. The splanchic mesoderm and underlying embryonic endoderm form the embryonic gut or splanchnopleure. d. During the second month, divides into: i. Perichardial cavity ii. Pleural cavity iii. Peritoneal cavities. Briefly describe the folding processes that occur in the embryo and the consequences of these processes. a. See next lecture Briefly describe the changes in appearance of the embryo and fetus during development. a. The fourth to eight weeks of development constitute most of the embryonic periods. The critical developmental events occur during the first 3 weeks such as the cleavage of the zygote, blastogenesis, and early development of the nervous and cardiovascular systems. b. All major external and internal structures are established during the forth to eight weeks. c. By the end of this organogenetic period, the main organ systems have begun to develop. As the tissues and organs form, the shape of the emrbyo changes to a more cylindrical appearance, and by the eighth week, it has a distinctly human appearance. © 2008 Mark Tuttle Embryology 3: Folding of the embryo (Ch. 5,9/20) 1. Describe the results of the lateral and longitudinal folding processes that occur in the embryo. a. The growth rate at the sides of the embryonic disk fails to keep pace with the rapid growth of the long axis as the embryo increases rapidly in length. This results in the folding at the cranial and caudal ends of the embryo and relative constriction at the junction of the embryo and the yolk sac. b. By the beginning of the fourth week, the neural folds in the cranial region have thickened to form the primordium of the brain. Initially, the brain projects dorsally into the amniotic cavity. Later, the developing forebrain grows cranially beyond the oropharyngeal membrane and overhangs the developing heart. Concomitantly, the septum transfersum, primordial heart, pericardial coelom, and oropharyngeal membrane move to the ventral surface of the embryo. Part of the yolk sac is incorporated into the embyro as the foregut. c. After folding, the septum transfersum lies caudal to the heart where it subsequently develps into the central tendon of the diaphram. d. Folding of the caudal end results in the partial incorporation of the endodermal germ layer into the embryo as the hindgut. The terminal part of the hindgut dilates and form the coaca. Before folding, the primative streak lies cranial to the coacal membrane; after foldling, it lies caudal. The connecting stalk becomes attached to the ventral surface and the allantois is partially incorporated into the embryo. 2. Define: a. Coelom i. The coelom develops in the lateral intraembryonic mesoderm and makes its way around in a horseshoe shape ii. It will eventually develop into the body cavities (pericardial, pleural, peritoneal) b. Mesentery i. A double layer of peritoneum that begins as an extension of the visceral peritoneum covering an organ ii. Connects the organ to the body wall and conveys vessels and nerves to it c. septum transversum i. Thick mass of cranial mesenchyme that gives rise to parts of the thoracic diaphragm and the ventral mesentery of the foregut in the developed human being. ii. Is the primordium of the central tendon of the diaphragm iii. After the head folds ventrally during the fourth week, the septum transversum forms a thick incomplete partition nbetween the pericardial and abdominal cavities 3. Describe/define the adult structures derived from the primitive intraembryonic coelom. a. Pericardium, pleura, peritoneal cavities b. These are isolated spaces formed in the lateral mesoderm, as the spaces grow, it puches into the intermediate mesoderm. All the cells lining the primative intraembryonic coelom are intraembryonic mesoderm cells. © 2008 Mark Tuttle 4. Describe/define the origin of the cells lining the intraembryonic coelom and its definitive derivatives. a. Once the fully developed, the coelom is lined by the intraembryonic splanchnic mesoderm cranially and intraembryonic splanchnic mesoderm caudally. 5. Describe the configuration of the intraembryonic coelom following the development of the head fold. a. Before folding, the intraembryonic coelom consists of a flattened horseshoe-shaped cavity b. After folding, the pericardial coelom lies central to the heart and cranial to the septum transversum 6. Describe/define the pleuropericardial membranes; the pleuroperitoneal membranes. a. Seperation happens in 7th week b. Pleuropericardial membrane i. Seperates the pericardial cavity from the pleural cavity ii. Contains the common cardinal veins which drain the venous system into the sinus venosus of the heart iii. As the pleural cavity expands ventrally around the heart, splits mesenchyme into: 1. Outer layer that becomes the thoracic wall 2. Inner layer that becomes the fibrous pericardium c. Pleuroperitoneal membrane i. Seperates the pleural cavity from the peritoneal cavity ii. Pleuroperitoneal opening on the right side closes slightly before the left one 7. Describe the relative position of the (thoracoabdominal) diaphragm during its early development a. During the 4th week, the septum transversum lies just opposite to the third to fifth cervical somites b. A large part of the liver is embedded c. Fuse with dorsal mesentery of the esophagus (mesoesophagus) d. By the 6th week, diaphragm has descended to the level of the thoracic somites e. By the beginning of the 8th week, the dorsal part of the diaphragm lies at the level of the first lumbar vertebra 8. List the four major tissue sources contributing to the definitive diaphragm. Correlate each with the related area of the definitive diaphragm. a. Septum transversum i. Tendon of diaphragm b. Mesentary of esophagus i. the opening in the diaphragm through which the esophagus and vagus nerves pass c. Pleuroperitoneal folds and membranes d. Muscular ingrowth (myoblasts) © 2008 Mark Tuttle i. Muscles of diaphragm 9. Describe the probable developmental errors that produce: a. congenital posterolateral diaphragmatic hernia i. 1/2200 ii. Herniation of abdominal contents into the thoracic cavity iii. Life-threatening breathing difficulties iv. The predominance of left-sided defects may be related to the earlier closure of the right pleuroperitoneal opening. b. congenital hiatal hernia i. herniation of part of the fetal stomach through an excessively large esophageal hiatus ii. the opening in the diaphragm through which the esophagus and vagus nerves pass iii. more often this is an acquired condition c. congenital retrosternal hernia i. Herniatiosn through the sternocostal hiatus 1. The opening for the superior epigastric vessels in the retrosternal area ii. Uncommon iii. Herniation of intestine into pericardial sac or part of heart descend s into peritoneal cavity © 2008 Mark Tuttle Embryology 4: Cellular Controls in Development (chapter 8) 1. Briefly explain why the conceptus is not immunologically rejected by the mother during and following the process of implantation. a. Does not display many antigens (HLA component) b. Desidual change makes maternal leukocytes down-regulated 2. Define/describe: homeotic genes (homeobox genes). What is their role in development? How are they regulated? a. Group of genes found in all vertebrates b. Highly conserved c. Involved in early embryonic develo9pment and specify identity and spatial arrangements of body segments d. DNA binding brotein 3. Define the term: critical (sensitive) period of development. List several examples of critical periods and the results of alterations in the regional micro environment within the embryo/fetus during them. a. Critical period: during this time development may be disrupted i. When cell division, differentiation and morphogenesis are at their peak ii. Each organ, tissue, and system has a critical period iii. In general, the first two weeks after fertilization will either cause spontaneous abortion or it will leave the fetus unaffected. b. Examples i. Brain: 3-16 weeks 1. But development continues until 2 years at least ii. Radiation: CNS problems iii. Rubella virus: eye defects iv. Thalidomide: limb defects 4. Describe the principle of cranio-caudal and proximo-distal growth sequences. a. The cranio-caudal and proximo-distal growth sequences occur during the fetal period of development, after the eighth week. Structures develop in a cranial to caudal direction, with the head structures being more developed at any given time than the tail structures. Structures also develop proximally to distal. b. A good example of this is seen in the limbs, where the proximal attachments and regions of the limbs develop earlier than the distal regions. In addition, the upper limb is more developed at any given time than the lower limb, showing a good example of the cranio-caudal growth sequence. The reason that the cranial region develops earlier than the caudal region is that the proliferating tissue during embryonic folding was in the midline. This tissue is related to nervous system development and structures related to the nervous system 5. Define induction. Give two examples of induction during embryonic development. a. Eye i. Optic vesicle induces the development o the lens from the surface ectoderm b. Kidney © 2008 Mark Tuttle i. Metanephric diverticulum induces the formation of the tubules in the metanephric mesoderm 6. Describe the following processes that are important in development: a. tissue aggregation b. cell death i. apoptosis is especially important in development because as the conceptus grows and changes shape, certain parts need to disappear. ii. For example, the tissue between the fingers needs to apoptosize c. Differentiation i. Differentiation is the process of changing from a generic stem cell to a committed specialized cell, like a liver cell d. growth and regeneration 7. Define teratology a. Monster b. Birth defects 8. Give an example of a defect caused by each of the following classes of teratogen. a. Environmental i. Fetal alcohol syndrome ii. Cigarette smoking b. Infectious agents i. Rubella Virus 1. If the rubella virus crosses the placental membrane and infects the fetus, will get congenital rubella syndrome 2. Cardiac defects, cataracts, deafness 3. Sometimes mental deficiency, chorioretinitis, glaucoma, microphthalmia 4. Critical period: 4-5 weeks c. Radiation or chemical i. Can result in cell death, chromosome injury, retardation of mental/physical growth ii. Severity is related to the absorbed dose, dose rate, and stage of embryonic or fetal development iii. 8-16 weeks is the most sensitive period d. Hormonal i. Androgens and progestogens 1. Progesterone produced by corpus luteum 2. Can have a masculinizing effect on female fetus 3. Also cardiovascular problems e. Chromosomal or genetic i. Fetal hydantoin syndrome 1. Genotype determines how the fetus responds to phenytoin 2. With a certain genotype, this drug is teratogenic © 2008 Mark Tuttle 3. With other genotypes, it is harmless f. Autosomal abnormalities i. Down’s syndrome g. Sex chromosome abnormalities i. Klinefelter’s XXY ii. Turner’s X0 h. Mechanical i. Oligohydramnios: reduced quantity of amniotic fluid 1. Mechanically induced deformation of limbs 2. Limb gets “pinched off” ii. Amniotic bands: rings formed as a result of rupture of amnion during early pregnancy © 2008 Mark Tuttle Development of the muscular system (chapter 15) - Chiaia 1. Define and describe the location of three types of muscle tissue: a. Skeletal i. Paraxial mesoderm Somite Myotome Skeletal muscle b. Cardiac i. Lateral mesoderm Splanchnic mesoderm Cardiac muscle c. Smooth i. Lateral mesoderm Splanchnic mesoderm Smooth muscle 2. List and describe the differences between the developmental origins for the skeletal muscle of the body: a. trunk muscles i. Develop from myoblasts that remain in the myotome b. pharyngeal arch muscles i. From the first 7 “somites” that didn’t fully develop ii. Myoblast here forms 1. Muscles of mastication (chewing) 2. Facial expression 3. Pharynx, larynx c. ocular muscles i. iris muscle comes from ectoderm d. tongue muscles i. From the hypaxial mesoderm e. muscles of the limbs i. From the hypaxial region of myotomes in specific somatic levels (where the limbs should be) ii. Differentiate and migrate iii. Dorsal limb bud 1. All extensor muscles/supinators 2. Innervated by dorsal branch of ventral rami iv. Ventral limb bud 1. All limb flexors 2. Upper limb protanators 3. Innervated by ventral branch of ventral rami 3. Define and/or describe: a. epaxial musculature i. dorsomedial ii. Extensor muscles of the neck and vertebral column iii. Innervated by the dorsal primary ramus of the spinal nerves iv. Stimulated to form by Myt5 b. hypaxial musculature i. ventrolateral ii. form muscles of body wall, lumbs, tongue iii. stimulated to form by MyoD 4. Describe the process of muscle cell maturation a. Fusion of mononucleated myoblasts to form multinucleated myotubules b. Expression of contractile proteins and arrangement of sarcomeres i. Functional fiber type is established during this phase © 2008 Mark Tuttle ii. Connective tissue sheath of myotubule appears to play an instructive role in the expression of proteins appropriate for different fiber types c. Founder cells recruit fusion-competent cells 5. List the major regulatory factors that influences muscle cell maturation a. MyoD: Hypaxial muscles i. BMP4 initiates this b. Myt5: Epaxial muscles i. Wnt initiates this c. Ephrin: Somite segmentation © 2008 Mark Tuttle Development of the Skeletal System: Limbs and Back – Hankin (Chapter 15) 1. Understand how mesoderm and neural crest contribute to skeletal system formation. a. Mesoderm differentiates into muscles b. Neural crest cells differentiate into melanocytes of epidermis 2. Understand the basic processes involved in development of the axial skeleton. a. Understand the principal molecules and genes involved in somite differentiation that relate to skeleton development. i. Noggin and sonic hedgehog (shh) secreted by notochord and neural tube floor ii. Induce sclerotome formation iii. Sclerotome expresses PAX1 b. Vertebrae and ribs i. Describe how vertebrae and ribs are formed by endochondral ossification of sclerotome regions of somites. 1. Sclerotome on each side of body contributes to each vertebra and intervertebral disc 2. Ribs form from lateral outgrowths of thoracic vertebrae ii. Describe the formation of intervertebral disks 1. Cranial and caudal parts of adjacent somites combine to form vertebra 2. Ventral part forms centrum around notochord (future vertebral body) 3. Dorsal part of each vertebra forms costal processes (future transverse processes) and vertebral arch 4. Notochord persists and enlarges to form nucleus pulposus iii. Understand the principal molecules and genes involved in development of vertebral column 1. SHH stimulates sclerotome cells to express PAX1 2. Guides ventromedial sclerotome cells to form centrum 3. Induction of roof plate of neural tube results in PAX9, MSX1, and MSX2 expression a. Guide lateral sclerotome cells to form dorsal (vertebral) arch 4. Individual vertebrae specified by combinations of Hox genes a. Atlas (C1): Hoxa-1, Hoxa-3, Hoxb-1, Hoxd-4 b. Axis (C2): Hoxa-1, Hoxa-3, Hoxb-1, Hox-4, Hoxa-4, Hoxb-4 iv. What are brevicollis, spina bifida, and scoliosis; what are some of the causes for these defects? 1. Breviocollis a. Rare congenital failure of segmentation of cervical vertebrae b. Usually C2&C3 c. Short neck d. 60% associated with scoliosis e. 36% associated with hearing loss f. 34% associated with GI abnormalities 2. Spina bifida a. Incomplete development of vertebral arch i. Primary: failure of normal vertebral induction ii. Secondary: failure of neural tube to close dorsally b. Herniation of spinal cord and/or meninges 3. Scoliosis © 2008 Mark Tuttle a. Defective formation of ONE SIDE of vertebral column i. Can be “cumulative” b. Hemivertebra: only half a vertebra forms 4. Causes a. Hox gene misexpression b. Excess retinoid acid (RA) (vitamin a) i. Cranio-caudal RA gradient is disrupted c. Metabolic disturbances (ex. Maternal diabetes) v. Describe how ribs form from lateral processes of thoracic vertebrae 1. Sclerotome cells migrate within somatic lateral plate mesoderm around body curvature toward ventral surface vi. Describe how the sternum and clavicle are formed 1. Sternum is fusion of first 7 vertebrae 2. Clavicle forms in weeks 5-6 a. Ossification doesn’t complete until 21 years old! b. Forms by intramembranous ossification vii. What is cleidocranial dysplasia? 1. Affects head, dentition, and clavicle 2. Can be without a clavicle alltogether 3. 1/1,000,000 4. Nose flat, wide, lacking bridge 5. Presence of supernumerary and unerupted teeth 6. Primary dentention may be retained into adulthood 3. Understand the basic processes involved in development of the appendicular skeleton. a. Describe how somatic lateral plate mesoderm forms the skeleton of the appendages – the limb bones and appendicular girdles. i. Forms from lateral plate mesoderm as opposed to somitic mesoderm like axial skeleton ii. Limb buds form consisting of mesenchyme b. Describe how the appendicular skeleton is formed by endochondral ossification of cartilage models. i. Cartilage forms first, then ossifies ii. Clavicle forms by intramembranous ossification c. Understand the role of the apical ectodermal ridge (AER), zone of polarizing activity (ZPA), and the molecules that establish axes of polarity in the limb. i. Apical Ectodermal Ridge (AER) 1. Is a thickened distal border of limb bud 2. Bone Morphogenetic Proteins (BMPs) induce AER formation 3. Exerts influence on underlying mesenchyme 4. Prevents differentiation, promotes rapid proliferation 5. As limb grows, proximal portion becomes farther away from influence of AER, begins to differentiate ii. Zone of Polarizing Activity (ZPA) 1. Cluster of cells at caudal border of limb 2. Location determined by HOX + Gli 3. Produce retinoic acid (RA) which initiates expression of sonic hedgehog (shh) a. Absence of shh yields the degeneration of AER © 2008 Mark Tuttle 4. Yields location of digits d. Describe how digits (fingers and toes) are formed. What is the role of cell death? i. At 48 days gestation, apoptosis occurs in AER to create ridge for each digit ii. At 51 days, cell death in interdigital space iii. 56 days: separation complete iv. Bone Morphogenetic protein concentration determines digit identity 1. Highest near digit 4 2. Lowest near digit 1 (thumb/big toe) e. Describe limb rotation and the consequences for muscle compartments i. Arm rotation occurs laterally during development ii. Leg rotation occurs medially during development iii. Consequence: flexors and extensors are on opposite sides for arms and legs in mature human f. What are amelia, meromelia, and achondroplasia? i. Amelia 1. Complete absence of limbs ii. Meromelia 1. Partial absence f limb 2. Phocomelia (proximal long bones are absent or small) iii. Achondroplasia 1. Abnormal ossification of cartilage 2. Epiphyseal growth retarded and ceases early 3. Dwarfism g. What are the epiphyses and diaphyses and what are their significances? i. Epiphysis is the head of a long bone ii. Diaphysis is the shaft of a long bone iii. Diaphysis ossifies first and proceeds towards epiphyses 4. Describe how synovial joints are formed? a. Formed in cartilaginous condensations when chondrogenesis is arrested b. Joint “interzone” induced c. Joint cavity formed by cell death d. WNT14 is inductive signal © 2008 Mark Tuttle Blood –Howard 1. Identify the components of the blood and describe their functions. a. Transport O2 and CO2 b. Body buffer c. Transport hormones, molecules d. Produce and transport antibodies e. White blood cells i. 60-70% Neutrophils ii. 20-25% Lymphocytes iii. 3-8% Monocytes iv. 2-4% Eosinophils v. 0.5-1% Basophils 2. Identify sites of hematopoesis and describe what happens there. a. Prenatally it happens in spleen, liver, yolk sac b. Postnatally it happens in bone marrow i. Most persistent in vertebrae/sternum ii. Nonfunctional cells can react to replace functional cells if functional cells are destroyed iii. Hemopoetic cord 3. Explain the importance of stem cells and how they relate to hematopoiesis. a. Stem cells are self-renewing and produce blood cell progenitor cells 4. Describe the functional anatomy of the bone marrow. a. Sinusoids are near megakaryocytes so that they can secrete platelets out 5. Distinguish the developmental stages of formed elements a. Granulopoeisis i. Promyelocyte 1. Oval nucleous with nucleoli 2. Basophilic cytoplasm 3. Azurophilic granules ii. Neutrophilic myelocyte, eosinophilic meyolocyte, basophilic myelocyte (committed differentiation) 1. Specific granules 2. Nucleus changes shape b. Monopoeisis i. Monoblast ii. Promonocyte 1. Well developed golgi, abundant RER, mitochondria, lysosomes iii. Monocyte 1. Differentiate into macrophages c. Lymphopoiesis i. Lymphoblast ii. Prolymphocyte 1. T-cell progenitor 2. Β-cell progenitor 6. Describe the functions of the granulocytes. © 2008 Mark Tuttle Thoracic Wall, Lungs, Pleura -Lane Describe the boundaries and reference lines of the thoracic cavity and the skeletal components (thoracic cage) of the thoracic wall. a. Thoracic cavity i. Superior portion of trunk ii. Upper half of body iii. Diaphragm separates thorax from abdominal cavity b. Skeletal components i. Ribs 1-12 1. True ribs: 1-7 2. False ribs: 8-10 3. Floating ribs: 11-12 ii. Vertebra T1-T12 iii. Sternum 1. Manubrium 2. Body 3. Xyphoid process c. Reference lines i. Midclavicular line 1. Middle of the clavical running longitudally downward, almost through nipple ii. Costal margin 1. Bottom edge of ribs What are the functions and surface landmarks associated with the thoracic cage? a. Superior thoracic aperture (Thoracic inlet) i. T1 vertebra ii. 1st rib iii. Manubrium b. Inferior thoracic aperture (Thoracic outlet) i. T12 vertebra ii. 11th/12th ribs iii. Costal margin iv. Xyphosternal junction c. Sternal angle i. T shape junction of sternum and manubrium d. Jugular notch i. Superior notch of medial manubrium Describe the anatomy and articulations of a typical rib. a. Head i. Superior facet: articulates with superior vertebra ii. Inferior facet: articulates with inferior vertebra iii. Crest of head: articulates with intervertebral disc b. Costal tubercle i. Articular part: articulates with transverse process ii. Nonarticular part: point of attachment for skeletal muscle c. Costal groove i. Groove on deep, inferior part of rib that shields intercostals neurovasculature d. Joints: these are all synovial, but there is not much movement here © 2008 Mark Tuttle i. Constovertebral 1. Rib & vertebrae ii. Costotransverse 1. Rib & transverse process iii. Costochondral 1. Rib & costal cartilage iv. Sternocostal 1. Sternum & costal cartilage Describe the process of respiration and the associated movements of the thoracic wall. a. Quiet inspiration i. Diaphragm only increase in vertical dimension b. Active inspiration i. Diaphragm increase in vertical dimension ii. Respiratiory muscles contract increase in transverse and anterior-posterior dimensions 1. Pectoralis major 2. Serratus anterior 3. Serratus posterior superior/inferior 4. Scalene 5. Intercostal 6. Subcostal 7. Transversus thoracis iii. Bucket handle iv. Pump handle Describe the anatomy of the breast. What is the clinical significance of the lymphatic drainage in this region? a. Nipple i. Openings of lactiferous ducts b. Areola i. Pigmented skin surrounding nipple c. Subcutaneous tissue i. Mammary glands ii. Lactiferous ducts iii. Lactiferous sinuses iv. Suspensory ligaments (of Copper) v. Retromammary space 1. Breast not connected to chest wall d. Neurovasculature i. Arteries 1. Tributaries of internal thoracic a. 2. Pectoral branch of thoracoacromial a. 3. Lateral thoracic a. 4. Posterior intercostals a. ii. Nerves 1. 4th-6th intercostal nn. e. Lymph nodes i. Important as a vehicle for metastatic breast cancer ii. 90 % into the axillary lymph node © 2008 Mark Tuttle Describe the muscles that make up the thoracic wall. a. Intercostals i. External 1. Oriented in V shape 2. Elevates the ribs during active inspiration ii. Internal 1. Oriented in upside-down V-shape 2. Interosseous part depresses ribs 3. Interchondral elevates ribs Neurovascular bundle is here iii. Innermost 1. Oriented in upside-down V-shape 2. Interosseas part depresses ribs 3. Interchondral part elevated ribs What nerves, arteries and veins supply the thoracic wall? a. Neurovascular bundle i. V – Vein 1. Drains into azygous system, internal thoracic vein ii. A – Arteries 1. Posterior intercostal a. supplied by thoracic aorta 2. Anterior intercostals a. supplied by internal thoracic a. iii. N – Nerves 1. Ventral rami of T1-T12. T12 is called subcostal n. Describe the arrangement of the intercostal nerve, artery and vein within the intercostals space. a. VAN b. In costal groove Describe the major anatomical compartments within the thoracic cavity: pleural cavities and the mediastinum. a. Parietal pleura i. Intimate with chest wall ii. Most superficial pleura iii. Parts 1. Costal: Communicates with ribs 2. Diaphragmatic: Inferior aspect 3. Mediastinal: Medial aspect 4. Cervical: Superior aspect (above 1st rib – cupola) b. Visceral pleura i. Intimate with lungs c. Pleural cavity i. Between visceral/parietal pleuras ii. Parts 1. Costodiaphragmatic recess: Inferior portion of the pleural cavity 2. Costomediastinal recess: Medial portion of the pleural cavity d. Other landmarks i. Hilum of lung: Where parietal/visceral pleuras meet ii. Root of lung: Where mediastinum/lung meet iii. Pulmonary ligament: Continuation of Hilum inferior to root © 2008 Mark Tuttle Lungs and Pleura - Lane What distinguishes parietal from visceral pleura? a. Parietal pleura is not intimate with the lung b. Visceral pleura is Describe the 4 regions of parietal pleura. a. See above What is the pleural cavity. How does it relate to the thoracic cavity. What are the costodiaphragmatic and costomediastinal recesses of the pleural cavity? a. See above Describe pathologies associated with the pleural cavity including: a. Pneumothorax i. b. Hemothorax i. c. Chylothorax i. d. Pleuritis (pleurisy) i. Describe the surfaces, lobes, and fissures of the right and left lung. a. Right lung i. Three lobes 1. Middle a. Really only on anterior side b. Posterior side two fissures meet 2. Superior 3. Inferior ii. Two fissures 1. Oblique a. Superior portion is at about the level of the 6th rib 2. Horizontal a. Superior portion is at about the level of the 4th rib b. Left lung i. Two lobes 1. Superior 2. Inferior ii. One fissure 1. Oblique a. Superior portion is about the level of the 4th rib Describe the anatomy associated with the root or hilum of the lung. a. Triangular depression b. Contents i. Pulmonary artery, superiormost on the left lung ii. Superior and inferior pulmonary veins iii. Bronchus, with bronchial vessels surrounding it Describe the anatomy of the trachea and bronchi. Why are aspirated foreign objects often found in the right lung? a. Trachea © 2008 Mark Tuttle i. Starts at C6 ii. 16-20 cartilaginous rings 1. Except in posterior where it articulates on esophagus (Wood block food) b. Brochii i. The right bronchus is oriented more straight up and down and is larger ii. The left bronchus most deviate at a sharper angle to get around the pericardial sac iii. Lobes 1. 2 lobes on left = 2 secondary bronchii 2. 3 lobes on right = 3 secondary bronchii iv. Each lobe branches into segmental (tertiary) bronchii Be able to explain the concept of bronchopulmonary segments a. A bronchopulmonary segment is a given region of the lung supplied by one artery and one tertiary bronchus b. Bulmonary veins tend to NOT travel with the arteries, but instead between segments c. About 10 per lung d. Diseases can affect one segment without affecting the others, even if it is removed Describe the blood circulatory systems (Pulmonary and Bronchial) associated with the lungs a. Bronchial: supply oxygenated blood to the lungs i. Small ii. Usually 2 to right lung, 1 to left lung b. Pulmonary: supply de-oxygenated blood to perform gas exchange with inspired air i. Large ii. 19 total iii. 3 superior lobe branches in each lung iv. 2 medial in right lung, 1 in left lung v. 6 inferior lobe branches in each lung Describe the autonomic innervation of the lungs. a. Parasympathetic i. Vagus nerve 1. Pulmonary plexus a. Bronchoconstrict, vasodialate, secretory b. Cough reflex b. Sympathetic i. Paravertebral sympathetic ganglia 1. Pulmonary plexus a. Bronchodialate, vasoconstrict, inhibit secretions b. Visceral pain Describe the lymphatic drainage of the lungs. a. Intimately associated b. Superficial (subpleural): on periphery of pleura i. Bronchopulmonary nodes ii. Tracheobroncial nodes iii. Bronchomediastinal trunk iv. Right lymphatic duct (both) or thoracic duct (left only) c. Deep (Peribronchail): Follows bronchial tree i. Pulmonary nodes ii. Bronchopulmonary nodes © 2008 Mark Tuttle iii. Bronchomediastinal trunk iv. Right lymphatic duct (both) or thoracic duct (left only) Be able to relate the borders, lobes, fissures, and sounds of the lungs as well as the pleural recesses to the surface anatomy of the thorax. a. OK © 2008 Mark Tuttle Histology of the Respiratory System - Giovannucci Identify the anatomical components of the respiratory system. Differentiate between the ventilation system, conducting and respiratory portions of the respiratory system. Be able to describe their components, morphology and functions. Conducting i. Cleans, humidifies, adjusts temperature of air ii. Contains sites of olfaction and phonation iii. Components 1. Nasal cavity 2. Paranasal sinuses 3. Pharynx 4. Larynx 5. Trachea 6. Bronchi 7. Bronchioles Ventilation system Respiratory system i. Sites where gas exchange occurs ii. Components 1. Respiratory bronchioles 2. Alveolar ducts 3. Alveolar sacs Define the tissue layers and cell types found in the nasal cavity, pharynx, larynx, trachea, bronchi, bronchioles and alveolar airways. Relate the structure to the function of each of the above organs. Nasal cavity i. Abundant goblet cells and glands ii. Ciliated pseudostratified columnar epithelium iii. No cartilage iv. No muscles v. No elastic fibers Pharynx i. Same as nasal cavity except elastic fibers are present here Larynx i. Same as pharynx but add cartilage (complex hyaline/elastic) Trachea i. Same as larynx but add C-shaped rings of cartilage, smooth muscle Bronchi i. Same as trachea but glands/goblet cells are fewer, rings are irregular, smooth muscle, elastic fibers are now abundant Bronchioles – alveolar airways i. Transitions to ciliated simple cuboidal epithelium in respiratory bronchioles ii. Goblet cells and glands disappear iii. Cartilage disappears iv. Smooth muscle and elastic fibers are abundant © 2008 Mark Tuttle Know how the epithelium of the larynx is adapted for voice production or altered by cigarette smoke. When infected, or irritated by cigarette smoke, the vocal folds become inflamed and cannot vibrate together effectively i. Smoker’s cough: Cigarette smoke destroys or paralyzes the cilia, so only way to clear phlegm is by coughing False vocal fold (top): stratified non-keritinated squamous True vocal fold (bottom): pseudostratified ciliated coumnar Describe how the histology of the respiratory system is designed to meet functional requirements associated with gas exchange between the body and the atmosphere. Large surface area (140 m2) Very thin (0.1 um) Abundant capillary supply Both air and blood volumes must be rapidly cycled past blood-gas barrier Explain the structure of the alveolar-capillary membrane. Extremely flat 0.2 um thick 4 layers to cross i. Alveolar epithelial wall of type I cells ii. Fused alveolar epithelial/capillary basement membrane iii. Endothelial cell of capillary Be able to describe the location and structure of ciliated cells, mucus producing cells, alveolar macrophages, type I and type II pneumocytes and how they relate to their individual functions in the respiratory system. Ciliated cells i. Located in upper respiratory tract ii. Help move mucus elevator Mucus producing cells i. Goblet cells produce mucinogen (mucin zymogen) (sticky) Alveolar macrophages i. Final scavenger for resp system ii. Monocyte enter lung interstitium iii. Roam across alveolar surface and phagocytize debris iv. Move into a conducting bronchiole and ride mucociliary escalator to orpharanx v. 100 million times per day Identify the respiratory system cell types involved in and their functional relationship with carcinoid disease, asthma, respiratory distress syndrome, heart failure and emphysema. Carcinoid disease i. Tumor in DNES (Diffuse neuroendocrine system) cells AKA APUD (amine precursor uptake and decarboxylation cells) AKA small granule cells ii. 3% iii. Secrete hormones and biogenic amines (i.e. Kulchitsky cell) Asthma i. Bronciole thickening, restricting airway Respiratory distress syndrome i. Alveolar type II cells 1. Don’t produce enough surfactant 2. Common in premature babies © 2008 Mark Tuttle Heart failure i. Alveolar macrophages ii. Heart failure cells are hemosiderin-containing macrophages in the alveoli. The main causes are left heart failure and chronic pulmonary edema. iii. In left heart failure, the left ventricle cannot keep pace with the incoming blood from the pulmonary veins. The resulting backup causes increased pressure on the alveolar capillaries, and red blood cells leak out. Alveolar macrophages ingest the red blood cells, and become engorged with brownish hemosiderin. iv. In pulmonary edema, alveolar septa get thick and fibrous, again increasing pressure on alveolar capillaries and resulting in leakage of red blood cells which undergo phagocytosis by alveolar macrophages. Emphysema i. Alveoli ii. Goblet cell metaplasia and replacement of surfactant-secreting Clara cells with mucus-secreting and infiltrating mononuclear inflammatory cells. iii. Smooth-muscle hypertrophy may also be present. iv. These abnormalities may cause luminal narrowing by excess mucus, edema, and cellular infiltration. v. Reduced surfactant may increase surface tension at the air-tissue interface, predisposing to airway narrowing or collapse. respiratory epithelium Pseudostratified ciliated columnar epithelium (PCCE) olfactory epithelium Pseudostratified ciliated columnar Thicker than respiratory epithelium Lacks goblet cells swell bodies Within the lamina propina of conchae in nasal cavity Every 20–30 min, the swell bodies on one side of the nasal fossae become engorged with blood, resulting in distention of the conchal mucosa and a concomitant decrease in the flow of air. During this time, most of the air is directed through the other nasal fossa. These periodic intervals of occlusion reduce airflow, allowing the respiratory epithelium to recover from desiccation (dryness). Clara cells Non-ciliated columnar epithelium with microvilli Abundant mitochondria and secretory vesicles that contain glycoproteins Can proliferate and replace ciliated cells Secretes stuff that protects the bronchioles from damage Secretes components of the lung surfactant Amine precursor uptake and decarboxylation cells (3%) Secrete hormones and biogenic amines i.e. Kulchitsky cell Tumors in these cells result in Carcinoid Disease Narrow columnar cells with microvillus border Replacement cell or sensory cell (3%) neuroendocrine cells ciliated columnar epithelium brush cells © 2008 Mark Tuttle basal cells Part of olfactory epithelium Replaces both olfactory and sustentacular cells mucous goblet cell Secrete mucinogen sero-mucus glands A mixture of watery and mucinous material small granule cells DNES cells Kulchitsky cells Example of DNES cells, associated with carcinoid disease alveolar macrophage Final scavenger for respiratory system Once it is engorged with stuff it migrates into a conducting bronchiole, rides the mucus elevator to the oropharynx 100 million per day Type I pneumocyte Covers 95% of alveolar surface Very thin Basal lamina often fuse with adjacent capillaries Type II pneumocyte Covers 5% of alveolar surface Produces surfactant More of them than type 1, but type 1 are so flat that they cover more surface area cells surfactant a phospholipid-protein mixture that is secreted onto the surface of the alveoli to reduce surface tension fetal distress syndrome Alveolar type II cells don’t produce enough surfactant Common in premature babies hyaline membrane disease Identical to respiratory distress syndrome trachea primary, secondary & tertiary bronchi Bronchus splits into branches as it enters the lungs conducting bronchioles Part of respiratory system which moves air in and out and moves foreign material up the mucus escalator alveolar ducts Linear airway lined by alveoli Terminate as alveolar sacs alveolar sacs Cul-de-sacs (dead ends) lined with alveoli respiratory bronchioles First site of gas exchange blood-air barrier emphysema squamous metaplasia atrium Junctions which open into alveoli olfactory cells supporting cells lamellar bodies secretory organelles found in type II pneumocytes and in © 2008 Mark Tuttle keratinocytes. In pneumocytes, the choline-based phospholipids that are stored in the lamellar bodies, serve as pulmonary surfactant after being released from the cell pulmonary surfactant dust cells alveolar pores alveoli Alveolar macrophage © 2008 Mark Tuttle Mediastium - Baptista 1. Delineate the superior, anterior, middle, and posterior mediastinum. a. Superior i. Above T5/Sternal angle b. Anterior i. Bordered by sternum/pericardial sac c. Middle i. Anteriorly bordered by the anterior mediastinal compartment ii. Posteriorly borderd by the posterior mediastinum d. Posterior i. Bordered by pericardial sac anteriorly/anterior surface of vertebral bodies posteriorly 2. Describe the major structures associated with the four regions of the mediastinum. a. Superior i. Thymus ii. Aorta branches into brachiocephalic trunk, left common carotid a., left subclavian a. iii. Superior Vena Cava branches into left and right brachiocephalic veins iv. Trachea branches into left and right bronchi v. Esophagus vi. Right/left vagus n. vii. Phrenic nn. viii. Thoracic duct b. Anterior i. Sternopericardial ligament ii. Fat iii. Lymph nodes c. Middle i. Pericardium ii. Heart iii. Phrenic nn iv. Pericardiophrenic vessels v. Stems of great vessels d. Posterior i. Descending aorta ii. Esophagus iii. Azygous system of veins iv. Vagus n v. Thoracic duct vi. Lymph nodes vii. Thoracic splanchnic nn 3. Identify the contents of the superior mediastinum and relationship to the heart and lungs. a. See above 4. Identify the borders of the posterior mediastinum. a. See above 5. List the major vessels that occupy the posterior mediastinum. a. See above 6. Define the origin, course, and termination of the thoracic duct. © 2008 Mark Tuttle 7. 8. 9. 10. a. Lymphatic duct b. Drains all of body below the diaphragm and on the left side of the thorax (everything except right side of thorax) c. Ascends through the aortic hiatus of the diaphragm d. Ascends between azygous vein and aorta to T4-T5 plane e. Terminates in left subclavian v. Describe the path of the esophagus and trachea through the thoracic cavity. a. Trachea i. Originates at larynx ii. Bifurcates at T4-5 iii. Anteriorly: great vessels and thymus iv. Posteriorly: esophagus v. Azygous v to the right of bifurcation vi. Aortic arch to the left of bifurcation vii. Carina divides the bronchi b. Esophagus i. Goes through superior and posterior mediastinum ii. Pierces diaphragm at T10 to join stomach Describe the azygos system of veins. a. Drains intercostals veins, some lumbar segmental veins b. Azygous vein i. Alternate route to superior vena cava ii. Ascends along right side of vertebral column to T4 1. Superficial to intercostals aa. 2. Thoracic duct to the left c. Hemiazygous vein i. Formed by union similar to azygous ii. Ascends left of vertebral column iii. Crosses over to join azygous at T8-9 d. Accessory hemaizygous vein i. Formed by posterior intercostals 4-8 ii. Crosses to join azygous at T8 Describe and contrast the distribution of the vagi and phrenic nerves throughout the thoracic cavity. a. Vagus nerves form a plexus at the heart around the aortic arch Discuss the relationship of the heart, pericardium, lungs, and pleura to structures in the posterior mediastinum. a. Descending aorta, esophagus, vagus nerve, azygous system of veins, thoracic duct b. Left laryngeal nerve runs off of vegus nerve © 2008 Mark Tuttle Development of the Respiratory System - Lane 1. Define: pharynx, larynx, foregut, pharyngeal arches and pouches. a. Pharynx: b. Larynx: airway supported by thyroid cricoids, arytenoids and epiglottic cartilages c. Foregut: pharynx, esophagus, stomach, duodenum d. Pharyngeal arches: Ventral/lateral walls of foregut e. Pharyngeal pouches: packets along inner surface of forgut, lined by endoderm 2. List the germ layers of origin for: epithelium, glands, cartilage, smooth muscle, and blood vessels of the respiratory system a. Cartilage: splanchnic mesoderm b. Smooth muscle: splanchnic mesoderm c. Epithelium: endoderm d. Blood vessels: e. Glands: Endoderm 3. Describe the laryngotracheal groove. a. Gives rise to both lungs b. Between 4th and 6th pharyngeal arches 4. Define/describe the development of the laryngeal cartilages and musculature. a. Starts as one tube b. Respiratory bud forms induced by Fibroblast Growth Factor 10 (FGF10) off of esophagus c. Laryngeal groove forms at ~4 weeks d. Eventually the groove fuses and the two tubes are separated i. This forms the tracheoesophageal septum e. Laryngeal epithelium: Endoderm of laryngotracheal tube f. Epiglottis: Mesenchyme of hypobrachial eminence (3/4 pharyngeal arches) g. Arytenoid, cricoid: Mesenchyme of cranial laryngotracheal tube (4/6 pharyng.arch) h. Thyroid cartilage: “ i. Laryngeal muscles: Myoblasts in 4th/6th pharyngeal arches 5. Describe the process by which the trachea is separated from the esophagus by the tracheoesophageal septum (folds). a. See above 6. Describe the probable process by which a congenital tracheoesophageal fistula is created. a. Called H-type b. 1/3000 c. The trachea probably never fully separates from the esophagus during development 7. What are the consequences of this defect? a. Problems eating and breathing 8. Define/describe the lung buds. a. Primordial division in thelaryngotracheal diverticulum that will eventually become the two primary bronci 9. Correlate the first, second, and third divisions of the distal end of the primitive trachea with the bronchi of the adult lung. 10. Define/describe the four major phases in lung development. a. Pseudoglandular period 6-16 weeks i. Conducting airways develop in lungs ii. Capillaries form in splanchnic mesoderm b. Canalicular period 16-26 weeks i. Lumen of bronchi and bronchioles enlarge © 2008 Mark Tuttle 11. 12. 13. 14. 15. 16. ii. Bronchioles and alveolar ducts increase in number iii. More blood vessels form, stimulated by Wnt iv. Gas exchange is now possible c. Terminal sac period 26 weeks to birth i. Capillaries move into position next to epithelia ii. Epithelium thins (type I pneumocytes) iii. More terminal sacs form iv. Type II pneumocytes emerge v. End of this period: sufficient surfactant d. Alveolar period 32 weeks to 8 years i. 95% of all alveoli develop ii. Mature alveoli develop after birth iii. More bronchioles, alveolar ducts, alveolar sacs Describe the processes by which the intraluminal fluid contents of the respiratory system are removed at and immediately after birth. a. Expelled during delivery b. Absorbed by pulmonary capillaries c. Absorbed by lymphatics Define/describe: surfactant. Where and when is it produced? What is its function? a. Produced by the type II pneumocytes with clara cells secreting components of surfactant b. Surfactant keeps alveoli from collapsing by reducing surface tension What are the consequences of a lack of surfactant in the lung? a. Lung will collapse Define/describe: respiratory distress syndrome (RDS)/ hyaline membrane disease (HMD). How are these pathological processes treated currently? a. Monitor phospholipid levels in amniotic fluid b. Treat mother with steroids before birth c. After birth, treat with synthetic/animal surfactant d. After birth, continuous positive airway pressure (CPAP) Explain the formation of: congenital lung cysts, lung agenesis, and lung hypoplasia. a. Congenital lung cysts i. Blockage of airway ii. Air or fluid filled cysts iii. Usually on visceral surface of lung b. Lung agenesis i. Bronchial bud fails to grow into mesenchyme of lung ii. If it occurs only on one side (unilateral), infant can survive c. Lung hypoplasia i. Often associated congenital diaphragmatic hernia ii. Usually on left side abdominal organs push stuff on right side over iii. Usually fatal Describe the major features of the time line for respiratory system development. How do these features relate to the survivability of a premature infant. a. It is not possible for the infant to survive without respiratory bronchioles which develop by 24 weeks b. It is possible for an infant to survive without sufficient type II cells/surfactant yet developed (~25 weeks) © 2008 Mark Tuttle i. However, they will need synthetic surfactant © 2008 Mark Tuttle Heart and Pericardium – Baptista 1. Describe the location of the heart within the thoracic cavity and its relationship with the pericardium and the pericardial cavity. a. Heart is in the medial mediastinum b. Inside the pericardium and pericardial cavity 2. Describe the structure and function of the layers of the pericardium a. Fibrous layer: Forms bulk of the gross pericardial sac b. Parietal serous: Lines inside of fibrous pericardium c. Visceral serous: covers outside of the heart (epicardium) i. Fused to the fibrous layer 3. Define the atrioventricular groove, anterior and posterior interventricular sulci, apex and base of the heart, anterior, posterior and diaphragmatic surface of the heart. a. Atrioventricular groove: Groove between atria and ventricles b. Anterior interventricular sulcus: Ridge on anterior side between ventricles c. Posterior ventricular sulcus: Ridge on diaphragm side of heart between ventricles Has posterior interventricular a. and middle cardiac v. d. Apex of heart: Inferior “point” of heart e. Base of heart: Superior aspect of heart f. Anterior surface of heart: Sternocostal aspect of heart g. Diaphragmatic surface of heart: Inferior aspect of heart 4. Describe the layers of the heart, relating structure and function. a. Epicardium i. Visceral layer of the pericardium ii. Subepicardium 1. Between epicardium and myocardium 2. Contains fat and major vessels of heart b. Myocardium i. Middle muscular layer ii. Oblique fibers iii. Torsion of chambers c. Endocardium i. Inner lining layer ii. Composed of endothelium backed by thin connective tissue iii. Subendocardium 1. Just outside the endocardium 2. Contains tissues of conducting region 3. First region compromised in myocardial infarction 5. Describe the internal structure of the right atrium including: right atrial appendage, superior and inferior venae cava, crista terminalis, musculi pectinati, coronary sinus, and fossa ovalis. a. Right atrial appendage i. small conical muscular pouch attached to the right atrium b. Superior/inferior vena cava i. Great vein of the heart, comes in from above as superior, and up from below as inferior c. Crista terminalis i. Unique to the right side of the heart ii. Seperates the vena cava sinus of the right atrium from the rest d. Musculi pectinati © 2008 Mark Tuttle 6. 7. 8. 9. 10. i. Hold the valves shut during contraction ii. Bigger in right than left ventricle e. Coronary sinus i. All coronary veins drain into this before going to the right atrium ii. Between the right atrium and right ventricle f. Fossa ovalis i. Vestigial structure where the foraman oval used to be ii. Only in the left atrium Describe the internal structure of the left atrium, including: musculi pectinati, and the left atrial appendage. a. See above Describe the components and locations of the Tricuspid, Mitral and semilunar valves (Aortic and Pulmonary). a. Tricuspid: Between right atrium/ventricle b. Mitral: Between left atrium/ventricle c. Aortic: Between left ventricle/aorta d. Pulmonary: Between right ventricle/pulmonary artery Describe the surface projections and auscultation points for each of the heart valves on the chest wall. a. Aortic valve: 2nd intercostal space on right side of sternum b. Pulmonary valve: 2nd intercostal space on the left side of sternum c. Mitral valve: 5th intercostal space on at midclavicular line d. Tricuspid valve: 5th intercostal space on left aspect of sternum Describe the normal heart sounds. a. S1 i. Lub sound ii. Closure of atriventricular valves (tricuspid, mitral) b. S2 i. Dub sound ii. Closure of semilunar valves iii. Aortic first, then pulmonary iv. Can get “splitting of S2” during inspiration c. S3 i. Early diastole ii. Results from tensing of the chordate tendinae during rapid filling and expansion of the ventricle iii. Normal in children and young adults iv. Sings of pathology in middle aged and older adults v. Pathologic S3 is sometimes referred to as a ventricular gallop d. S4 i. Late diastole ii. Usually indicates presence of disease iii. Generated by the left (or right) atrium vigorously contracting against a stiffed ventricle iv. Sometimes referred to as an atrial gallop Describe heart murmurs and explain valve stenosis and regurgitation. a. Heart murmurs are abnormal heart sounds indicative of abnormally turbulent flow b. Stenosis is narrowing of the arteries that causes turbulent flow © 2008 Mark Tuttle c. Regurgitation is backflow of blood through a valve due to valve problems 11. Describe the internal structure of the right ventricle including: trabeculae carneae, papillary muscles, septomarginal trabecula, and supraventricular crest. a. Trabeculae carnae i. Help keep valves closed b. Papillary muscles i. Help keep valves closed ii. Tug on chordae tendinae c. Septomarginal trabecula i. extends from the base of the anterior papillary muscle to the ventricular septum d. Supraventricular crest i. separates the arterial cone from the rest of the cavity of the right ventricle 12. Describe the internal structure of the left ventricle, including: trabecuale carnea, and papillary muscles. a. Trabeculae carnea i. Trabeculae which line the interventricular septum b. Papillary muscle i. Hold mitral valve closed during contraction 13. Describe infundibulum and conus arteriosus. a. The conus arterious is the narrowing of the ventricle as it transitions into one of the great arteries b. Infundibulum is the conus arteriosus of the right ventricle 14. Describe the fibrous skeleton of the heart. a. Provides a place to anchor the muscles of the heart b. Provides insulation for the electrical conducting system of the heart 15. Describe systole and diastole and relate these events to the normal heart beat and cardiac cycle a. Systole is contraction of the ventricles i. It between lub and dub ii. Between closure ov AV valves and the closure of the semilunar valves b. Diastole is the contraction of the atria i. It is between dub and the next lub ii. Between closure of semilunar valves and AV valves 16. Describe the flow of blood through the heart, comparing and contrasting the pulmonary and systemic circulations. a. Right side deals with deoxygenated blood only i. Receives blood from the vena cava ii. Pumps blood through the pulmonary artery to pulmonary circulation b. Left side deals with oxygenated blood only i. Receives blood from the 4 pulmonary veins ii. Pumps blood to the aorta and to systemic circulation © 2008 Mark Tuttle Conduction system and coronary circulation – Baptista Conduction System: 1. Describe the components and function of the cardiac conduction system including the: sinu-atrial node, atrioventricular node, atrioventricular bundle (bundle of His), right and left bundle branches and the septomarginal fasciculus. a. SA Node i. Pacemaker ii. Located along upper end of sulcus terminalis near iii. Supplied by sympathetic and parasympathetic innervations b. AV Node i. In the interatrial septum adjacent to ostium of coronary sinus inside the Triangle of Koch c. Triangle of Koch i. Roughly triangular area on the septal wall of the right atrium between the: 1. tricuspid valve 2. coronary sinus orifice 3. tendon of Todaro, that marks the site of the AV node d. Bundle of His i. Extends from AV node along the interventricular septum e. Right/left bundle branches i. Branches off of the bundle of His going to each ventricle f. Septomarginal fasciculus i. in the right ventricle, where the conduction system runs to get to the papillary muscle 2. Describe the location of the SA node and AV node. a. See above 3. Describe the interatrial or internodal conducting tracts: a. Bachmann’s bundle to the left atrium i. Originates in SA node ii. Only tract that conducts APs to the left atrium b. Anterior internodal tract (James’s Tract) i. SA node around superior vena cava to join Bachmann’s bundle and continues to left atrium c. Middle internodal tract (Wenckebach’s tract) i. From SA node directly to the AV node passing through the middle marign of crista terminalis d. Posterior internodal tract (Thorel’s tract) i. From the posterior margin of the SA node along the crista terminalis and Eustachian ridge around the coronary sinus ostium into the posterior margin of the AV node 4. Describe the autonomic innervation of the heart and its influence in the regulation of the conduction system and control of the cardiovascular system. a. Sympathetic i. Upper thoracic spinal cord through sympathetic chain to cardiac nerves ii. Directly to ventricular myocardium iii. Can raise heart rate to 230 bpm b. Parasympathetic i. Right vagus nerve to SA node © 2008 Mark Tuttle ii. Left vegus nerve to AV node iii. Vagal tone: slows heart rate to 70-80 bpm 5. Correlate the sequence of excitation of the components of the heart conduction system with a basic electrocardiogram trace image. a. P wave i. Sequential activation of the right and left atria b. QRS complex i. Right and left ventricular depolarization (normally the ventricles are activated simultaneously) c. ST-T wave i. Ventricular repolarization d. U wave i. Origin for this wave is not clear ii. Probably “afterdepolarizations” in the ventricles, repolarization in the atria e. PR interval i. Time interval from onset of atrial depolarization to onset of ventricular depolarization 6. Compare and contrast normal sinus rhythm with sinus bradycardia, tachycardia, heart block and fibrillation. a. Bradycardia: slower than 60 bpm b. Tachycardia: faster than 100 bpm c. Heart block i. Failure of conduction system to transmit signals 1. Bundle branch block (damage to bundle branch) 2. Total heart block (damage to AV node) Coronary Arteries: 7. Describe the origin and course of the right and left coronary arteries and explain the nature of their anastomoses. a. Right coronary artery i. Originates at aortic sinus ii. Courses in coronary sulcus from the aorta toward the region of the posterior interventricular sulcus iii. Depending on left/right dominance, may go down in posterior interventricular branch iv. Branches 1. Right marginal branch 2. Posterior interventricular branch (80%) 3. Sinoatrial branch (55%) 4. Atrioventricular branch (85%) b. Left coronary artery i. Arises from the left aortic sinus ii. Courses in the anterior interventricular sulcus where it divides iii. Branches 1. Anterior interventricular (descending) branch (LAD) 2. Circumflex branch 3. Left marginal branch 4. Posterior interventricular branch (20%) 5. Sinoatrial nodal branch (45%) © 2008 Mark Tuttle 6. Atrioventricular nodal branch (15%) 8. Describe the following branches of the right coronary artery: sinoatrial (SA) nodal artery, right marginal artery, Atrioventricular (AV) nodal artery, terminal branches, posterior interventricular artery and septal branches a. Sinoatrial nodal artery i. Supplied about 50/50 by right/left coronary artery b. Right marginal artery i. Runs along the oblique angle of the heart ii. Supplies the right ventricle c. Atrioventricular nodal artery i. Important contributor to the arterial supply of the AV conducting pathway ii. Important for pathogenesis of heart blockage iii. Usually form right coronary artery d. Terminal branches e. Posterior interventricular artery i. Usually right coronary artery supplied ii. Sometimes left supplied (20%) f. Septal branches 9. Describe the following branches of the left coronary artery: left circumflex artery, anterior marginal artery, obtuse marginal artery, atrial branches and posterior marginal arteries, anterior interventricular artery, anterior diagonal artery and septal branches. a. Left circumflex i. Always present ii. Runs around the left atrium from the anterior side to posterior side b. Anterior marginal artery i. Branch of the right coronary artery ii. Runs along the obtuse angle of the heart? iii. Supplies the right ventricle c. Obtuse marginal artery i. Branch of the left circumflex ii. Supplies the left ventricle d. Posterior marginal branch i. Probably the branch that supplies the right ventricle e. Anterior interventricular artery i. Supplied by the left coronary artery ii. Also known as LAD f. Anterior diagonal artery i. The branches off of the LAD 10. Describe the concept of Dominance of coronary circulation. a. Which one supplies more of the heart 11. Describe the specific tasks required of the coronary circulation and how the coronary circulation is structurally and functionally adapted. a. Needs to supply the heart with blood b. Gets bigger in congestive heart failure and atherosclerosis c. Can adapt with collateral circulation if atherosclerosis happens 12. Define ischemic heart disease and describe the consequences of inadequate blood supply to the heart muscle. a. Reduced blood flow to the heart © 2008 Mark Tuttle b. Heart muscle can die Cardiac Veins: 13. Describe the venous drainage of the heart. a. Everything drains into the coronary sinus b. Small cardiac vein runs with right coronary artery c. Great cardiac vein runs with left coronary circumflex i. Drains LAD d. Middle cardiac vein i. Drains posterior interventricular 14. Describe the coronary sinus and the Thebesian valve (valve of the coronary sinus). 15. Describe the relationship of the coronary sinus and the left atrial wall. a. On inferior aspect 16. Describe the distribution pattern of the tributaries of the coronary sinus: great cardiac vein, middle cardiac vein, oblique vein of the left atrium, and small cardiac vein. a. Coronary sinus i. Left side 1. Great cardiac vein ii. Right side 1. Middle cardiac vein a. Posterior interventricular 2. Small cardiac vein a. Left circumflex © 2008 Mark Tuttle Development of the cardiovascular system – Baptista 1. Compare and contrast vasculogenesis and angiogenesis. a. Vasculogenesis i. Fusion of locally-formed endothelial vesicles b. Angiogenesis i. Outgrowth or branching of preformed vessels 2. List/describe the derivatives of the aortic arches. a. Arch 1 i. Regress ii. Part of maxillary artery iii. Head b. Arch 2 i. Regress ii. Stapedial artery iii. Head c. Arch 3 i. Common and internal carotid arteries ii. Head d. Arch 4 i. Right 1. Proximal right subclavian artery ii. Left 1. Arch of aorta e. Arch 6 i. Right 1. Part of right pulmonary artery ii. Left 1. Part of left pulmonary artery and ductus arteriosis f. Arch 7 i. Right 1. Part of the right subclavian artery ii. Left 1. Entire left subclavian artery g. Dorsal aorta i. Right 1. Regress 2. Middle of the right subclavian artery ii. Left 1. Descending thoracic aorta h. Aortic sac i. Ascending aorta and brachiocephalic artery 3. Diagram the sequential changes that lead to the development of the definitive aortic arch and its branches. a. Neural crest cells play a role in persistence of aortic arches 4. Describe the development errors that result in aortic arch abnormalities. a. Right aortic arch i. Obliteration of the left 4th brachial arch artery ii. Regression of the left dorsal aorta © 2008 Mark Tuttle 5. 6. 7. 8. iii. Problem: ductus arteriosus must now traverse the midline and may constrict the esophagus b. Double aortic arch i. Failure of obliteration of the section of the right dorsal aorta between the 7th intersegmental artery and the junction with the left dorsal aorta c. Interrupted aortic arch i. Obliteration of the left 4th brachial arch artery ii. Only supplies the barchiocephalic trunk and left carotid artery iii. Aorta does not supply lower/left half of body with blood! iv. Ductus arteriosus becomes extremely dilated in order to compensate d. Right subclavian artery anomaly i. Rare ii. Obliteration of right 4th arch arter iii. Comes around from the descending aorta instead of the ascending iv. Passes behind the esophagus and trachea Describe the developmental relationships of the recurrent laryngeal nerves. a. On the right side, the recurrent laryngeal is “free” to migrate upward, just beneath the right subclavian a. because the right 6th aortic arch degenerates b. On the left side, the aortic arch does not degenerate, so it stays right between aorta and pulmonary artery and ligamentum arteriosum Define and describe: cardinal veins (anterior, posterior, common), subcardinal veins, supracardinal veins. a. Cardinal veins i. Anterior (superior) 1. Bring blood from the head via the left and right common cardinal vein ii. Posterior (inferior) 1. Drain the blood form the lower half of the body into the two common cardinal veins iii. Common b. Subcardinal c. Supracardinal Describe the formation of the left brachiocephalic vein, and the ductus arteriosus a. Describe the development errors that result in venous system abnormalities. © 2008 Mark Tuttle Microanatomy of the Circulatory System – Giovannuci 1. Identify the two major components of the circulatory system and their functions. a. Cardiovascular i. Closed system ii. Lined by endothelium b. Lymphatic i. Functions to collect and filter lymphatic fluid ii. Consists of lymphatic vessels, lymph nodes and other lymphatic organs iii. Functions to remove excess interstitial fluid form the extracellular space, filter it and return it to the CV system 2. Identify the components of the cardiovascular and lymphatic systems and integrate the structure with the function of each component. a. Cardiovascular i. Arteries 1. Carry blood away from the heart 2. High pressure 3. Large tunica media 4. Smooth muscle cells on arterioles ii. Microvasculature 1. Exchange of materials between blood and parenchyma iii. Veins 1. Carry blood back to the heart 2. Low pressure b. Lymphatic System i. Drain into larger vessels ii. Contain valves to direct lymphatic fluid back to heart iii. Ducts 1. Thoracic duct a. Starts at level of diaphragm as cistern chili b. Drains 2/3 of body into left subclavian vein where it joins with the left internal jugular vein 2. Right duct iv. Histology 1. Lymphatic capillary a. Internal elastic lamina b. Tunica media has 2 muscle layers c. Tunica adventitia i. Smooth muscle ii. Collagen 3. Describe the three layers of blood vessels and integrate their structural components to specific functions. (Tunica intima, media, & adventitia) a. Tunica intima i. Innermost layer ii. Lined by simple squamous endothelium iii. Composed of: 1. Endothelium 2. Subendothelial connective tissue 3. Internal elastic lamina © 2008 Mark Tuttle a. fenestrated elastic sheet with holes to allow nutrient exchange b. Tunica media i. Consists of smooth muscle cells ii. Also contains: 1. Elastic fibers 2. Type III collagen 3. Proteoglycans iii. In metarterioles, tunica media is basically absent 1. Instead, you just have pericyte layer with some transient contractile ability iv. Most prominent in arteries c. Tunica adventitia i. Outermost laer ii. Dense irregular connective tissue iii. External elastic lamina 1. Seperates the media form the adventitia iv. Contains vaso vasorum 1. Small vessels that supply the wall of large BVs 4. Compare and contrast the structural and functional differences between the various types of vessels, arterial and venous as well as microcirculation. a. Arteries i. Elastic artery 1. Ex aorta, pulmonary artery 2. Initma: thick (20% of total wall) 3. Media: 4-70 layers of elastic sheets, each separated by smooth muscle & CT 4. Adventitia: has vaso vasorum ii. Muscular artery 1. Intima 2. Media: thick, 5-20 layers of smooth muscle cells a. Some scattered elastic lamenae b. Adventitia: Relatively thin iii. Arteriole 1. Intima: may or may not have IEL 2. Media: onl 1-3 layers of smooth muscle cells 3. Adventitia: minimal 5. Integrate the structure of the three types of capillaries with their functional capacities and locations. a. Arteriole i. Feeds the capillary bed ii. Supply either metarteriole or arteriovenous shunt b. Central channel i. Preferred and more direct channel through the capillary bed ii. Metarteriole is the beginning portion 1. Has SMs 2. Slightly larger than true capillary iii. Thoroughfare channel 1. Distal end of central channel 2. Does NOT have SM’s c. Arteriovenous shunt © 2008 Mark Tuttle i. Alternate channel ii. Direct link between arteriole and venule without going through capillaries iii. 2-3 layers of SMs iv. Usually found in skin to bypass superficial capillaries and conserve heat d. Capillaries i. Simple squamous ii. Some areolar CT iii. No tunica media iv. Occasional pericyte v. 5-10 µm diameter vi. Types 1. Continuous a. Most common in muscle b. Connected by tight junctions c. Basal lamina continuous 2. Fenestrated a. Single endothelial cell b. Holes perforating through the cytoplasm c. 60-80nm d. Basal lamina continuous e. Location: endocrine glands, intestinal villi, exocrine pancreas 3. Discontinuous (Sinusoid) a. Larger diameter b. Irregular shape c. Large gaps between endothelial cells d. NO tight junctions e. DISCONTINUOUS basal lamina f. Location: spleen, liver, bone marrow, lymph nodese 6. Integrate the structural components of an arteriovenous anastomosis and the microcirculatory bed to their functions. a. See above 7. Relate the microscopic structure of the heart to its gross anatomy. a. Function: pump b. Same basic layout as great vessels c. Endocardium: Innermost i. Has endothelium (simple squamous) ii. subendocardial CT (contains purkinje fibers, nerves & adipose cells) iii. wraps around all internal structures (trab. Carnae, chorda tendinae, valves) d. Myocardium i. Middle and thickest layer ii. Cardiac muscle iii. Spirals around heart to apex e. Epicardium i. Relatively compared to myocardium ii. CT layer iii. Mesothelium: simple squamous epithelium (visceral layer of serous pericardium) iv. Folds over on itself at great vessels and continues as parietal pericardium © 2008 Mark Tuttle 8. Identify and describe the layers of the pericardial sac and heart wall. Be able to relate them to the function of the heart. a. See above 9. Describe the structural components and functions of the cardiac skeleton. a. “chondround” dense irregular connective tissue with large round cells like cartilage b. Components i. Annulus fibrosus 1. Base of outflow/AV valves and AP valves ii. Fibrous trigones 1. Triangular shaped CT area between valves 2. Right trigone pierced by AV bundle of His iii. Septum membranaceum 1. CT extending downward from trigone into top of interventricular septum 10. Describe the structural components cardiac conduction system and relate them to their function. a. SA node i. Located at junction of SVC with atria b. AV node i. Located in lower left atria in atrial septum by tricuspid valve c. AV bundle of His i. Leaves AV node, pierces right trigone and enters the ventricular septum ii. Divides into the left and right bundle branches in superior portion of septum d. Left & right bundle branches i. Travel down on each side of IV septum to supply the appropriate ventricle e. Subendocardial plexus i. Each bundle branch supplies the impulse to each ventricle ii. Impulse starts at apex of heart and spreads upward towards base 11. Locate and describe the function of the carotid sinus and aortic bodies. a. NOT IN LECTURE 12. Integrate the lymphatic system circulation into the cardiovascular system both structurally and functionally. a. Thoracic duct empties into left subclavian vein b. Right duct empties into right subclavian vein 13. Relate how the following diseases affect the cardiovascular system: varicose veins, Marfan's syndrome, Ehler-Danlos syndrome, atherosclerosis, & aneurysm. a. Vericose veins i. Usually superficial, like saphenous vein in lower extremity ii. Caused by excess pressure in the veins iii. Perhaps faulty valves b. Marfan’s Syndrome i. Autosomal dominant ii. Messed up FBN1 gene for fibrillin iii. Can result in mitral/aortic valve prolapse c. Ehler-Danlos i. Collagen disorder d. Atherosclerosis i. “hardening of the arteries” e. Aneurysm © 2008 Mark Tuttle i. aortic aneurysm is a general term for any swelling (dilatation or aneurysm) of the aorta, usually representing an underlying weakness in the wall of the aorta at that location © 2008 Mark Tuttle Cardiac Development – Baptista 1. Define and describe a. endocardial tube i. forms from two portions of splanchnic mesoderm ii. primordial heart tube b. myoepicardial mantle and derivative i. forms around the endocardial tube out of mesenchyme ii. becomes myocardium and epicardium iii. separated from the future endocardium by cardiac jelly c. cardiac jelly i. seperates the myoepicardium from the endocardium ii. becomes the subendocardial tissue d. endocardial cushions i. above and below AV canal ii. thickenings of the subendocardial tissue which develop in the region of the atrioventricular canals iii. Eventually grow together and fuse. iv. They serve two important functions: 1. form AV canal 2. provide a "scaffold" to which the interatrial septae and the interventricular septum will grow towards and fuse with 2. Describe formation of the: a. mesodermal germ layer i. Cells from the anterior part of the lateral plate mesoderm are what give rise to the precardiogenic mesoderm. This precardiogenic mesoderm constitutes a horse-shoe shaped region of the mesoderm that extends alongside the foregut. Neighboring endoderm cells are what induce formation. The heart is derived from the splanchnic mesoderm, and starts as bilateral tubular primordial, which are located ventrolateral to the early pharynx. b. cardiogenic plate i. anterior lateral plate mesoderm ii. as mesoderm splits into splanchnic and somatic, a cardiogenic plate is recognizable in the splanchnic mesoderm rostral to the oropharygeal membrane c. embryonic folding i. Embryonic head and lateral foldings have a great impact of heart development. (begins Day 20): Lateral and cephalic folding of the trilaminar germ disc over the course of several days brings the endocardial tubes together and tucks them ventrally in the thoracic region at the base of the yolk sac. This process also brings the septum transversum into its adult position inferior to the heart. 3. Describe early development of the primitive heart tube. a. Endocardial cardiac jelly form both sides migrates and will meet in the middle and fuse 4. Describe and discuss the relationship between: a. Sinus venosus i. Attaches to the vitelline, cardiac, umbilical systems ii. Bottom-most part of primitive heart tube b. Primitive atrium i. Just above bottom-most part. Forms common atria c. Primitive ventricle © 2008 Mark Tuttle 5. 6. 7. 8. 9. 10. i. Will eventually form the left ventricle d. Bulbus cordis i. Includes the truncus and conus (conus arteriosis) segements of the primitive heart tube ii. Will form the right ventricle e. Truncus arteriosus. i. Top-most part just below the aortic sac ii. Part of the bulbous cordis Define aortic sac and explain its relationship to the truncus arteriosus and aortic arches. a. Top most part, above truncus arteriousus b. Forms the ascending aorta and brachiocephalic artery Explain the process of looping of the heart. a. Atrium and sinus venosus come to lie dorsal to the bulbus cordis, truncus arteriosus and ventricles Describe partitioning of the atrioventricular canal, primordial atrium and ventricle. a. Atrium becomes partially separated from ventricle by formation of thickened AV cushions b. Cushions grow and eventually fuse c. AV canal migrates as ventricles enlarge in order to keep it centered d. Later partitioning i. Separation of atria from ventricles ii. Partition of atria Describe partitioning of the bulbus cordis and truncus arteriosus. a. Partitioning of the outflow tract begins with continuous sets of ridges in the bulbus cordis (bulbar ridges) and truncus arteriosus (truncal ridges). They grow toward each other while spiraling 180 degrees. They then fuse to form a spiraling aorticopulmonary septum, dividing aorta & pulmonary trunk. Bulbar ridges are also involved in forming the IV septum. Both the ridges are derived from neural crest cells. Describe development of the cardiac valves and conducting system of the heart. a. AV valves: form from cushion i. Myocardium atrophies a but and leaves cordae tendonae and papillary muscles ii. By 50 days, muscular cords are formed, which eventually fully become chordae tendinae and papillary muscles by 60 days. At the same time, the endocardial cushions, which originally were separating the Atria and ventricles, are remodeled to form AV valves. b. Semilunar i. Neural crest cells migrate inward and close off truncus unto 2 cavities ii. Neural crest cells actually just INDUCE this to happen, they don’t do it themselves c. Conducting i. Neural crest gives rise to everything ii. Sympathetic, parasympathetic, and cardiac ganglion iii. Conducting system is poorly understood Describe the normal fetus blood circulation and the changes that occur when a newborn switches from fetal to adult-type blood circulation. a. Fetal circulation artery/vein blood oxygenation is reversed! b. Ductus venosus i. Regulates how much of maternal blood reaches fetal circulation ii. Protects it in the event that mother is giving too much blood (ex. High maternal blood pressure) © 2008 Mark Tuttle iii. Becomes ligamentum venosum c. Ductus arteriosus shunts blood from pulmonary trunk to aorta i. In fetus, R side pressure is much higher ii. Pressure differential disappears at birth and lungs secrete rediokinins which help constrict ductus arteriosus d. Foramen ovale i. Septum premium, septum segundum, ostium premium/secundum, cushions ii. When pressure differential changes, septum premium closes © 2008 Mark Tuttle Introduction to the Autonomic Nervous System – Bennett-Clarke 1. Define: a. Somatic efferent i. Non autonomic nerve which controls motor innervation b. Somatic afferent i. Non autonomic sensory nerve c. Visceral efferent i. Autonomic nerve which controls innervation of: 1. Smooth muscle 2. Cardiac muscle 3. Exocrine glands 4. Sweat glands d. Visceral afferent i. Autonomic sensory innervation ii. More stretch then touch iii. Can feel pain but it is a different kind of pain e. Effector i. Whatever is innervated by a given nerve ii. Example: smooth muscle, cardiac muscle or glands 2. Compare the structural differences between the somatic and the autonomic components of the peripheral nervous system. a. Autonomic nervous system has a preganglionic fiber and postganglionic fiber with a synapse in the ganglion i. Except for adrenal medulla sympathetic nerve which is just like a somatic nerve b. Somatic motor system has one nerve going all the way to its effector 3. Compare the sympathetic and parasympathetic divisions of the ANS. How are these two similar? How are they different? a. Sympathetic is “fight or flight” i. Vasoconstrict in core ii. Increase respiration rate iii. Increase heart rate iv. Dilate iris b. Parasympathetic is “rest and digest” i. Slow heart rate ii. Slow respiration rate c. Both are autonomic and come from lateral horn of spinal cord (or from cranial nerves for parasympathetic) d. Sympathetic and parasympathetic use ACh as the neurotransmitter i. EXCEPT sympathetic postganglionic nerves e. Both innervate organs f. Parasympathetic innervates mucus glands/lacrimal glands exclusively g. Sympathetic innervates BVs, sweat glands, SM erector pillae exclusively h. Sympathetic ganglia are part of the sympathetic trunk whereas parasympathetic ganglia can be “named” ganglia 4. Be able to diagram a “typical” visceral efferent path for both the sympathetic and parasympathetic division of the ANS. a. Sympathetic © 2008 Mark Tuttle i. Exits lateral horn T1-L2, travels through white ramus, synapses at paravertebral ganglion, postganglionic fiber exits via grey ramus and joins ventral or dorsal ramus ii. Exits lateral horn T5-L2, travels through white ramus through paravertebral ganglion (but does not synapse), continues down splanchnic nerve to prevertebral ganglion, where it synapses (named ganglion), postganglionic fiber continues on to abdominal or pelvic viscera iii. Exits lateral horn T8-T12 travels through white ramus, continues without synapsing through paravertebral ganglion, splanchnic nerve and prevertebral ganglion, finally synapses on suprarenal medulla 1. No postganglionic fiber 2. Does this so it can secrete ACh as its neurotransmitter 5. List four possible terminations for the preganglionic sympathetic fiber. a. Paravertebral ganglion at same level b. Paravertebral ganglion at different level c. Prevertebral ganglion in abdomen d. Suprarenal medulla 6. What is a pelvic splanchnic nerve? Describe the course and termination for a pelvic splanchnic. a. A pelvic splanchnic nerve arises from the parasympathetic nervous system of S2-S4 b. It exits the ventral ramus and goes to a terminal ganglion before synapsing and then innervates: i. Descending colon ii. Bladder iii. Urethra iv. Sex organs v. External genetalia © 2008 Mark Tuttle Lymphatic System - Howard 1. Be able to identify the tissues and cells of the lymphoid system. a. Cells i. Helper T cells 1. Identified by CD4 2. Stimulate differentiation of B cells ii. Cytotoxic T cells 1. Identified by CD8 2. Perform cell lysis iii. B cells 1. Effector only 2. 150,000 IgM on surface b. Tissue i. Specialized connective tissue 1. Reticular connective tissue a. Form the stroma 2. Cells in between reticular fibers a. Lymphocytes, macrophages, plasma cells, antigen-presenting cells 3. Lymphatic vessels c. Thymus i. Where T cells mature ii. 2 lobed structure iii. Cortex 1. Tightly packed lymphocytes & macrophages 2. Self-recognizing T-cells are killed off here 3. Double layer sperates cortex/medulla iv. Medulla 1. Reticular epithelial cells produce thymic hormones 2. Hassall’s corpuscles *DIAGNOSTIC v. Functions 1. T cells mature 2. T cells become immunocompetent 3. Develop tolerance (avoidance of self-recognition) 4. T-cells proliferate a. Thymosin b. Thymopoietin c. Thymulin d. Thymic humoral factor 2. Know the functions of the various cells of the lymphoid system. a. Cortex i. Type I epithelial reticular cell: Isolate cortex from body Occluding ii. Type II epithelial reticular cell: Divide cortex into pockets Desmosomal iii. Type III epithelial reticular cell: Corticomedullary junction Occluding Isolates cortex/medulla b. Medulla i. Type IV epithelial reticular cell: Corticomedullary junction ii. Type V epithelial reticular cell: Framework of medulla iii. Type VI epithelial reticular cell: Hassall’s corpuscles *DIAGNOSTIC © 2008 Mark Tuttle 3. Be able to trace cells of the lymphoid system within the body. a. 4. Know the functions of the tissues of the lymphoid system. a. It absorbs and transports fatty acids and fats as chyle to the circulatory system b. The last function of the lymphatic system is the transport of antigen presenting cells (APCs), such as dendritic cells, to the lymph nodes where an immune response is stimulated 5. Be able to distinguish cellular from humoral immunity. a. Cellular immunity i. T-cell immunity ii. Delayed hypersensitivity iii. Inflammation at site iv. Recruitment of macrophages, natural killer cells, cytotoxic T cells b. Humoral immunity i. B-cell immunity (immunoglobulins) ii. Immediate hypersensitivity iii. Antibodies in circulation iv. Antibodies inactivate or destroy foreign invaders 6. Be able to describe basic immune responses. 7. Compare and contrast structure-function relationships between the lymphoid organs. © 2008 Mark Tuttle Congenital Heart Defects – Baptista 1. List the most commonly encountered congenital cardiac malformations. a. Ventricular Septal Defect (VSD) 25-30% b. Atrial Septal Defect (ASD) 10-15% c. Patent Ductus Arteriosus (PDA) 10-20% d. Tetrology of Fallot 6-15% e. Pulmonary stenosis f. Coarctation of Aorta g. Aortic stenosis h. Transposition of the great arteries i. Truncus arteriosus j. Tricuspid atresia 2. Classify the congenital cardiac malformations according to structural anomalies. 3. Describe the development errors that take place in the heart resulting in left-to-right shunt. a. Any hole in the atrium or ventricle or aorta which results in higher pressure arterial blood going toward the lower pressure venous system i. VSD ii. ASD iii. PDA iv. Post-ductal Coarctation of Aorta 4. Describe the development errors that take place in the heart resulting in right-to-left shunt. a. Tetrology of Fallot b. (Pre-ductal Coarctation of Aorta) 5. Describe the development errors that take place in the heart causing anomalies of the outflow tract. a. Aorta migrates too far during development b. Compresses pulmonary artery i. Pulmonic stenosis results ii. Right ventricle hypertrophy because of high pressure load iii. **Right-to-left shunt c. Cushions do not close, causing VSD d. Cyanosis is reversed during squatting i. Decreases venous return because blood is trapped in the legs ii. Right ventricle pressure drops iii. Left ventricle pressure increases iv. More oxygenated blood in the aorta e. Systolic murmur heard best at the upper left sterna border 6. Describe and compare the clinical consequences of: a. Patent Ductus Arteriosus i. Congestive heart failure ii. Cyanosis of the lower extremities iii. Continuous murmur b. Coarctation of Aorta i. 2:1 male/female ratio ii. Blood flow to head is normal iii. Pre-ductal: Cyansis in lower extremities iv. Post-ductal: NO CYANOSIS c. Transposition of Great Arteries © 2008 Mark Tuttle i. Abnormal growth and absorption of subpulmonary ii. Cyanosis presents on birth iii. As ductus arteriosis closes, death results 1. Can keep baby alive by keeping ductus open d. Atrial Septal Defect i. Most infants are asymptomatic ii. Dectected by a murmur when becomes school age iii. Most common symptom in an adult is heart palpitations e. Ventricular Septal Defect i. Membranous 1. Most common 2. Cardiac cushions degenerate 3. Occurs near top ii. Muscular 1. Can occur in places other than near top/cusions f. Tetralogy of Fallot i. Dyspnea on exertion ii. “spells” may occur following feeding 1. This is one of the only times babies exert themselves iii. Children alleviate symptoms by squatting iv. Mildly cyanotic b/c of pulmonary stenosis g. Persistent Truncus Arteriosus i. Absence or incomplete partitioning of truncus arteriosus ii. Degree of cyanosis depends on the varying degree of contribution of the right ventricle to the aorta iii. Usually little or no cyanosis initially 1. Later on, it can develop along with pulmonary vascular disease, polycythemia, and clubbing of the fingers iv. Heart failure v. Recurrent respiratory tract infections