Gastro35-GISecretionsI

GI #35
Fri, 02/28/03, 9am
Dr. Gwirtz
Jennifer Uxer for Margaret Veach
Page 1 of 8
Gastrointestinal Secretions
I. Introduction
A. Types of secretions
Salivary
Esophageal
Gastric
Pancreatic
Biliary
Intestinal
B.
Objectives
Describe the formation of the primary secretion: saliva, gastric, pancreatic, bile, intestinal. Salivary and pancreatic glands have primary secretions from acinar cells. These secretions are modified in the secretory ducts; the amount of modification is dependent upon the rate of secretion.
Describe the modification, if any, to the secretion by ductal cells
Functions of the secretion
Stimulus for release of the secretion
Inhibition of release of the secretion
Regulation of secretion
During the 4 phases: interdigestive phase, cephalic phase, gastric phase, intestinal phase
3 methods of control: neural, hormonal, local
Define: alkaline tide, acid tide, proenzyme
List the major types of digestive enzymes produced by the pancreas
Describe the enterohepatic circulation of bile salts and its physiologic significance
Explain diseases and disorders
Acute and chronic gastritis
Describe the pathophysiology of peptic ulcer disease
Mechanisms of diarrhea
Pancreatitis
II. Types of Secretions in the GI tract
1.
Enzymes: salivary α-amylase, pepsin, brush border enzymes
2.
Water, electrolytes: found in salivary secretions, and in those from the Crypts of Lieberkuhn
3.
Mucus—from goblet cells in many different regions
Importance of Mucus
Adheres to particles
Coats the wall of the gut—protection
Low resistance for slippage—makes it easier for the bolus of food to slip through the esophagus
Causes fecal particles to adhere to each other
GI #35
Fri, 02/28/03, 9am
Dr. Gwirtz
Jennifer Uxer for Margaret Veach
Page 2 of 8
Resistant to enzyme digestion—protects the stomach and upper duodenum from enzyme effects
Amphoteric properties (buffers acid)
4.
Hormones/Paracrines from specialized cells
III. Saliva and Salivary Glands
A.
Salivary Glands
1. Parotid—Serous secretion
2. Submandibular, submaxillary—Serous and mucus secretions
3. Sublingual—Serous and mucus secretions
4. Buccal—Mucus secretion
B. Characteristics of Saliva
1-1.5 liters secreted daily; amount is increased during digestion
pH 6.0 - 7.4;
hypotonic relative to plasma
; it’s slightly acidic to neutral. All other secretions are isotonic relative to plasma.
Serous secretion contains alpha-amylase (ptyalin—old name) which begins digestion of starches
Primary secretion by acinar cells is modified by salivary ducts
Ionic concentrations vary with rate of secretion of saliva
Acinar serous cells—look like bunches of grapes and secrete digestive enzymes in a serous solution—the primary secretion.
Mucus cells—mucin
Intercalated duct cells—are the initial part of the duct and secrete protein
Striated duct—modify primary secretions by either secreting or absorbing an ion; influenced by aldosterone. Aldosterone is involved in blood volume regulation. ↓ blood flow → renin → angiotensin II → stimulate adrenal cortex → release aldosterone → salivary ductile cells (& kidneys) reabsorb
Na
+
→ water follows Na
+
→ ↑ volume → restore (blood) pressure
Excretory duct - modify secretions; secrete factors (epidermal growth factor, enzymes)
C. Functions of Saliva
Moisten, lubricate mouth to make it easier to talk and swallow
Excretory: urea, sugar, mercury, lead)
Buffer stomach acid
Kill bacteria in mouth via antibacterial and immunologic agents
Begin digestion of foods: salivary α-amylase; salivary lipase—very minor effect
D. Formation of Saliva
1. Stage One:
Formation of a primary secretion containing
-amylase,
-lipase, mucous and ions: Na
+
, Cl
-
, K
+
, HCO
3
-
Rate of secretion can increase 20 X (parasympathetic stimulation); begin cephalic phase → ↑ parasympathetic stimulation→ ↑ acinar secretions
GI #35
Fri, 02/28/03, 9am
Dr. Gwirtz
Jennifer Uxer for Margaret Veach
Page 3 of 8
From picture: In the end of the duct in the acinar cells is the amylasecontaining primary secretion (nearly isotonic; levels Na
+
, Cl
-
, K
+
, and
[probably] HCO
3
-
similar to plasma. Secretion then flows through striated and excretory ducts where it is modified. How it is modified is influenced by aldosterone, which affects the Na
+
pump causing more
Na
+ to be absorbed. Na
HCO
3
— secretion
+ —absorption, Cl — absorption, K
+ —secretion,
Note that striated and excretory ducts are impermeable to water.
So, there’s an absorption of ions without water following. This yields a hypotonic solution.
2. Stage Two:
Modification of primary secretion in the salivary ducts; process affected by rate of secretion
Na
+
actively reabsorbed - influenced by aldosterone; 3 Na
+
absorbed for every 1 K
+
excreted
K
+ actively secreted, but at slower rate (in exchange for H
+
)
Cl
- passively reabsorbed with Na
+
HCO
3
-
secreted and in exchange for Cl
-
ducts impermeable to water
E.
Effect of saliva flow rate on electrolyte composition (graph)
1.
At the resting basal state, there’s no parasympathetic stimulation
Na + levels are low because the secretion has been sitting in the duct a long time, so the Na
+
has been absorbed. Cl
-
is also absorbed.
K
+
is at its highest level.
2.
Simulate salivation
Stimulate parasympathetic nerve activity
↑ rate of secretions; ↓ time the secretion spends in the salivary duct
Now, there’s less time for modification, absorption, and secretion, so
[Na + ] ↑, [Cl ] ↑, [K + ] ↓
Also have an ACTIVE release of HCO
3
-
F.
Neural Regulation of Salivation
Salivation is controlled strictly by neural control!
Parasympathetic nervous signals from the salivatory nuclei in the brainstem;
PSN stimulates salivary glands to secrete. Sympathetics have a small effect: initially they increase salivation. Over time, when more Norepi has been released, there’s less water available to make the secretions, and salivation decreases.
Hormones only modulate (not control) reconditioning in ducts— aldosterone increases Na
+
absorption
Stimuli—taste, tactile, thought, smell, GI irritation
Influenced by stimuli from other CNS centers, reflexes (vomiting, nausea)
Rate of secretion: Basal (when sleeping—note you drool because you don’t swallow)= 30 ml/hr; Maximal = 400-600 ml/hr
GI #35
Fri, 02/28/03, 9am
Dr. Gwirtz
Jennifer Uxer for Margaret Veach
Page 4 of 8
G. Cellular Mechanisms of Evoking Salivary Secretion—don’t memorize the picture. Know the following points.
Norepinephrine
-adrenergic receptor
IP
-adrenergic receptor
cAMP
amylase rich secretion
IP i
3
[Ca
Acetylcholine—Major mechanism
++ i
]
volume
]
volume secretion
3
[Ca
++
Substance P
IP
3
[Ca
++ i
]
volume secretion
Key:
cAMP &/or
Ca ++ i will increase salivation
H. Case Study: Salivation
A 60 year old woman complains of a persistent dry mouth and difficulty in chewing and swallowing. Food seemed tasteless because taste buds aren’t stimulated as much without watery fluid; eyes dry & gritty. Gums & teeth inflamed and infected, tongue lobulated.
Dx: xerostomia
Affects 2% of population
Variety of causes: medication (esp. tricyclic antidepressants and simpathomimetics—decongestants), head & neck irradiation, auto-immune inflammatory diseases , such as Sjogren’s syndrome
Findings: atrophy of acinar tissue, ductal hyperplasia
Consequences: oral & dental—dry mouth, inflamed gums
Treatment: artificial salivas; low dose pilocarpine (parasympathetic stimulant)
IV. Esophageal Secretion
Mucous
Main body of esophagus is lined by simple mucous glands
Gastric end contains many compound mucous glands that produce alkaline, thick, gelatinous secretions. Important in protection esophagus from digestion by reflux of gastric juices into the lower esophagus
V.
Gastric Secretions
Mucus secreting cells (cardiac glands)
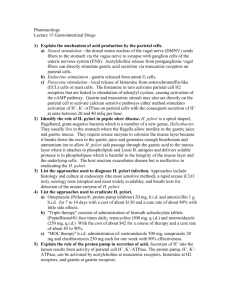
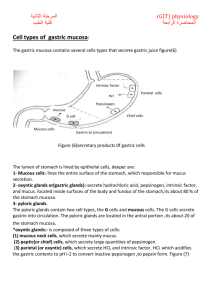
A. Oxyntic or gastric glands - body, fundus of stomach
1. Parietal (oxyntic) cells—secrete acid (HCl) and intrinsic factor into the duct and they percolate into the lumen
2. Chief cells (peptic)—secrete pepsinogen, a protease. It’s secreted in this inactive form so that it does not digest the cells of the organ.
3. Mast cells (enteroendocrine)—secrete histamine, which regulates acid secretion by the parietal cells
B. Pyloric glands - antral region of stomach
Secrete mucus
Some pepsinogen
Most important: gastrin (G cells) — regulate acid secretions by parietal cells
GI #35
Fri, 02/28/03, 9am
Dr. Gwirtz
Jennifer Uxer for Margaret Veach
Page 5 of 8
Somatostatin (D cells)—paracrine agent; secreted when the stomach is too acidic; inhibit parietal cells through negative feedback
C. Cardiac glands—mucus secreting cells
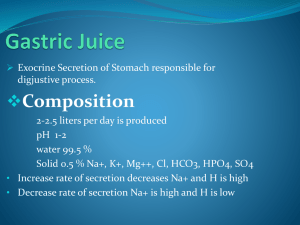
VI. Gastric Acid
A. Concentration of Ions in Gastric Juice as a Function of Rate of Secretion (graph)
Basal period: [H + ] is very low; [Na + ] is at its highest. Non-parietal cell secretions account for this.
Stimulate stomach to secrete: [H
+
] ↑; [Na
+ ] ↓ This is NOT due to a Na-H exchange! Parietal cell secretions are added to the non-parietal cell secretions, so lots of H + is added overwhelming the Na +
B. HCl Formation and Secretion by Parietal Cells—1 of most important secretions
1. Formation of HCl
160 mOsm/L
pH 0.8
1500 cal required to synthesize 1 L—lots of calories are needed to form the H + in this acid
2. Electrolyte composition changes with secretion rate. Basal (interdigestive) stat is different than the secretions at a maximum rate.
3. Composition: H
+
, K
+
, Na
+
, Cl
-
, water
4. Severe / prolonged vomiting causes a metabolic alkalosis—loss of H
+
, K
+
(hypokalemia), water (hypovolemia), saliva
5. Postulated mechanism of HCL secretion (picture)
Carbonic acid is formed by CO
2
(from digestion) and H
2
O with the addition of carbonic anhydrase.
The acid is broken down to H + + HCO
If the proton pump is blocked, acid secretion is blocked.
HCO
3
-
3
. This is the H + that’s secreted.
is pumped into the venous blood in exchange for Cl . So, the pH of the venous blood draining the stomach is slightly alkaline in digestion: alkaline tide.
Carbonic anhydrase is used in saliva, gastric acid, parietal bicarbonate formation.
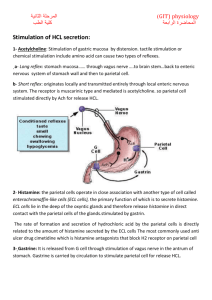
C. Regulation of Gastric Acid Secretion—more complex because it has lots of control
1. Cephalic Phase 30-40% of acid secretion
Neural (via ACh and GRP/bombesin)
If you cut parsympathetic nerves, you completely eliminate the cephalic phase.
2. Gastric Phase 50-60% of acid secretion
Occurs when swallowed food is in the stomach
Neural (distension)—via vagus, submucosal plexus
Hormonal (gastrin)—released in response to vagus, digested proteins, alcohol, Ca
++ —these directly stimulate G-cells
If lumen pH < 3 (inhibit—via somatostatin). Stimulates D-cells in the pyloric region to release somatostatin—this decreases gastrin secretion
GI #35
Fri, 02/28/03, 9am
Dr. Gwirtz
Jennifer Uxer for Margaret Veach
Page 6 of 8 and decreases parietal cell stimulation, thus decreasing the amount of acid released.
3. Intestinal Phase 10% of acid secretion
Most of the response of the intestine is to inhibit acid secretions
Circulating amino acids, duodenal gastrin (stimulate)
Neural reflexes (inhibit - via somatostatin)
Hormonal—mediated by vagal and submucosal n. (GIP, CCK (released in response to fat), secretin (inhibits acid and gastrin secretion) - inhibit).
These also inhibit gastric mobility
4. Interdigestive Phase—lowest rate of secretion
D. Major Mechanisms for Stimulation of Gastric Acid Secretion (Table 38-1)
Phase Stimulus Pathway
Cephalic Vagal reflex 1. Parietal cells
2. G cells
Gastric Gastric distention
Intestinal Protein digestion products in duodenum
Submucosal reflex, local and vagovagal reflexes to:
1. Parietal cells
2. G cells
1.
2.
Intestinal G cells
Intestinal endocrine cells
E.
Major Mechanisms for Inhibition of Gastric Acid Secretion
Region Stimulus Mediator
Antrum
Duodenum
Acid (pH < 3.0)
Acid
None, direct
Secretin
Bulbogastrone
Nervous reflex
Inhibit gastrin release
+
+
+
Stimulus to parietal cell
Acetylcholine
Gastrin
Acetylcholine
Gastrin
Gastrin
Entero-oxyntin
Inhibit acid secretion
+
+
+
Duodenum &
Jejunum
*Hyperosmotic solutions
*Fatty acids, monoglycerides
*Unidentified enterogastrone
*GIP
*CCK
*Unidentifed enterogastrone
+
+
+
+
+
F. Neural Regulation of Gastric Acid Secretion
1. Vagus nerves (release ACh) to enteric nervous system
Stimulate ACh receptors on parietal cells causing acid release.
Vagus innervates the G cell, and its neurotransmitters are ACh and
Bombesin.
GI #35
Fri, 02/28/03, 9am
Dr. Gwirtz
Jennifer Uxer for Margaret Veach
Page 7 of 8
Vagal fibers release bombesin (Gastrin Releasing Peptide)
gastrin from G cells
If you give atropine, you block the cholinergic receptors, but wouldn’t completely block this due to the bombesin release.
2. Stimuli include:
Cephalic phase (thought, smell, sight, presence of food in mouth, taste)
Distention of stomach
G. Gastrin Regulation of Gastric Acid Secretion
Gastrin secreted by G cells in antrum into blood stream (hormone)
Stimulate gastrin receptors on parietal cells
acid secretion
Stimuli for release: vagal stimulation, distension, proteins, peptides, amino acids from chyme, Ca
++
, alcohol
If a patient is prone to gastric ulcers, they need to avoid Ca
2+
and alcohol to limit the gastric acid release. They should use magnesium based antacids rather than calcium based.
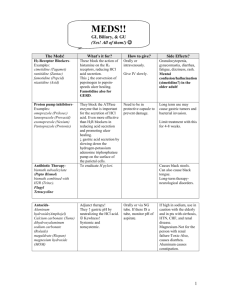
H. Regulation of Gastric Acid Secretion
1. Histamine: stimulate H
2
receptors on parietal cells; released from mast cells; potentiates (magnifies) secretion produced by ACh & gastrin
Quick note on potentiates: this is to magnify the result of. If Ach causes a 2x increase and histamine causes a 2x increase, then together they can cause a
6 – 8 x increase. This is not a linear relationship because 1 magnifies the other.
Vagal stimulation of histamine released by the H
2
cells—reason H
2 blockers work well
Gastrin
Other
2. Feedback inhibition: (via inhibition of gastrin by somatostatin from antral D cells) when lumen pH < 3.0
3. (Picture) Drugs to block the 3 receptors on the parietal cell that stimulate
H
+
formation
Atropine and anticholinergic drugs block the muscarinic receptors for
ACh.
Cymetadine and tagamet block the H
2
receptors for histamine. These decrease acid secretion by don’t block the H +
pump. Must block this pump to completely stop the acid secretion.
Gastrin receptor blockers are not used clinically because they have too many side effects.
Prilosec is an H
+
pump blocker.
GI #35
Fri, 02/28/03, 9am
Dr. Gwirtz
Jennifer Uxer for Margaret Veach
Page 8 of 8
I. Gastric Acid Output—don’t memorize the chart
Acid Output (mEq/hr) Serum Gastrin
Condition
Normal
Pernicious Anemia
Basal
1-5
0
Maximal
6-40
0
(pg/ml)
35
350
Gastric Cancer
Gastric Ulcer
Duodenal Ulcer
Gastrinoma
0-5
0-3
2-10
10-30
0-40
1-20
15-60
30-80
50
500
At a basal rate, there are low acid secretions
If there’s atrophy of parietal cells, no acid is produces. Also, no intrinsic factor is released, so no vit B12 is absorbed. This leased to pernicious anemia and high secretin levels.
Gastric ulcers—not due to hypersecretion of acid. Actually have decreased acid levels, so they’re due to something else.
Duodenal ulcers—due to hypersecretion of acid
Gastrinoma—Sjogren’s syndrome—tumors, usually in pancreas. These tumors secrete HUGE amounts of gastrin causing hypersecretion of acid.