Chapter 3- Third Trimester Measurements
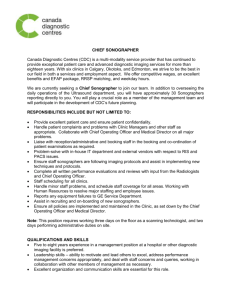
advertisement

Chapter Three THIRD TRIMESTER MEASUREMENTS: An Inter/Intra Sonographer Evaluation of Accuracy 3.1 Introduction “From twenty five weeks to term, measurements do not necessarily relate to the period of gestation but simply give a comparison to the mean values for the population at large. The variation among normal fetuses is considerable, and in the third trimester a variation of three weeks size on either side of the mean value may be seen.” Garrett and Robinson Third trimester pregnancy ultrasound assessment of fetal size is a common component of obstetric care. Of particular importance are those pregnancies deemed to be at greater risk with gestational diabetes, maternal hypertension, macrosomia, or intra uterine growth retardation. Although the accuracy of ultrasonic fetal measurements for weight estimation was questioned by, amongst others, Sarmandal et al (1989) and also the British Medical Ultrasound Society (BMUS) Fetal Measurements Working Party (1990), many clinicians compare their clinical estimation with the ultrasonic result. As ultrasound practitioners it is important to perform fetal measurements accurately and reproducibly so that when the figures are used for serial assessment of growth, or are applied to a fetal weight formula, the results may be more reliable. These measurements may impact on the outcome of a pregnancy (Dudley and Chapman 2002) with the decision to intervene often based on the ultrasound findings. It is therefore essential to 111 perform fetal parameter measurements, at all stages of pregnancy, in a consistent and reproducible way. Anderson et al (1995) assessed ultrasonic prenatal diagnosis of fetal anomalies, concluding that 2% of all pregnancies had an anomaly. Dudley and Chapman noticed that over 90% of all antenatal ultrasound journal articles were written about these 2% of anomalies and that fetal measurements and quality control, which affects every ultrasound examination, was almost neglected. It has only been as recently as May 2001 that the Australasian Society for Ultrasound in Medicine (ASUM) recommended the use of ultrasonic fetal measurement charts based on an Australian population, to help standardize fetal size/growth reporting. Previously a combination of different charts by, amongst others, American sonologists Hadlock and Deter (1982) were used which made it difficult for an obstetric patient being scanned at different practices, to get the most reliable assessment of fetal growth. In Australia sonographers perform fetal measurements for gestational age and fetal growth and weight evaluation. All sonographer training establishments in Australia require a high standard of obstetric scanning ability, with particular reference to obtaining the correct imaging plane and measuring of the individual fetal parameters before registration as an accredited medical sonographer (AMS) with the Australasian Sonographer Accreditation Register (ASAR). To remain registered sonographers must undertake ongoing continuing professional development via conferences, seminars, workshops or individual journal reading with the aim of maintaining an acceptable skill level. Of particular importance is that their ability to competently scan and measure a 112 fetus for size and growth remains, with a high inter and intra sonographer measuring accuracy level. As discussed in Chapter Two the relevant head image required for the measurement of the biparietal diameter (BPD), occipito-frontal diameter (OFD) and head circumference (HC) is a transverse axial plane, which includes the falx cerebri anteriorly and posteriorly, cavum septum pellucidum anteriorly in the midline, and the thalami (Image 3/1). The BPD should be measured at the widest point of the head from the outer edge of the nearest parietal bone to the inner edge of the more distant parietal bone and the OFD perpendicular to the BPD from mid to mid occipital bones. The head circumference should be traced either with an ellipse mode or manually around the outer perimeter of the skull. In late pregnancy it can be difficult to obtain the ideal imaging plane due to the head lying low in the pelvis. The imaging plane for the abdominal circumference (AC) is a true transverse cut at the level of the fetal liver and stomach, including the left portal vein at the umbilical region. Although the AC can be measured using the ellipse mode, in the third trimester it is usually more precise to manually trace the perimeter of the abdomen, including the fat layer. Long bones should be imaged in the axial plane to achieve the longest length, with clean blunt ends and a strong acoustic shadow behind the bone (Image 3/5). Measuring must be along the diaphyseal shaft, excluding the epiphysis. 113 3.2 Aims of Objective Two The aim of this study was to assess inter and intra-sonographer measurement reproducibility of fetal variables in late pregnancy and to detect any common pitfalls of measuring that could affect the report on fetal size. 3.3 Methodology Using an HDI 5000 Ultrasound system (Philips Medical Systems), images were captured for measurements of the BPD, OFD, HC, AC and long bones. Three images of a head, abdomen and femur, were deliberately suboptimal, taken at awkward imaging planes to reflect the difficulty of always obtaining ideal images to measure in late pregnancy. Two pregnancies in the final 6 weeks of gestation were chosen for imaging and the dates were confirmed based on the LMP and scans at both 12 and 19 weeks gestation. The ASUM 2001 Fetal Measurement Charts were used to estimate size. Eighteen images from these two pregnancies were archived twice on to an optical disc. This gave a total of 36 images to be measured. The optical disk was copied and distributed to 20 Medical Imaging Australasia (MIA) practices throughout Australia where HDI 5000 or 3000 systems were installed. Images were downloaded from the optical disc to the hard drive of each ultrasound machine, and the systems recalibrated for measuring imported images. Following a point-by-point list of system instructions (Appendix 5), sonographers scrolled through the collection of images, measured the variables as prompted, and recorded the results both onto film and data sheets. 114 Sonographers were asked to measure all images, even those deliberately taken at awkward angles that they may not normally image. This was important, as difficult fetal positions and perceiving edges for measuring are a reality in obstetric ultrasound. To assess inter & intra-sonographer reproducibility, sonographers, both qualified and unqualified (students), sequentially measured the 36 images. Intra-sonographer reproducibility was achieved, as the initial 18 images were each measured twice. The images were randomly measured and no indication was given to the sonographers that any of the images were in fact duplicated. No measuring instructions were given to sonographers in regard to fetal variables, as it was important to determine whether correct measuring procedures, as suggested by ASUM, were routinely followed in clinical practice. Assessment of calliper placement was by viewing the recorded images. Sonographers were not given the option to refuse to measure the suboptimal images. 3.4 Results The 26 sonographers from MIA practices in NSW who participated in the study had scanning experience ranging from 6 months to 21 years with a mean of 8.9 years. Five of the more senior sonographers no longer routinely perform obstetric scans and at their own admission said they were out of practice in correct calliper placement. All 26 sonographers were disadvantaged as they did not physically perform the scans and this can make image edge perception difficult. The resultant measurements therefore, 115 particularly those from the images at awkward angles, had to be assessed with this perception problem noted. 3.4.1 BPD, OFD and Head Circumference Image 3/1: Head imaged at an acceptable angle Image 3/2: Head at difficult angle Table 3/1: Range of head measurements. Actual dates: 34wks – BPD 86 +/- 6mm(2SD), OFD 108+/- 5.5mm, HC 305 +/- 25mm. BPD range OFD range Image 3/1 Image 3/2 83 – 88mm (mean 84mm) 84 – 88mm (mean 86mm) 32.5 to 35 weeks 33 to 35 weeks 100 - 107mm (mean 97 104mm) 31 to 33 weeks HC range 294 – 319mm – 107mm (mean 102mm) 29 to 33 weeks (mean 295 – 328mm (mean 305mm) 32.5 to 36.5 weeks 305mm) 32.5 to 38 weeks 116 Image 3/1 represents an acceptable head image for measuring the biparietal diameter, occipito-frontal diameter and head circumference in the third trimester. Twenty-one sonographers measured the BPD at the widest section of the image and were within a 3mm range. The differences occurred with calliper placement from outer to inner and outer to outer parietal bones. The occipito-frontal diameter range was wider due to a poorly defined occipital bone and this also translated to the head circumference differences. The inter- sonographer variability for the head circumference on this image was 8.1%. Image 3/2 is a technically unacceptable image but was taken at an awkward angle to reflect the problems often occurring with third trimester measuring. Once again the OFD and HC range was due to perception of the occipital edge. All but one of the sonographers used the ellipse-measuring mode for the head circumference which means that the circumference didn’t always follow the outline of the skull, thus making a few millimetres difference. Comparing the measurements obtained from the optimum image (3/1) and the suboptimal image (3/2) with a one-tailed t-test showed no statistically significant difference. 117 3.4.2 Abdominal Circumference Image 3/3: Typical image Image 3/4: Spine anterior Table 3/2: Range of abdominal circumference measurements Actual dates Image 3/3 Image 3/4 34 weeks. AC 305mm 36 weeks. AC 317mm Abdominal circumference 295 range – 308mm (mean 314 301mm) 33 to 34.5 weeks – 338mm (mean 321mm) 35 to 37.5 weeks Image 3/3 abdominal circumference was performed well by all sonographers, even considering the ill defined posterior edge. The inter-sonographer variability for this image was 4.3%. Image 3/4, an often-typical 3rd trimester abdominal image, had poorly defined abdominal wall yet the AC measurements were within normal range for the gestation. Twenty-two of the 26 sonographers utilized the ellipse measuring facility for both images which can be a source of error due to the often irregular shape of the abdomen in late pregnancy, particularly when the cross section is non-elliptical. 118 3.4.3 Femur Length Image 3/5: Correct imaging plane Image 3/6: Acute angle – unacceptable. Table 3/3: Range of Femur Length Measurements Actual dates Image 3/5 Image 3/6 34 weeks FL 67mm 34 weeks +/- 5.5mm (2SD) Femur length range 66 – 71mm (mean 68mm) 66 – 76mm (mean 70mm) 34 to 36.5 weeks 34 to 40 weeks Image 3/5 represents the ideal long bone imaging plane. Twenty-three of the measurements were within a 2mm range. The higher figures were due to measurement of artefact. Image 3/6 was a technically unacceptable image plane for measuring long bones, which was reflected in the wide range of results. The majority of sonographers included the epiphysis and/or artefacts in their measurements. This fetal parameter in particular emphasises the importance of a correct imaging plane for accurate assessment of size. A long bone more than 15 degrees off the horizontal plane should not be used. 119 3.4.4 Fetal Weight Estimation The following Hadlock fetal weight formula incorporating the BPD, HC, AC and FL was used for this study. Log10 (EFW in grams) = 1.3596 – (0.00386 AC x FL) + (0.0064 HC) + (0.00061 BPD x AC) + (0.0424 AC) + (0.174 FL). Standard deviation (EFW) = +/- 7.5% of EFW (predicted mean). Table 3/4: Fetal Weight Variations Measurements used. Weight +/- standard deviation Lowest measurement 2212 grams 166 grams For each variable. (4lbs 14ozs) Highest measurement 2657 grams For each variable (5lbs 14ozs) Individual sonographer - 2243 grams 168 grams 2578 grams 190grams 199 grams Mean of each variable (lowest). Individual sonographer Mean of each variable (highest). The weight range seen in Table 3/4 highlights the problem of predicting fetal weight. Individual sonographers can vary slightly in their measuring techniques for each fetal variable, leading to a difference of over 300 grams in weight estimation. The most commonly used fetal weight formulas are those of Hadlock et al, using different combinations of fetal parameters. All of these formulas have a standard deviation of seven to ten percent. The sub-optimal images were not used in this analysis. 120 3.4.5 Intra-Sonographer Results Statistical analysis for this sub study was performed using SPSS for Windows Percentage Exact Agreement (PEA) and Percentage Close Agreement (PCA) 1mm & 3mm. For PEA, repeat measurements must be exactly the same to achieve 100%. PCA 1mm means that the repeat can be within 1mm of the first measurement and PCA 3mm within a 3mm range to achieve 100%. Intra-sonographer results were divided into 3 groups. Group (A) had less than 4 years experience and included the student sonographers, Group (B) had 4 to 10 years experience and Group (C) with greater than 10 years experience. These groups were further divided into the best and worst results, which helped distinguish those sonographers without much obstetric experience. Only this later group are represented in the table below. Table 3/5: Intra-Sonographer Results Group (number) Years Experience Percentage A. < 4years (6) B. 4 – 10years (11) C. > 10years (9) Best Worst Best Worst Best Worst 6mths 3yrs 6yrs 7yrs 12yrs 15yrs 16.7% 50% 16.7% 41.7% 16.7% 91.7% 25% 66.7% 41.7% 66.7% 33.3% 91.7% 58.3% 75% 66.7% 75% 41.7% Exact 66.7% Agreement Percentage Close Agreement (1mm) Percentage Close Agreement (3mm) 121 3.5 Discussion In this study, with few exceptions, sonographers measured the fetal variables in an acceptable way. The only variables where some of the 52 measurements were not within the accepted range of two standard deviations were the OFD in both image 3/1and 3/2 and the femur at the acute angle in image 3/6. Although the OFD on its own is not utilised in any fetal weight formula it is important in the third trimester when head shape can change due to moulding thus affecting the BPD and consequently the estimated fetal weight. The OFD measurement is used in the calculation of the cephalic index (CI = (BPD/OFD)x100%) and the BPD should only be used in a fetal weight formula if the CI is within the normal range. The abdominal circumference grows by approximately 10mm a week and so any measuring error can place an IUGR fetus at risk of non-detection. Dudley and Chapman (2002) found in their study that 53% of abdominal circumference errors were 5mm or greater and 16% greater than 10mm, or a one-week error. Gull et al (2002) also found the abdominal circumference to have the largest variation. This type of clinical error, over or under measuring, could impact on clinical management decisions for intra-uterine growth restriction (IUGR) or the macrosomic fetus and was also one of the components of the study by Mongelli et al (1998) when they contrived a mathematical model of the effect of time interval and ultrasound error when screening for IUGR. 122 Inter/intra observer variability was an important component of the works of the prominent sonologists Hadlock and Deter. Using the optimum head and abdominal images (images 3/1, 3/3) and the measurements of all 26 sonographers, this study had an inter-sonographer error of 8.1% for the head circumference and 4.3% for the abdominal circumference compared with Hadlock’s study, with only two operators, of 1.2% for the head circumference and 2.4% for the abdominal circumference. Measuring suboptimal images may be a factor in inter-observer variability, as could the averaging of measurements taken from both optimal and suboptimal images. The range of results for the individual fetal variables, using the optimal images 3/1, 3/3 and 3/5, made a 445gram or 17% difference in the fetal weight estimation. Using the individual sonographers mean set of variables on these same images the difference was 335 grams or 12%. The intra-observer error with 26 sonographers was 83gms, which compared favorably with the study of Chang who concluded that ultrasound for fetal weight assessment was reproducible with an intra-observer difference of less than 75gms. Gull et al (2002) assessed the inter and intra- sonographer contribution to discrepancies in fetal weight estimation. Using only three sonographers the BPD, HC, AC and femur length were measured in 39 fetuses at term and the resultant individual measurements and weight estimations were compared with the abdominal circumference showing the largest discrepancy. There was a difference of 5.8% in estimated fetal weight between the three sonographers. One of the aims was to detect any common pitfalls of measuring that could affect the report on fetal size. The most common problem was on images that were not 123 standard measuring planes due to angulation. The best example was the long bones, where both experienced and inexperienced sonographers measured the diaphysis, epiphysis and/or artefact. This may have been due to the fact that the sonographers did not personally perform the scans and so end point/edge perception was difficult to evaluate. In the third trimester it is not always possible to capture the recommended image plane for measuring a fetal variable. In this instance it may be necessary to accept a sub-optimal image for measuring. Experience with obstetric measurements was reflected in the final analysis, with incorrect calliper placement more obvious by those sonographers who did not routinely perform obstetric scans. Five of the sonographers involved in the study either did not routinely perform third trimester scans, or had limited obstetric ultrasound exposure. It was important to include this group of sonographers as they were qualified to perform such examinations, regardless of how often they actually scanned pregnancies. This lack of obstetric scanning experience was reflected in their measurements of both the acceptable and sub-optimal images, with calliper placements less accurate than those sonographers with more obstetric exposure. Three of these sonographers were the worst in their respective group for intra-sonographer evaluation. Years of experience made no difference to the accuracy of the measurements, with the best result obtained by a student with six months of clinical practice and the worst by a fifteen-year veteran. All of the student sonographers involved in the study were very precise with calliper placement, which may reflect the constant supervision and reinforcement of correct measuring procedure and practice in implementing what they have been taught during the obstetric 124 component of their ultrasound course. More veteran sonographers may become complacent with measuring procedures. The more accurate and reproducible measurements were achieved when the recommended imaging planes were used as in images 3/1, 3/3 and 3/5. Although the difference in using ellipse and tracing method for the head and abdominal circumference was not statistically significant in this study, Chitty et al (1994) believed that a difference of 3.5% in the two methods justify separate charts. Dudley and Chapman’s 2002 study showed a difference of 1.3% and concluded that this may have been due to the improvement in measuring facilities on the newer ultrasound machines. One of the statistical reviewers for this article was critical of the simplistic approach to the statistical analysis. When the paper was resubmitted it was thought appropriate to explain why a more complicated approach was not taken. For the purpose of this study, adjustment for correlations was not necessary and so a principal components analysis to correlate the various measures was not performed. The aim was to establish the agreement between sonographers, for each of the measures separately, as these are the measures routinely taken by sonographers. Reducing the various measures to a principal component would not shed light on the sonographers' agreement on any one of them. 125 3.6 Quality Control in the Third Trimester Quality control in obstetric ultrasound is essential if clinically significant errors are to be avoided. Obstetric ultrasound will always be limited by maternal body habitus, position of the fetus, liquor volume, gestational age, the physical principles of ultrasound and the time constraints of scanning. Equipment maintenance, with particular reference to calliper calibration, is an important aspect of quality control. By implementing ongoing sonographer training, adherence to scanning protocols and audits for imaging planes and measurement accuracy, improvements can be made in fetal growth assessment. The failure to meet quality criteria results in errors. In Australia ASUM has attempted to standardise ultrasonic fetal assessment of size/growth by recommending scanning protocols, the use of particular measuring planes and fetal measurement charts for reporting. It is hoped that sonographers and sonologists adopt this policy so that all practices are taking measurements in a similar way and as a result pregnant women can confidently move inter-practice throughout Australia for ultrasonic examinations without jeopardising the report on fetal size. 126