Template letter to Primary Care from Specialist following initiation of
advertisement
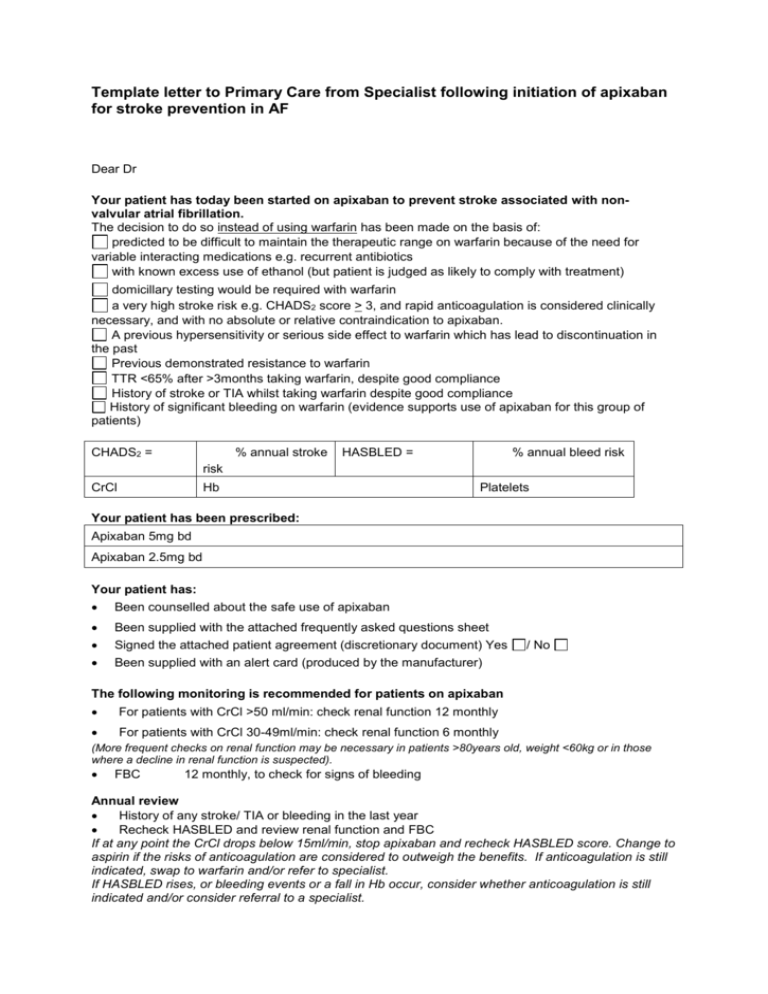
Template letter to Primary Care from Specialist following initiation of apixaban for stroke prevention in AF Dear Dr Your patient has today been started on apixaban to prevent stroke associated with nonvalvular atrial fibrillation. The decision to do so instead of using warfarin has been made on the basis of: predicted to be difficult to maintain the therapeutic range on warfarin because of the need for variable interacting medications e.g. recurrent antibiotics with known excess use of ethanol (but patient is judged as likely to comply with treatment) domicillary testing would be required with warfarin a very high stroke risk e.g. CHADS2 score > 3, and rapid anticoagulation is considered clinically necessary, and with no absolute or relative contraindication to apixaban. A previous hypersensitivity or serious side effect to warfarin which has lead to discontinuation in the past Previous demonstrated resistance to warfarin TTR <65% after >3months taking warfarin, despite good compliance History of stroke or TIA whilst taking warfarin despite good compliance History of significant bleeding on warfarin (evidence supports use of apixaban for this group of patients) CHADS2 = % annual stroke HASBLED = % annual bleed risk risk CrCl Hb Platelets Your patient has been prescribed: Apixaban 5mg bd Apixaban 2.5mg bd Your patient has: Been counselled about the safe use of apixaban Been supplied with the attached frequently asked questions sheet Signed the attached patient agreement (discretionary document) Yes Been supplied with an alert card (produced by the manufacturer) / No The following monitoring is recommended for patients on apixaban For patients with CrCl >50 ml/min: check renal function 12 monthly For patients with CrCl 30-49ml/min: check renal function 6 monthly (More frequent checks on renal function may be necessary in patients >80years old, weight <60kg or in those where a decline in renal function is suspected). FBC 12 monthly, to check for signs of bleeding Annual review History of any stroke/ TIA or bleeding in the last year Recheck HASBLED and review renal function and FBC If at any point the CrCl drops below 15ml/min, stop apixaban and recheck HASBLED score. Change to aspirin if the risks of anticoagulation are considered to outweigh the benefits. If anticoagulation is still indicated, swap to warfarin and/or refer to specialist. If HASBLED rises, or bleeding events or a fall in Hb occur, consider whether anticoagulation is still indicated and/or consider referral to a specialist. APIXABAN KEY POINTS for clinicians It does not require blood tests to monitor anticoagulant effect (INR monitoring) Regular blood tests are needed to monitor kidney function and look for signs of bleeding It must be stopped if kidney function declines so that the CrCl <15ml/min In patients with severe liver disease associated with clotting problems and clinically significant bleeding risk, including those with cirrhosis, apixaban should not be prescribed Apixaban levels drop by half in approximately 12 hours. Taking the tablets on a regular basis is therefore very important, and protection from stroke will be lost if only one dose is missed (the effect of warfarin lasts longer). In the event of surgery or procedures, apixaban should be stopped 24-48 hours prior to the intervention depending on the bleeding risk of the procedure. See product SPC for details: http://www.medicines.org.uk/EMC/medicine/27220/SPC/Eliquis+5+mg+filmcoated+tablets/ Apixaban should not be used with the following drugs because of interactions: Ketoconazole, itraconazole, voriconazole and posaconazole and HIV protease inhibitors (e.g., ritonavir). Caution recommended for concomitant use with strong CYP3A4 rifampicin, phenytoin, carbamazepine, phenobarbital or St. John's Wort). Apixaban prolongs clotting tests such as prothrombin time (PT), INR and activated partial thromboplastin time (aPTT) but these are not a measure of degree of anticoagulation There is no established method to reverse the effect of apixaban. In the event of suspected overdose, activated charcoal should be administered within 2 hours of ingestion. For further information or advice please contact , the local Trust contact who will be able to answer any further questions you may have. Signature of specialist