Surgery in Africa8

Gynecologic Emergencies
1.0 Introduction
2.0 Abnormal Pregnancy
2.1 Forms of abortion
2.11 Spontaneous Abortion
2.12 Threatened Abortion
2.13 Inevitable and incomplete abortion
2.14 Septic abortion
2.2 Gestational Trophoblastic Disease
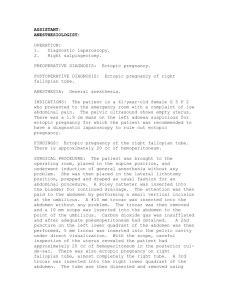
2.3 Ectopic Pregnancy
3.0 Infectious Gynecologic Diseases
3.1 Bartholin’s Gland Abscess
3.2 Pelvic Inflammatory Disease
3.3 Toxic Shock
3.4 Necrotizing Fasciitis
4.0 Ovarian Cysts
4.1 Torsion
4.2 Hemorrhagic ovarian cyst
4.2 Rupture
5.0 Trauma
5.1 Vulvar Hematoma
5.2 Sexual Assault
6.0 Recommendations
7.0 Conclusions
8.0 Clinical Questions
1.0 Introduction
General surgeons in the developing world have to be versatile in diagnosing and managing abdominal disorders, not just involving the GI tract, but also those of other organ systems such as the genitourinary tract. It has been estimated that 30% or more of emergency abdominal operations in Africa are for obstetric or gynecologic conditions
[71]. Common gynecologic emergencies can mimic general surgical conditions such as cholecystitis and appendicitis. Most patients with gynecologic emergencies complain of pelvic pain and/or abnormal vaginal bleeding. A complete history and physical exam will define the extent of the laboratory and radiologic work up and the expediency of resuscitation. Most gynecologic emergencies arise from benign rather than malignant etiologies.
2.0 Abnormal Pregnancies
2.1 Forms of abortion
2.11 Spontaneous abortion
Approximately 20% of known human pregnancies terminate in a recognized abortion [1].
Eighty percent of spontaneous abortions occur in the first trimester and are usually a result of chromosomal or genetic abnormalities. The risk factors for a spontaneous loss
include prior pregnancy loss (history of one abortion (13%); two prior abortions (25%); three prior abortions (45%) and 4 prior abortions (54%)) and rising maternal age (women
35-40 yr (21%); women over 40 yr (42%)).
2.12 Threatened abortion
These women present less than 20 weeks’ gestation with crampy abdominopelvic pain, vaginal spotting, no cervical dilation or effacement and an intact intrauterine pregnancy.
The management includes restricting activities. There is no evidence that progesterone or injectable HCG will improve outcome. Serial bHCG and ultrasonography will aid in predicting outcome [64].
2.13. Inevitable and incomplete abortion
Those women with an inevitable abortion present with an open cervical os on pelvic examination but without a history of passing tissue [64]. The women with an incomplete abortion have evidence of retained products either by examination or ultrasound. These cases usually occur between 8 and 14 weeks of pregnancy are incomplete and require surgical evacuation. If the woman’s vital signs are stable, then treatment includes: CBC, group and screen and possibly cross match, insertion of a large bore IV, oxytocin (10-30 units in 1000ml of 5% Ringers lactate) , analgesia, and a paracervical block with 1% lidocaine (10cc).The goal is to evacuate the uterine contents with suction (vacuum aspiration) [69]. Intercourse should be avoided for 2 weeks. Iron supplementation should be considered. If the mother is Rh negative and father Rh positive, give 50 microgram of anti-D gamma globulin IM.
2.14 Septic Abortion
There is an extensive literature on complications related to abortions in Africa. The
World Health Organization estimates that the death rate from unsafe abortions in Africa is 110/100,000 live births, the highest in the world. In Mozambique, 22% of maternal deaths were in adolescents and septic abortion was one of the 4 leading causes [36]. In
Nigeria, unsafe abortions account for 40% of maternal deaths [38]. In Kenya, the annual number of women with abortion complications admitted to public hospitals is 20,893, with a case fatality rate of 0.87% (95% CI 0.71-1.02%) [37]. In the Central Republic of
Africa, abortions accounted for 13.6% of gynecologic admissions, 43.4% of which were from complications of self inflicted abortions (SIA). This later type of abortion is more common in students and the main reason is the financial inability to maintain the pregnancy and child. The common methods for SIA are drug combinations (39.1%) and mechanical tools (26%). Severe complications including infection and death seem to be confined to this group [39].
When a patient presents to emergency, a history and subsequent physical exam is important. The investigations will include CBC, urinalysis, electrolytes and renal function tests, Gram stain of vaginal discharge, blood cultures, CXR and PTT/INR. An ultrasound will define retained products of conception.
The management begins with combination IV antibiotics (including gram positive, gram negative and anaerobic coverage) and evacuation of the uterus. If there are signs of septic shock, then CVP will guide the fluid resuscitation, (administer IV fluid according to CVP of > 4 and < 12). Also important are placing a foley catheter, nasal oxygen, oxytocin or ergot as required to cause the uterus to contract (may effect the blood pressure). If sepsis persists despite these initial maneuvers or if there is evidence of
visceral perforation (ie. bowel) as a result of the abortion, a laparotomy may be required to repair the involved organ or remove the source of infection (hysterectomy).
A case control study from 4895 post abortion records in Zimbabwe showed that complete uterine evacuation and use of oxytocin are very important. Associated complications such as anaemia and sepsis were related to mortality. They recommended improved education of health care workers, in-service training, regular audits and changes in policies for managing abortions [33]. In Ghana the government has responded to high rates of complications from abortions by providing training to community-based midwives especially in the technique of manual vacuum aspiration [35]. A group from the Central Republic of Africa stressed the importance of making contraceptive methods more available in schools and universities [39]. In Kampala, Uganda, a qualitative study was completed with 30 women who had a near death experience. Four of these women had a septic abortion. The themes included powerlessness to get help both within and outside of the hospital. Financial barriers and transport problems were pre-eminent. Other issues included overcrowding, long delays, shortages and inhumane care. Interestingly, bribery was not reported as an issue [34].
2.2 Gestational trophoblastic disease (GTD)
Molar pregnancies occur in 1 out of 1000 pregnancies [64]. They are usually associated with abnormal chromosomal complement of the fetus. In a complete mole, there are only paternal chromosomes present (usually 46XX , occasionally 46XY). In a partial mole, triploidy is common (ie., XXX, XXY). The Mandela School of Medicine,
Durban [32] studied the referral pattern of 98 women with GTD over a 5-year period.
There was no trend of referral of patients from specific geographic areas.
Women with GTD present with a history of amenorrhea, hyperemesis, vaginal spotting, and possibly passing grape like tissue. On physical exam there may be tachycardia. This results from the elevated
HCG. The common portion of the
HCG and TSH molecule results in the body reacting to the elevated
HCG as if TSH were elevated. One can also see tremors, elevated blood pressure, respiratory distress (as a result of trophoblastic embolization, congestive heart failure secondary to anemia, hyperthyroidism, preeclampsia or fluid overload need to be ruled out) and blood in the vagina. Uterine size is enlarged for dates in 50% of cases, and/or palpable ovarian mass from theca lutein cysts may be present. Investigations include CBC, PTT, INR, Blood type, antibody screen and cross match, serum
HCG, and CXR. An ultrasound shows a snowstorm pattern. You may consider sending renal, liver and thyroid function tests.
Treatment begins with starting an IV. If the woman is hypertensive it is important to stabilize the blood pressure. If she shows evidence of hyperthyroidism, use
blockers to prevent thyroid storm and the associated delirium, convulsions, atrial fibrillation and cardiac collapse. Evacuate the uterus in the operating room using suction D+C. Start oxytocin (10u per 1000 cc NS) once dilatation is completed. Rhogam should be given if mother is Rh negative and a form of reliable contraception started. Serial weekly
HCG should be taken until normal then q2-4weeks for 6 months. If
HCG plateaus over 3 weekly values or rises refer for treatment with chemotherapy (ie. methotrexate or actinomycin D)
2.3 Ectopic Pregnancy
Any pregnancy not in the uterus is considered ectopic. Ninety-five percent of ectopic pregnancies are tubal, less commonly on the ovary or the peritoneum. Population based
incidence of ectopic pregnancy in Cameroon was 0.79% (95% CI 0.72%-0.88%) with a mortality rate of 0.94% (95% CI 0.32%-2.72%) [45]. A twenty year review of the African literature showed that the ectopic pregnancy case fatality rate is 1-3% [52], which is more than 10 times higher than that reported in industrialized countries. Late diagnosis leading to major complications and the necessity of emergency surgical treatment are the key causes [49]. Morbidity rates are high, usually due to post-operative infection [52]. A case report of ectopic pregnancies in Ile-Ife Nigeria showed that the incidence was 10.5 per
1000 live births. In 10% of cases, the initial diagnosis was wrong and this led to 5/38 deaths. This death rate was very much higher than the rate among those correctly diagnosed (2/342) [50].
We will specifically discuss tubal pregnancies. These pregnancies account for
1.3-2% of all pregnancies. Mortality rates from ectopic pregnancy fell from 35.5 to 3.8 per 10,000 from 1970 to 1986 in the USA. The women at risk are all those of childbearing age with abdominal pain or abnormal vaginal bleeding, even those over 40 years, tubal ligation [2] or on oral contraception. A case-control study in Lagos, Nigeria showed that the risk factors for ectopic pregnancy were early age of sexual debut (OR
1.93, 95%CI 1.71-2.93), multiple lifetime sexual partners, induced abortions, PID
[44,51], STD, miscarriage [44,51], prior induced abortions [51], pelvic surgery, IUD (OR
3.76, 95% CI 2.12-6.69) [44,48]. A case series completed at the Nigeria Teaching
Hospital in Enugu, showed that ectopic pregnancy was most common in young single women who had previously undergone an induced abortion with resultant pelvic infection
[41]. Other risk factors include: prior ectopic pregnancy, infertility, prior pelvic inflammatory disease (PID) or sexually transmitted disease (STD), intrauterine devise
(IUD), past or present smoker, documented tubal pathology, or multiple sexual partners.
Only one third of patients are diagnosed on initial evaluation [2, 62]. Any woman with pelvic pain and vaginal bleeding should be screened with serum or urine human chorionic growth factor (
HCG).
The woman may have no symptoms [2]. If symptoms are present they may include abnormal vaginal bleeding (in 50-80% of patients) [2,51], abdominal pain (in 90-
100% of patients) [2,51], shoulder tip pain (which reflects blood in the peritoneal cavity), and amenorrhea [51].
On exam, an adnexal mass is present in only one-third of patients [2]. The presence of peritoneal signs, cervical motion tenderness and lateral or bilateral abdominal or pelvic tenderness increases the likelihood of an ectopic pregnancy [62]. Hypotension strongly suggests a ruptured ectopic [2, 51]. In Benin City, Nigeria, 49.3% of women with ectopic pregnancy were in shock at the time of diagnosis [51].Tachycardia unfortunately is only seen in half of the patients. In the other 50% of patients with hypotension and a normal heart rate [2], the hematoperitoneum has triggered a parasympathetic response preventing increase in the heart rate despite significant volume loss. The Nigerian group showed that the frequency of ectopic pregnancy was 2.32% of all pregnancies. They used culdocentesis to make the diagnosis in 80% of cases [40]. In
Dakar, Senegal, mini-pfannenstiel laparotomy under local anaesthesia was the management approach in view of difficulties with laparoscopy in their unit [47].
Investigations
HCG : this serum lab value will increase by 66% every 48 hours in normal intrauterine pregnancy. If the value does not rise appropriately, the patient may have either an ectopic pregnancy or a failing intrauterine pregnancy.
Pelvic Ultrasound : An intrauterine pregnancy is confirmed by a gestational sac, fetal pole or a fetal heart beat within the uterus. An ectopic pregnancy is confirmed by evidence of an adnexal mass with extrauterine fetal heart beat. The intrauterine findings are only visible on transabdominal ultrasound when the
HCG is above 6000 mIU/mL and on transvaginal ultrasound when the
HCG is above 2000 mIU/mL. When the
HCG is below these levels, ultrasound may not be reliable. In Botswana, the addition of ultrasound improved case management. The service was felt to be affordable for the health care system [55].
Decision for Surgery
Watch and wait: When hemodynamically stable, one may watch the patient either at home or in the hospital with serial
HCG.
Surgery is preferred : when the
HCG > 5000 mIU/mL, or there is positive cardiac activity on ultrasound, or the mass is greater than 4 cm, or the patient is unstable or there is free fluid in the cul de sac. In Benin City, Nigeria [51], 80.3% had ruptured tubal pregnancy at diagnosis; in Senegal, 95% had ruptured [52].
Some of the advantages of a surgical approach are: confirming the diagnosis of ectopic pregnancy, effective and prompt treatment, and visual inspection of the pelvis and both fallopian tubes. Laparoscopy has replaced laparotomy for routine management of ectopic pregnancy in many centers. A review of 3 randomized controlled trials showed that salpingostomy by laparotomy has an increased rate of elimination of the pregnancy compared to laparoscopic technique. However, the 2006 Cochrane review recommends laparoscopic salpingostomy even though there is a slightly higher rate of persistent trophoblast rate (RR 3.6, 95%CI 0.63-21)[68]. There was no difference in tubal patency, rates of subsequent intrauterine pregnancy or ectopic. Operative blood loss was higher in open cases and laparoscopy is cheaper. Salpingostomy should be considered instead of salpingectomy when the contralateral tube is diseased. Due to the risk of persistent ectopic tissue with salpingostomy,
HCGs need to be followed. Persistent elevations in
HCGs can be managed by an ultrasound to rule out another site for pregnancy and if confirmed that there is no intrauterine pregnancy, methotrexate in the stable patient or repeat surgery in those that have failed medical management. Salpingectomy is the treatment of choice in Africa, occurring in 89.5% of cases [51] – 100% [52,53].
Autotransfusion is an option and occurs at rates of 54.6% of cases in Nigeria [51,54].
Medical Management of Ectopics
Methotrexate has been used for many years in the management of gestational trophoblastic disease. It interferes with DNA synthesis causing destruction of trophoblastic activity. It inhibits dihydrofolate reductase and therefore the synthesis of thymine and purine. Stoval [1,4,5] has reported on 100 outpatients treated with methotrexate for an unruptured ectopic 3.5 cm or less in size. The regimen was alternate day methotrexate until the serum
HCG decreased by greater than 15% over 2 consecutive days. 96 patients were successfully treated and 4 required surgery for ruptured ectopics. Tubal patency was present by hysterosalpingogram in 84.5% of the cases. Stoval has also reported using a single dose of methotrexate (50 mg/m2 IM) in 120
patients with 7 requiring surgery and 82.3% tubal patency. No side effects from the medication were noted. 60% of patients treated this way will develop pain. If the patient is seen for increased abdominal pain, an ultrasound and Hct should be done. Patient can be observed if there is no large accumulation of blood in the cul de sac. Success rates of medical management were at 92% with a
HCG less than 5000 IU/L and 98% with
HCG less than 1000 IU/L. Multiple doses appear to be superior [5]. Repeat ectopics are seen in 10% of cases.
3.0 Infectious Gynecologic Diseases
3.1. Bartholin’s Gland Infection
The Bartholin’s glands are located at the 4 and 8 o’clock position of the entrance to the vagina. About 2% of women develop enlarged Bartholin’s glands [1]. This is due to cystic dilation of the duct with obstruction and resultant adenitis or abscess. Usually the infection is a polymicrobial, necrotizing, subcutaneous infection. Bartholin’s gland infections usually occur during the reproductive years [63].
The symptoms include acute vulvar pain that develops rapidly over 2-4 days, dyspareunia, and pain during walking or movement. The signs include vulvar erythema, acute tenderness, edema and cellulitis of the surrounding tissue. For a symptomatic abscess, this is treated by creating a marsupialized tract by removing an elliptical wedge of skin over the abscess and suturing the edges of the abscess to the skin. An alternative treatment is to place a Word catheter through a stab incision into the abscess. The balloon tip is inflated to break up all the loculations and left it in place for 4-6 weeks [63]. This allows epithelialization of the tract. Antibiotics are not necessary unless there is surrounding cellulitis. If the abscess recurs, or presents in a woman over 40 years, excision of the gland or biopsy of the gland is important to rule out an adenocarcinoma of the Bartholin’s gland.
3.2. Pelvic Inflammatory Disease (PID)
Pelvic inflammation is usually caused by an ascending infection to the upper genital tract not associated with pregnancy or intraperitoneal pelvic operations. This inflammation may include infections of the endometrium (endometritis), oviducts
(salpingitis), ovary (oophoritis), uterine wall (myometritis), uterine serosa and broad ligaments (parametritis) and pelvic peritoneum. The most important sequela of PID is the destruction of the tubal architecture [1].
The most important issue with PID is prevention. Primary prevention includes education of the cause of PID and use of condoms and chemical barrier methods.
Secondary prevention involves screening women at high risk for chlamydia and gonorrhea, screening for acute cervicitis, treating sexual partners and education to prevent recurrent infection. PID is rarely seen in women who are not menstruating
(prepubertal, pregnant or postmenopausal women). When an infection is seen in a postmenopausal woman one should consider genital malignancies, diabetes, concurrent intestinal disease.
Pelvic inflammatory disease is usually a polymicrobial infection with aerobic and anaerobic bacteria. N. gonnorhoeae and C. trachomatis cause acute PID in the majority of cases. These are usually cultured in the first 48hrs of the disease. Later, anaerobic bacteria tend to be seen.
Risk factors
PID is seen in menstruating young women. 75% of cases occur in women less than 25yr of age. The risk of PID in a sexually active adolescent is 1 in 8 versus 1 in 80 for women over 25 yr [1]. Exposure to multiple sexual partners increases the risk of PID by 5 times [1]. Living in an area of high prevalence of sexually transmitted diseases increases the risk of acquiring PID. Known cervical colonization with C. trachomatis increases the PID risk.
Douching increases the risk of PID by 3-4 [1]. Intrauterine device is associated with an increased risk especially during the first 3 weeks from the time of insertion. Risk of PID is 9.7 per 1000 women-years in the first 20 days after insertion versus 1.4 per
1000 women-years during the next 8 years [1]. Prior episode of PID is associated with a subsequent risk of PID. 25% of women with one episode of PID will develop another episode [3]. This may be related to microscopic tube damage or an untreated male partner. 1 in 200 cases of therapeutic abortion will develop PID. A history of recent instrumentation is associated with PID.
Methods for minimizing or preventing PID include monogamy, low number of partners (decreases likelihood of exposure to the causative agent), barrier methods
(condoms, diaphragms, spermicidal preparations (ie., nonoxynol 9)), oral contraceptives
(the progesterone in the OBCP thickens the cervical mucus which inhibits sperm and bacterial penetration and decreases menstrual flow which shortens the interval for bacterial colonization), vaccine for Hepatitis B, and tubal ligation.
Symptoms of PID may be nonspecific. The timing is usually after menstruation.
Other symptoms include fever (34.4%), dull and constant lower abdominal pain (may be made worse with sexual activity (99.3%)),vaginal discharge (69.3%), irregular bleeding
(40%), urinary symptoms (19.8%), and vomiting (10.4%).
Pain is usually bilateral in 90% of women distinguishing PID from appendicitis, diverticulitis or postsurgical abscess [1]. Temperature is over 38
C. The abdominal/pelvic exam shows direct tenderness with or without rebound (95.4%); tenderness with motion of cervix and uterus and adnexal mass or tenderness (47.8%).
Purulent cervical discharge is present in 75% cases.
Investigations should include:
Culture the endocervix : looking for C. Trachomatis and N. gonorrhoeae.
WBC >10,000 (50%)
Elevated Erythrocyte Sedimentation Rate : greater than 15 mm per hr (75%)
Elevated C-reactive protein
Endometrial Biopsy : looking for endometritis with 5 or more neutrophils per 400 high- power field and 1 or more plasma cell in the stroma. (Usually only used in research protocols as it takes 48 hours to get a result).
Purulent material (WBC) from peritoneal cavity by culdocentesis or laparoscopy
Ultrasound: Early stages – no findings. Later stages – endometrial thickening with or without endometrial fluid and gas, ovarian enlargement with indistinct ovarian borders, uterine enlargement with indistinct uterine contours, free intraperitoneal fluid [4,6, 65].
Ascending extrauterine disease may cause tuboovarian complexes with dilated inflamed fallopian tubes and enlarged inflamed ovaries or frank tuboovarian abscess (10%).
Laparoscopy: Several conditions (ie. appendicitis) may mimic PID and laparoscopy will allow inspection of the tubes, collection of culture material and better define the situation.
However, laparoscopy is an expensive invasive technique and many women do not undergo this assessment. Indications for laparoscopy include: impending septic shock, acute surgical abdomen, complicated differential diagnosis in a postmenopausal woman.
At the time of scope, there is the opportunity to lyse adhesions, irrigate the pelvic cavity and drain the abscess. The classic findings for PID include: the pelvic organs appear red, indurated, edematous oviducts, pockets of purulent material, large pyosalpinx, tuboovarian abscess. Useful, especially if the patient is not responding to treatment
Culture the urethral secretions from the male partner: frequently an overlooked investigation
Management
Goals:
1.
Resolution of symptoms and
2.
Preservation of tubal function.
Early treatment (ie. within 3 days of symptoms) will minimize occurrence of tubal infertility or ectopic pregnancy. PID is usually a polymicrobial so treatment should cover N. gonorrhoeae, C. trachomatis, anaerobic rods and cocci (i.e, bacteroides, peptococcus, peptostreptococcus, clostridium, actinomyces species), gram-negative aerobic rods and gram-positive aerobes (ie., streptoccous, staphylococcus, haemophilus,
E. coli).
CDC guidelines for diagnosis [7,8,9,63]
Major Criteria (need all three)
Lower abdominal tenderness
Bilateral adnexal tenderness
Minor Criteria (need one)
Oral Temperature > 38.3 C
Mucopurulent cervical or vaginal discharge
Cervical motion tenderness Elevated ESR
Elevated C-reactive protein
Positive swab
CDC recommendations for treatment[7,8,9,63]
Outpatient:
Ofloxacin 400mg PO q12hr + Metronidazole 500mg PO q12h both for 14 days or
Cefoxitin 2gm IM + Probenecid 1 g PO + Doxycycline 100mg PO q12h for 14 days or
Ceftriaxone 250mg IM + Doxycycline 100mg PO q12hr for 14 days or
Ofloxacin 400mg PO q12hr + Clindamycin 450mg PO qid both for 14 days
Re-examine the patient within 3 days to ensure that she is improving. Reculture the cervix 4-6 weeks after treatment to ensure microbiologic cure.
Inpatient;
If a patient is not improving with oral antibiotics she should be hospitalized. Indications for hospitalization and use of intravenous antibiotics to get maximum levels of antibiotics include an adolescent with her first episode of PID, adnexal mass, associated pregnancy, immunodeficiency (especially with HIV and low CD 4 counts), when the diagnosis is in question (differential includes appendicitis, ectopic, cholecystitis if there is acute right upper quadrant tenderness). PID with an IUD in place or after instrumentation is usually from anaerobic bacteria. IUD should be removed and patient treated in hospital.
CDC recommendations for antibiotics for the in hospital patient are [5, 61]:
Regimen A : Doxocycline 100 mg IV or PO q12hr plus cefotetan 2 gm IV q12hr or cefoxitin 2g IV q6hr. May discontinue parenteral therapy 24 hr after improvement and complete a total of 14 days of doxycycline.
Regimen B : Clindamycin 900mg IV q8hr plus gentamicin load with 2gm/kg followed by a maintenace dose of 1.5 mg/kg q8hr. (May use single day dosing of gentamycin)
Alternate regimens : 1. Ofloxcin 400mg IV q12hr plus metronidazole 500mg IV q8hr or ampicillin/subactam 3g IV q6hr plus doxycycline 100mg IV/orally q12hr.
2. Ciprofloxacin 200mg IV q12h plus doxocycline 100kg IV/PO q12hr plus metronidazole 500mg IV q8hr.
There are a series of articles from several African countries including Ghana,
Addis Ababa, Gambia and Morocco. They all indicate the importance of following algorithms for determining treatment, and the problem of availability of high cost antibiotics [57, 58, 59, 60].
Surgery
An operation is indicated if there is life-threatening infection, ruptured tuboovarian abscess, pelvic abscess, persistent mass in an older woman where childbearing is not a concern, or a persistent symptomatic mass.
Percutaneous drainage of an abscess under ultrasonic or computer tomography guidance is an option which shows favorable short terms outcomes in the order of 90% [1]. When the abscess is 4-6 cm 15% will need drainage. If the abscess is greater than 10cm, 70% will need drainage. In this situation the induration may be of such a degree that you may only be able to culture the pus, biopsy the lesion and drain the abscess.
Complications of PID:
Disseminated peritonitis can be complicated by serositis of adjacent bowel, peritoneal adhesions and small-bowel obstruction or perihepatitis (Fitz-Hugh-Curtis syndrome 5-10%) [3]. With Fitz-Hugh-Curtis syndrome there can be right upper quadrant tenderness or pleuritic pain with radiation to the shoulder or into the back. Liver transaminases may be elevated [61].
Tubo-ovarian complex, abscess and pyosalpinx can occur. Rarely is gonorrhoeae or chlamydia isolated from the abscess. Usually peptostreptococcus, bacteroides or
E.Coli are isolated [61]. HIV positivity is more common in Africa than in other regions.
Research done with patients who have HIV-1-seropositivity and acute salpingitis show that tubo-ovarian abscesses are more common (OR 2.8 95%CI 1.2-6.5) and this finding is related to the CD4 count (ie. the lower the count, less than 14, the higher the rate of
TOA). Treatment needs to include treatment of the PID and the HIV [56]. The abscess may rupture in 15% of cases causing a surgical emergency [63].
Long term sequelae include increased risk of infertility related to a tubal factor (10 fold more common if there is a history of PID), recurrent PID, chronic pelvic pain (in 20% of patients with PID) and ectopic pregnancy (7-10 fold more common in women with a history of PID).
3.3 Toxic Shock
Septic shock can be seen in the following gynecologic circumstances: medical abortion with misoprostol within one week of medication [12], post-delivery, surgical abortion, retained tampon and recent pelvic surgery. Severe septic shock has a mortality rate approaching 50% [10]. In Tunisia, septic shock syndrome was one of three poor prognosis factors for outcomes related to gram negative bacterial septicemia from 1996-
1998. In this hospital population, 18% of patients with gram negative sepsis died [27].
Sepsis is defined as the presence of an infection accompanied by evidence of systemic response. This systemic inflammatory response is defined as the presence of at least two of the following:
1.
Temperature greater than 38
C (96.8
F)
2.
Pulse greater than 90 beats/min
3.
Respiratory rate greater than 20 breaths/minute
4.
WBC greater than 12,000/mm
3
or less than 4,000/ mm
3
or greater than 10% immature band forms
Other findings can include [11]:
1.
General a.
Altered mental status b.
Significant edema or positive fluid balance (>20mL/kg in 24 hours) c.
Hyperglycemia (plasma glucose > 120 mg/dL or 7.7 mmol/L) in the absence of diabetes.
2.
Inflammatory variables a.
Plasma C-reactive protein >2SD above the normal value b.
Plasma procalcitonin > 2SD above the normal value
3.
Hemodynamic variables a.
Arterial hypotension (SBP<90 mm Hg, MAP <70 mmHg, or an SBP decrease > 40 mmHG in adults or >2SD below normal for age) b.
SvO
2
> 70% c.
Cardiac Index > 3.5 L/min/m
2
4.
Organ dysfunction variables a.
Arterial hypoxemia (PaO2/FIO
2
< 300) b.
Acute oliguria (urine output < 0.5 mL/kg/h for at least 2 h) c.
Creatinine increase > 0.5 mg/dL d.
Coagulation abnormalities (INR> 1.5 or a PTT>60s) e.
Ileus (absent bowel sounds) f.
Thrombocytopenia (platelet count <100,000/
L) g.
Hyperbilirubinemia (Plasma total bilirubin > 4mg/dL or 70 mmol/L)
5.
Tissue perfusion variables a.
Hyperlactamia (>2mmol/L) b.
Decreased capillary refill or mottling
Severe sepsis is the presence of sepsis and 1 or more organ dysfunction (i.e., acute lung injury, coagulation abnormalities, thrombocytopenia, altered mental status, renal liver or cardiac failure, or hypoperfusion with lactic acidosis. Septic shock is defined as the presence of sepsis and refractory hypotension. Bacteremia is the presence of viable bacteria in the blood and is only found in 50% of cases of severe sepsis and septic shock.
The initial reaction to infection is a neurohumoral, pro and anti-inflammatory response. The vascular endothelium is the site for the interaction of cellular activation (ie. monocytes and macrophages), host response (ie. cytokines) and activation of complement and the coagulation cascade. Diffuse endothelial disruption will result in organ dysfunction and tissue hypoxia.
The goal in septic shock is to delivery oxygen systemically through volume
(preload), blood pressure support (afterload) and optimizing stroke volume (contractility)
[10]. Management options include: continuous monitoring of vital signs, pulse oximetry and urine output; lab tests to identify infection type and organ system status; fluid resuscitation with NS to a CVP of 8-12 mm Hg; foley catheter; vasoactive agents to maintain mean arterial pressure of 65-90 mm Hg (Norepinephrine, Dopamine,
Phenylephrine, vasopressin, epinephrine, nitroglycerine); blood transfusion to Hct>21%; inotropes (dobutamine); intubation, sedation and paralysis to achieve a ScvO
2
>70%. Use low tidal volume to maintain end-inspiratory plateau pressure less than 30 cm H
2
O; antibiotics for an abdominal or pelvic source such as Piperacillin/tazobactam 3.375g q6h and gentamicin 5mg/kg q24h; use radiologic techniques to help locate the source; if patient not responding to rescuscitation consider Hydrocortisone 50mgIV q6h and
9
-fludrocortisone 50
g orally once a day for 7 days as 20% of patients have adrenal insufficiency and randomized trials show decreased rates of mortality [10].
3.4 Necrotizing Fasciitis
There is a high mortality rate with this condition, 20% if the operation happens within 24hr and 75% if the operation is delayed 48hr or longer [13-23].
Some of the situations where this is seen include penetrating trauma, paracentesis and laparoscopic or open abdominal or vaginal surgery .
The risk factors include advancing age, diabetes, obesity, hypertension, arteriosclerosis, malnutrition, renal failure, immunosuppression, and trauma.
The classic bacteria include Group A beta Hemolytic strep and clostrium perfringens. The infection can be polymicrobial including Proteus mirabilis, E. Coli,
Candida albicans, Pseudomonas, Klebsiella, Staph aureus, Bacteroides, Enterobacter.
The patient presents feeling generally unwell and has pain greater than expected from the visualized area of concern. Findings on exam include a dull redness around the wound, crepitus in the area of the wound, and dirty dishwater coming from wound.
Investigations include: CBC and diff; electrolytes including HCO3 and blood sugar; cross
Match; blood Cultures; urine Culture; cross table flat plate to determine if there is gas in the subcutaneous tissue; and CT Scan.
Initial treatment includes: ICU admission; 2 Large bore IVs; tetanus booster; foley catheter; central Line; arterial line; continuous cardiac monitoring;
Blood sugar qid; culture wound drainage. Patient needs to start broad spectrum antibiotics – including coverage for gram positive (for Clostridium and
Hemolytic strep), gram negatives and anaerobes.
Antibiotic regimens include:
1.
Clindamycin 900 mg IV q8hr + Gentamycin 2 mg/kg bolus then 1.5 mg/kg q8hr or
2.
Ampicillin 2 gm q4hr + Gentamycin (as above) + Metronidazole 500mg q8hr or
3.
Imipenem 500-1000mg q6hr or
4.
levofloxacin 500 mg q24 hr + Metronidazole 500mg q8hr.
Consult plastic surgery and infectious diseases if available.
Urgent wide debridement of necrotic tissue back to healthy muscle or until you get bleeding is necessary. Leave the skin open and pack with saline gauze. Consider
hyperbaric oxygen if available. When the wound starts granulating, use a skin graft or myocutaneous graft.
4.0 Ovarian Masses
4.1 Tubo-ovarian Torsion
Acute adnexal torsion accounts for 3% of all emergent gynecologic surgeries [65].
Complete or partial torsion of the ovarian vascular pedicle compromises the lymphatic and venous drainage (presents as unilateral tender adnexal mass) with eventual loss of arterial perfusion (low grade fever and leukocytosis). The risk factors include: pregnancy, ovarian stimulation; and ovarian enlargement.
Symptoms include acute abdominal pain (stabbing (70%), sudden and sharp
(59%), radiate to the back, flank or groin (51%)), nausea and vomiting (70%), peritoneal signs (3%), and age under 50 yr in 80%. Signs are those of an acute abdomen and cervical motion tenderness when the torted side is put on stretch .
Investigations include CBC (fall in Hgb with hemorrhage and an increase in WBC with necrosis), electrolytes (especially if there has been persistent vomiting), ultrasound.
In children a torted ovary may be normal. In adults a torted ovary may have a large cyst
(up to 80%) [65]. With time the ovary enlarges and may be solid (hyperechoic) or fluid filled (hypoechoic) [20]. Free intraperitoneal fluid in the pelvis results from lymphatic and venous congestion or infarction with intraperitoneal hemorrhage. Intra-ovarian artery flow usually reflects partial torsion resulting from extrinsic compression and occlusion of the ovarian vein with an intact arterial supply [20,65]. Blood flow usually indicates a viable ovary. Doppler ultrasound will document arterial flow.
Detorsion can be used in young women to preserve ovarian function. 93% of detorted ovaries will regain normal ovarian function. Salpingo-oophorectomy should be completed if there is a concern of malignancy or if the tissue is clearly gangrenous. There is a 10% risk of recurrent torsion. Methods to prevent this include oral contraceptives to decrease development of ovarian cysts. Ovariopexy fixes the ovary to the uterus or pelvic sidewall. Ovariopexy is preferred if the problem is seen in childhood [1].
4.2 Hemorrhagic Ovarian Cyst
Physiologic ovarian cysts from corpus luteal or follicular origin can become hemorrhagic [24] The woman may present with acute pelvic pain or a dull constant lower abdominal pain. If you take a menstrual history, she with likely be at the time of ovulation. Rupture of a blood-filled corpus luteum cyst usually gives abdominal pain with guarding and possibly rebound . There is diffuse pelvic tenderness on vaginal exam.
The pain is more pronounced on the side of the ovarian cyst. A mass may or may not be palpated. If the hemorrhage is severe, then the abdominal is distended and there can be hypovolemic shock.
Ultrasound may show a heterogeneous, hypoechoic mass with internal echoes, thin and thick septations, fluid debris level, echogenic retracting clot or irregular nodular wall. Acute intracystic hemorrhage may appear isoechoic to the ovarian stroma and mimic an enlarged ovary [25]. There will be free fluid in the cul de sac and sometimes in the upper abdomen. A
HCG or urine pregnancy test is negative. Culdocentesis will reveal free blood in the abdomen
When there is significant hemorrhage, a laparotomy is indicated to confirm the diagnosis and excise the cyst. The ovarian defect should be closed in layers with fine
absorbable suture. Laparoscopy could be considered in a hemodynamically stable patient, however, it is often difficult to see well in the presence of a significant amount of intraabdominal blood.
6.0 Trauma
6.1
Vulvar Hematoma
Straddle injuries may result in vulvar hematomas (ie. falling on the cross bar of a bicycle). Symptoms include increasing vulvar pain. Signs include expanding vulvar mass and purplish discoloration of the skin. Treatment begins with IV, CBC, Cross match, ice packs and pressure dressings [67]. These hematomas can become quite large as blood dissects through the soft tissue planes. Ensure that the patient is able to void. It may be necessary to incise and drain the hematoma if it continues to expand.
6.2 Sexual Assault
Sexual assault is motivated by power and control issues rather than sexual gratification [66]. In keeping with this statement a 10 year review of vaginal injuries in a teaching hospital in Calabar, Nigeria showed the 68% were related to sexual assault usually in a nulliparous patient, toddler or teenagers [29]. Coital injuries made up
0.7/1000 gynecologic emergencies at that unit. A retrospective review of the literature from 1980-2003 showed that 10-67% of children with STD had been sexually abused, while 15-30% of sexually abused incidents were associated with STD. The alleged child abusers were adult males known by the child (family member (30-60%), teachers, household personnel, neighbor). The extent of this problem in sub-Saharan Africa is not well documented [28]. A report on post-coital injuries at the Addis Ababa Fistula
Hospital in Ethiopia from 1991-1997 showed that 78 of 91 women were sexually abused under the cover of marriage and 9 were kidnapped, raped then discarded. Once the fistula occurred, 59 women were divorced and 19 were abandoned. They advocated for changes which include education, amended polices and laws from government and health care workers [31].
The initial evaluation includes an appropriate history to detect life-threatening injuries, the state of the victim’s overall health (including tetanus status), gynecologic and assault history. The physical exam must be thorough with clear documentation of any signs of trauma and proper evidence collection. The exam usually shows anal or genital injuries, trauma to the perineum or lower third of vagina, vesico-vaginal or recto-vaginal fistula, vaginal bleeding and sometimes shock. In contrast to other centers, 32 cases of vaginal injuries due to coitus are seen annually in a Dakar hospital. The most common location of injury was the posterior upper third of vagina and this was managed with suturing [30].
Management includes vaginal cultures for sexually transmitted diseases
(chlamydia, gonorrhea), blood work for CBC, pregnancy test and possibly cross match.
HIV antibody testing should be done initially and repeated at 6 weeks, 3 months and 6 months. For HIV prophylaxis, the patient should receive zidovudine 300mg bid and lamivudine 150mg bid for 28 days [66]. The CDC recommends sexually transmitted disease prophylaxis for hepatitis B ( Hep B vaccination and repeat at 1 and 6 months and
Hep B immune globulin 0.06 mL/kg IM), Bacterial vaginosis and trichomoniasis
(Metronidazole 2g PO), Gonorrhea (Ceftriaxone 125-250mg IM or Ciprofloxacin 500mg
PO) and Chlamydia (Azithromycin 1g PO or Doxycycline 100mg PO bid for 7 days)
[66]. There are a few options for preventing an unwanted pregnancy. These include the morning after pill (thinly estradiol 100
g and levonorgestrel 0.5 mg and repeat in 12 hours) or 2 Ovral tablets and repeat in 12 hours or placement of a copper IUD with in 5 days of the assault [66]. Counseling is necessary and reporting to legal authorities in keeping with the laws of the country. Prior to discharging the patient, there must be plans for followup in 1-2 weeks and again in 2-4 months. Patient should be informed to return if her menses is more than 2 weeks late. She then requires a pregnancy test and her options need to be reviewed with her.
7.0 Recommendations
1.
The diagnosis is usually made on a thorough history (including a gynecologic history), and physical exam (including a pelvic exam). Laboratory investigations will support the diagnosis and help guide the resuscitation and management.
2.
Where CDC recommended treatment options are not available due to cost, use those management strategies that meet the guiding principles of treating the most likely bacterial/viral cause of infection.
3.
Among the imaging modalities available, the ultrasound is the most powerful tool for assessing the gynecologic patient [65].
4.
Availability of quantitative
HCG would help identify abnormalities in pregnancy at an earlier point in the disease process.
5.
Condoms and other recognized preventative measures against PID and other
STDs should be promoted [70].
6.
The time to learn laparoscopy is in a stable patient. Only in centers where the staff and physician have a good working relationship with the equipment should laparoscopy be considered for the emergency patient.
7.
The surgical approach for a hemodynamically unstable patient is laparotomy.
8.0 Summary
Gynecologic emergencies involve assessment by history and physical examination including a pelvic examination while one is also carrying out the important resuscitation principles of assessing and maintaining an airway, breathing and circulation.
The resuscitation efforts of accessing the venous system and ensuring appropriate fluid infusion can be done while sending off lab work and organizing other investigations appropriate to the situation. The expediency with which all of these maneuvers need to take place depends on the severity of the patient’s presentation. A surgical intervention may be required, so NPO is important along with an assessment of the urinary output.
Where possible, it is important to explain the situation to the patient and family and obtain informed consent. Psychosocial and possible legal consequences of the precipitating problem will need to be addressed once the acute issue is effectively managed and the patient is medically stable.
Laurie Elit MD MSc FRCS(C)
Associate Professor, Department of Obstetrics and Gynecology
McMaster University
Division of Gynecologic Oncology
Hamilton Health Sciences Centre – Henderson site and Juravinski Cancer Centre,
Hamilton, Canada
References
1. Stenchever. Comprehensive gynecology. 4 th ed. C2001. Mosby Inc. p. 413-34,642-
68,707-31.
2. Nadel E, Talbot-Stern J. Obstetrical and gynecologic emergencies. Pearls, pitfalls and updates. Emergency Medicine Clinics of N Am 1997 May;15(2):389-397.
3. Kaakaji Y, Nghiem HV, Nodell C, Winter TC. Sonography of obstetric and gynecologic emergencies. Am J of Reoentgenology 2000;174:651-656.
4. Cochrane Database Syst Rev 2000, 1: CD000324
5. Barnhart, K et al. The Medical Management of Ectopic Pregnancy: A Meta-analysis
Comparing “Single Dose” and “Multidose” Regimens Obstet Gynecol 2003;101:778-84
6. Boardman LA, et al. Endovaginal sonography for the diagnosis of upper genital infection. Obstet Gynecol 1997;90:54-57.
7. Centers for Disease Control and Prevention. 1998 Guidelines for treatment of sexually transmitted disease. Morbidity and Mortality Weekly Report 1997;47:82.
8. Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines. Morbidity and Mortality Weekly Report 1993;42(RR14):1-102.
9. Ness. PEACH Trial. Am J Obstet Gynecol 2002; 186: 929-37.
10. Nguyen HB, Rivers EP, Abrahamian FM, Moran GJ, Abraham E, Trzeciak S, et al.
Emergency Dept Sepsis Education Program and Strategies to Improve Survival (ED-
SEPSIS) Working Group. Severe sepsis and septic shock.: Review of the literature and emergency department management guidelins. Annals of Emergency Med 2006;48:1:28-
54.
11. Levy MM, Fink MP, Marshall JC. 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Intensive Care Med 2003;29:530-538.
12. Fischer M, Bhatnagar J, Guarner J, Reagan, S, Hacker JK, Van Meter SH, et al. Fatal toxic shock syndrome associated with clostridium sordellii after medical abortion. NEJM
2005;353(22);2352-2360.
13. Schorge JO, Granter SR, Lerner LH, Feldman S. Postpartum and vulvar necrotizing fasciitis. Early clinical diagnosis and histopathologic Correlation. J Reprod Med
1998;43:586-590.
14. Piper JM, West P. Necrotizing fasciitis following postpartum tubal ligation. A case report and review of the literature. Arch Gynecol Obstet 1995;256:35-38.
15. Lee Y, Chou T, Peng M, Chang F. Rapidly progressive necrotizing fasciitis caused by
Staphylococcus aureus. J Microbiol Immunol Infect 2005;38:361-364.
16. Wong C, Wang Y. What is subacute necrotizing fasciitis?: A proposed clinical diagnostic criteria. J Infect 2005;20:1-5.
17. Gallup DG, Freedman MA, Meguiar RV, Freedman SN, Nolan, TE. Necrotizing fasciitis in gynecologic and obstetric patients: A surgical emergency. Am J Obstet
Gynecol 187;2:06-311.
18. Walker, BW. Putting the brakes on necrotizing fasciitis. Nursing 2004;34(10):40-41.
19. Schwartz, RA. Necrotizing Fasciitis. Emedicine [Online]. [2006?] [cited 2006 Jan
01]. Available from: http://www.emedicine.com/derm/topic743.htm
20. Yildirim Y, Inal M, Tinar S. Necrotizing fasciitis after abdominal hysterectomy: a report on five cases. Arch Gynecol Obstet; 273:126-128.
21. Kdous M, Hachicha R, Iraqui Y, Jacob D, Piquet P, Truc J. Necrotizing fasciitis of the perineum secondary to a surgical treatment of Bartholin’s abscess. Gyn Obstet
Fertilite 2005;33:887-890.
22. Larsen JW, Hager WD, Livengood CH, Hoyme U. Guidelines for the diagnosis, treatment and prevention of postoperative infections. Infect Dis Obstet Gynecol
2003;11;65-70.
23. Stevens DL. Streptococcal Toxic-shock syndrome: Spectrum of disease, pathogenesis and new concepts in treatment [serial online]1995 [cited 6 Jan 2006];1(3):1-14. Available from: URL: http://www.cdc.gov/ncidod/EID/vol1no3/stevens.htm
24. Burnett LS. Gynecologic cause of the acute abdomen. Surgical Clinics of N Am
1988;68(2):385-398.
25. Stone IK. Atlas of Obstetric and Gynecologic Emergencies.
26. Dao B., Rouamba A, Ouedraogo D, KambouT, Bazie AJ. Transfer of obstetric patients in a pregnant and postpartum condition to an intensive care unit: eight-two cases in Burkina Faso. Gynecol Obstet Fertil 2003;31(2):123-6
27. Ben Salah D., Makni S., Ben Radjeb S. Epidemiology of gram negative bacterial septicemias: data from a Tunisian hospital (1996-1998). Tunis Med 2002;80(5):245-8
28. Pitche P. Child sexual abuse and sexually transmitted infections in sub-Saharan
Africa. Med Trop (Mars) 2005;65(6):570-4
29. Abasiattai AM, Etuk SJ, Bassey EA, Asuquo EE. Vaginal Injuries during coitus in
Calabar: a 10 year review. Niger Postgrad Med J. 2005;12(2):140-4
30. Ciss ct., Dionne P., Cathy A., Mendes V., Diadhiou F., Ndiaye PD. Vaginal injuries during coitus. Dakar Med 1998;43(2):135-8
31. Muleta M., Williams G. Postcoital injuries treated at the Addis Ababa Fistual
Hospital, 1991-1997. Lancet 1999;354(9195):2051-2
32. Moodley M., Marishane T. Demographic variables of gestational trophoblastic disease in KwaZulu-Natal, South Africa. J Obstet Gynaecol. 2005;25(5):482-5
33. Mudokwenuy-Rawdon C., Ehlers VJ., Bezuidenhout MC. Factors influencing post abortion outcomes among high-risk patients in Zimbabwe. Curationis 2005;28(4):74-85
34. Weeks A., Lavender T., Nazziwa E., Mirembe F. Personal accounts of ‘near-miss’ maternal mortalities in Kampala, Uganda. BJOG 2005;112(9):1302-7
35. Africa’s unsafe abortions. Afr Health 1998;21(1):43
36. Granja AC, Machungo F., Gomes A., Bergstrom S. Adolescent maternal mortality in
Mozambique. J Adolesc Health 2001;28(4):303-6
37. Gebreselassie H., Gallo MF., Monyo A., Johnson BR. The magnitude of abortion complications in Kenya. BJOG 2005; 112(9):1229-35
38. Oye-Adeniran BA., Umoh AV., Nnatu SN. Complications of unsafe abortion: a case study and the need for abortion law reform in Nigeria. Reprod Health matters 2002;
10(19):18-21
39. Sepou A., Ngbale R., Uanza MC., Domande-Modanga Z., Nguembi E. Analysis of abortions at a community maternity hospital in Bangui. Med Trop (Mars). 2004;64(1):61-
5
40. Nayama M., Gallais A., Ousmane N., Idi N., Tahirou A., Garba M., Djibrill B.,
Boukerrou M. Management of ectopic pregnancy in developing countries: example of a
Nigerian reference maternity. Gyn Obstet Fertil 2006;34(1):14-8
41. Ikeme AC., Ezegwui HU., Morbidity and mortality following tubal ectopic pregnancies in Enugu, Nigeria. J Obstet Gynecol 2005;25(6):596-8
42. Awori MN, Jani PG. Surgical implications of abdominal pain in patients presenting to the Kenyatta national Hospital casualty department with abdominal pain. East Afr Med J
2005;82(6):307-10
43. Igberase GO., Ebeigbe PN, Igbekoyi OF., Ajufoh BI. Ectopic pregnancy: an 11-year review in a tertiary center in the Niger Delta. Trop Doct 2005;35(3):175-7
44. Anorlu RI., Oluwole A., Abudu OO., Adebajo S. Risk factors for ectopic pregnancy in Lagos, Nigeria. Acta Obstet Gynecol Scand 2005;84(2): 184-8
45. Nkyekyer K., Major gynecological surgery in the Ghanaian adolescent. East Afr Med
2004;81(8):392-7
46. Leke RJ., Goyaux N., Matsuda T., Thonneau PF. Ectopic pregnancy in Africa: a population-based study. Obstet Gynecol 2004;103(4):692-7
47 Cisse CT., Belafia B., Dieme ME., Moreau JC. Minilaparotomy with a minipfannenstiel incision for the early diagnosis of ectopic pregnancy in Africa. Sante
2003;13(3):191-5
48.
Sepou A., Yanza MC., Goddot M., Ngbale R., Kouabosso A., Penguele A., Nali
MN. 116 ectopic pregnancies observed in Bangui (Central African Repulic).
Sante 2003;13(1):29-30
49.
Goyaux N., Leke R., Keita N., Thonneau P. Ectopic pregnancy in African developing countries. Acta Obstet Gynecol Scand 2003;82(4): 305-12
50.
Orji EO., Fasubaa OB., Adeyemi B., Dare FO., Onwudiegwu U., Ogunniyi SO.
Mortality and morbidity associated with misdiagnosis of ectopic pregnancy in a defined Nigerian population. J Obstet Gynecol 2002;22(5):548-50
51.
Gharoro EP, Igbafe AA. Ectopic pregnancy revisited in Benin City, Nigeria: analysis of 152 cases. Acta Obstet Gynecol Scand 2002;81(12);1139-43
52.
Cisse CA., Bernis LD., Faye HO., Diadhiou F. Ectopic pregnancy in Senegal.
Sante 2002;12(2):271-4
53.
Thonneau P., Hijazi Y., Goyaux N., Calvez T., Keita N. Ectopic pregnancy in
Canakry, Guinea. Bull World Health Organ 2002;80(5);365-70
54.
Awojobi OA., Ogunsina S. Ectopic pregnancy in a rural practice. Niger J Med
2001;10(3);139-40
55.
Bussmann H., Koen E., arhin-Tenkorang D., Munyadzwe G., Troeger J. Trop
Med Int Health 2001;6(12):1023-31
56.
Cohen CR, Sinei S, Reilly M., Bukusi E., Eschenbach D., Holmes KK., Ndinya-
Achola JO., Bwayo J., Grieco V., Stamm W., Karanja J., Kreiss J., Effect of human immunodeficiency virus type 1 infection upon acute salpingitis: a laparoscopic study. Ingect Dis 1998;178(5): 1352-8
57.
Bosu WK., Habey D. The availability and cost of antibiotics for treating PID in the Central Region of Ghana and implications for complicance with national treatment guidelins. Int J STD AIDS. 1998;9(9):551-3
58.
Duncan ME., Tibaux G., Kloos H., Pelzer A., Mehari L., Perine PL. STDS in women attending family planning clinics: a case study in Addis Ababa. Soc Sci
Med 1997;44(4):441-54
59.
Leiva A., Shaw M., Paine K., Manneh K., McAdam K., Mayaud P. Management of sexually transmitted diseases in urban pharmacies in the Gambia. Int J STD
AIDS 2001;12(7):444-52
60.
Ryan CA., Zidouh A., Manhart LE., Selka R., Zia M., Moloney-Kitts M.
Reproductive tract infections in primary healthcare, family planning and dermatovenereology clinics: evaluation of syndromic management in Morocco.
Sex Transm Infect 1998;74S1:S95-105.
61.
Beigi RH., Wiesenfeld HC. Pelvic inflammatory disease: new diagnostic criteria and treatment. Obstet Gynecol Clin N Am. 2003;30:777-793
62.
Della-Giustina D., Denny M. Ectopic Pregnancy. Emerg Med Clin N Am.
2003;21, 565-584
63.
Zeger, W., Holt, K. Gynecologic infections. Emerg Med Clin N Am.
2003;21;631-48
64.
Coppola, P.T., Coppola, M. Vaginal Bleeding in the first 20 weeks of pregnancy.
Emerg Med Clin N Am. 2003;21:667-677
65.
Harrison, B.P., Crystal, C.S. Imaging modalities in obstetrics and gynecology.
Emerg Med Clin N Am 2003:21:711-735
66.
Cantu, M., Coppola, M. Lindner, A.J., Evaluation and management of the sexually assaulted women. Emerg Med Clin N Am. 2003;21;737-750
67.
Daniels, R.V., McCusker, C. Abnormal vaginal bleeding in the nonpregnant patient. Emerg Med Clin N Am. 2003;21:751-772
68.
Hajenius PJ, Mol BWJ, Bossuyt PMM. Ankum WM, Van der Been F.
Interventions for tubal ectopic pregnancy. The Cochrane Database of Systematic
Reviews 2006;2:1-101
69.
Forna F, Gulmezoglu AM. Surgical procedures to evacuate incomplete abortion.
The Cochrane Database of systematic reviews. 2006;2:1-17
70.
Sangani P, Rutherford G, Wilkinson D. Population-based interventions for reducing sexually transmitted infections, including HIV infection. The Cochrane
Database of Systematic Reviews. 2006;2:1-23
71.
McConkey SJ, McConkey SJ. Case series of acute abdominal surgery in rural
Sierra Leone. World Journal of Surgery 2002; 26(4):509-513.
Multiple Choice Questions – right answers are x
1.
25 year old presents with 7 weeks amenorrhea, new onset right lower quadrant pain for the last 3 hours, nausea and vomiting. BP=90/60. HR= 100/min.
RR=24/min. The abdomen is distended and there is guarding especially in the right lower quadrant. On pelvic exam, there is a 4 cm mass in the right adnexa and there is significant tenderness when the right adnexa is put on stretch. Your differential diagnosis is: a.
Chlamydia cervicitis b.
Endometritis c.
PID d.
Corpus luteum cyst in pregnancy x e.
Ectopic pregnancy x
2.
Your management is: a.
Watch patient and re-examine in 4-6 hours b.
Start an IV, send lab work, do a urine pregnancy test, pelvic ultrasound x c.
Start antibiotics d.
Culdocentesis x e.
Laparoscopy/laparotomy to make a diagnosis x
3.
60 year old woman comes to emergency 48 hours after a laparoscopy to remove an ovarian mass. She is known to have diabetes, hypertension and heart disease.
She has excrusciating pain at the left lower quadrant trochar site. There is brown dish water like material coming from the site. There is a purple hughe to the tissues around the site. BP=90/60. HR= 100/min. RR=30/min. Differential diagnosis is: a.
trauma to small bowel x b.
trauma to large bowel x c.
trauma to bladder d.
wound cellulits x e.
necrotizing fasciitis x
4. Your management would be a.
check for crepitus in the tissue by palpation or plain XRay x b.
Consult General Surgery, Plastic Surgery, Infectious Disease, Intensive
Care x c.
Start an IV, place a foley cateter x d.
Broad spectrum high dose antibiotics x e.
Plan surgery to widely debride the wound x
5. 40 year old woman is rushed into emergency. She is unconscious and cannot give a history. She is bleeding profusely on a towel between her legs. BP = 60/40,
HR=130/min, RR=24/min, Afebrile. What do you do first: a.
Try to find someone who can give a history
b.
b.Complete physical exam c.
Send off lab work including: CBC, Cross Match d.
Start 2 large bore IVs x e.
Go to the operating room
6.
Once you have begun the resuscitation and gotten appropriate personel to help, you begin the pelvic exam. There is extensive bruising of the suprapubic region, upper thighs bilaterally, and the left vulva is huge looking like it is going to rupture blood clot everywhere. This injury is compatible with: a.
trauma from falling on the cross bar of a bicycle x b.
trauma from a sexual assault x c.
vulvar cancer d.
motor vehicle accident x e.
recent vulvar surgery ie., episiotomy, I+D Bartholins abscess.