SCHIZOPHRENIA LECTURE OUTLINE
advertisement
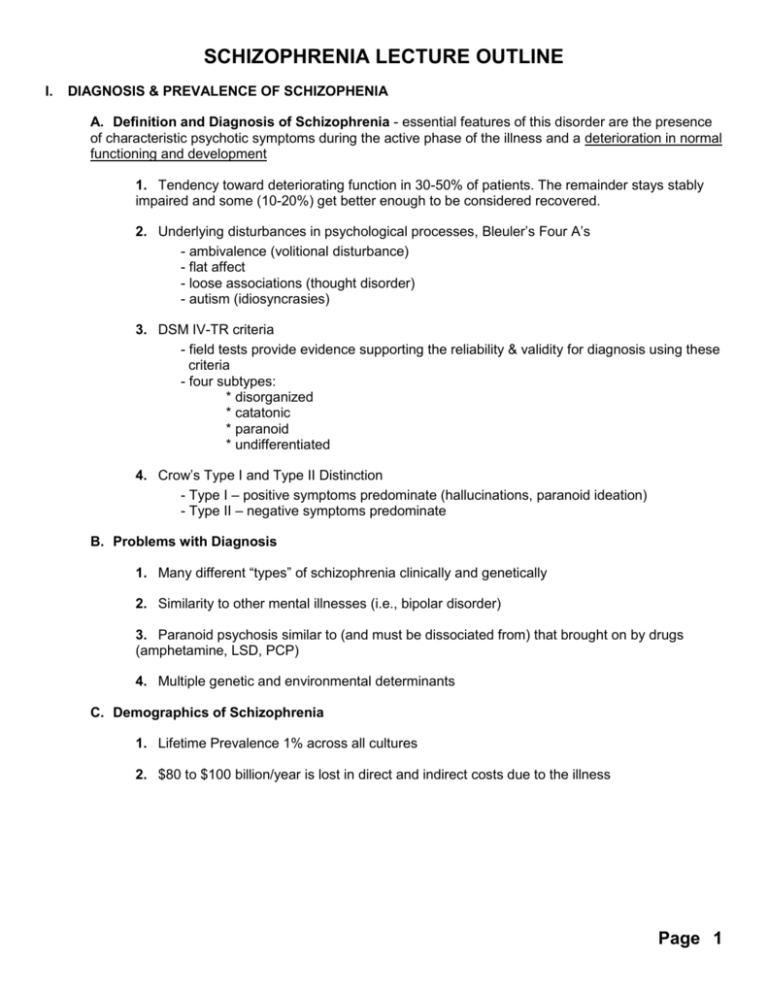
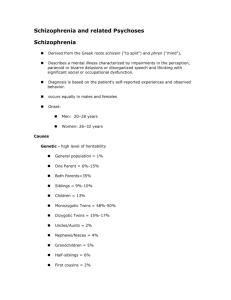
SCHIZOPHRENIA LECTURE OUTLINE I. DIAGNOSIS & PREVALENCE OF SCHIZOPHENIA A. Definition and Diagnosis of Schizophrenia - essential features of this disorder are the presence of characteristic psychotic symptoms during the active phase of the illness and a deterioration in normal functioning and development 1. Tendency toward deteriorating function in 30-50% of patients. The remainder stays stably impaired and some (10-20%) get better enough to be considered recovered. 2. Underlying disturbances in psychological processes, Bleuler’s Four A’s - ambivalence (volitional disturbance) - flat affect - loose associations (thought disorder) - autism (idiosyncrasies) 3. DSM IV-TR criteria - field tests provide evidence supporting the reliability & validity for diagnosis using these criteria - four subtypes: * disorganized * catatonic * paranoid * undifferentiated 4. Crow’s Type I and Type II Distinction - Type I – positive symptoms predominate (hallucinations, paranoid ideation) - Type II – negative symptoms predominate B. Problems with Diagnosis 1. Many different “types” of schizophrenia clinically and genetically 2. Similarity to other mental illnesses (i.e., bipolar disorder) 3. Paranoid psychosis similar to (and must be dissociated from) that brought on by drugs (amphetamine, LSD, PCP) 4. Multiple genetic and environmental determinants C. Demographics of Schizophrenia 1. Lifetime Prevalence 1% across all cultures 2. $80 to $100 billion/year is lost in direct and indirect costs due to the illness Page 1 II. PREDISPOSING FACTORS & MODELS A. Weighted Polygenic Model based on inheritance and adoption studies Inheritance: (Dr. Irving Gottesman) If the “probands” (patient) has schizophrenia, then: Parentage: Concordance: Monozygotic Twins 65% or greater Dizygotic twins, Siblings approx. 12% One Parent Affected 5-10% Two Parents Affected 46% Second Degree Relative 2-4% Baseline – Population 1% Adoption Studies: provide further evidence for genetically-linked risk factors High incidence of schizophrenia in the adopted offspring of parents with schizophrenia who have been reared by parents who do not have the disorder. The genetics of schizophrenia is complex, very similar to diabetes and hypertension, and involves (susceptibility) gene-environment (e.g., amphetamine use) interactions. III. DSM IV-TR DIAGNOSTIC CRITERIA FOR SCHIZOPHRENIA A. Characteristic Symptoms: Two (or more) of the following, each present for a significant portion of time during a 1-month period (or less if successfully treated): (1) Delusions (2) Hallucinations (3) Disorganized speech (e.g., frequent derailment or incoherence) (4) Grossly disorganized or catatonic behavior (5) Negative symptoms, i.e., affective flattening, alogia, or avolition NOTE: Only one Criterion A symptom is required if delusions are bizarre or hallucinations consist of a voice keeping up a running commentary on the person’s behavior or thoughts, or two or more voices conversing with each other. Also disorganized speech and behavior reflects disorganized thinking. B. Social/Occupational Dysfunction: For a significant portion of the time, since the onset of the disturbance, one or more major areas of functioning such as work, interpersonal relations, or self-care are markedly below the level achieved prior to the onset. In a few cases, the premorbid adjustment is extremely impaired. C. Duration: Continuous signs of the disturbance persist for a least 6 months (unless treated successfully) Page 2 IV. FACTORS INVOLVED IN THE DEVELOPMENT AND MAINTENCE OF SCHIZOPHRENIA A. Predisposing Factors: 1. Vulnerability – Personality: Traits/Disorders are modestly “predictive” a. suspicious personality (paranoid) b. withdrawn personality (schizoid) c. odd, eccentric personality (schizotypal) 2. Vulnerability – Genetics (see above) B. Precipitating Factors: 1. Stress – Biological a. drugs, like LSD b. post partum c. stimulant drugs (dopamine agonists like amphetamine) are major “offenders” 2. Stress – Psychological: stress which is translated into brain functional changes 3. Stress – Family: stress does not “cause” schizophrenia, but a “high expressed emotion” environment can affect the course of the disorder C. Sustaining Factors – Outcome is Multifactorial 1. Social function 2. Vocation function 3. Symptoms Schizophrenia Flow Diagram: OUTCOME AND FUNCTION PSYCHIATRIC SYMPTOMS COGNITION ATTENTION AND INFORMATION PROCESSING PATHOLOGY GENETIC SUBSTRATES Page 3 PSYCHOLOGY 179: DRUGS, ADDICTION AND MENTAL DISORDERS ANTIPSYCHOTIC DRUGS Drug Daily Dose Sedation Anticholinergic Side Effects Extrapyramidal Side Effects Potency chrlorpromazine (Thorazine)* 300-800 mg high high low low Olanzapine (Zyprexa) 2.5-15 mg moderate moderate none high haloperidol (Haldol)* 6-20 mg low low high high risperidone (Risperdal) 4-8 mg low low moderate high clozapine (Clozaril)# 300-450 mg low moderate low low Half-life: 10-20 hours; only need to be administered once per day. * High potency antipsychotics show less sedation, less anticholinergic effects and more extrapyramidal side effects. Low potency antipsychotics have the opposite effect. # Requires weekly blood test during treatments because clozapine can produce agranulocytosis (loss of white blood cells). Page 4