Lecture 7: Gastrointestinal & Hepatobiliary System
advertisement

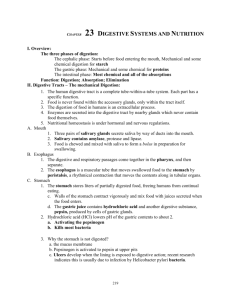
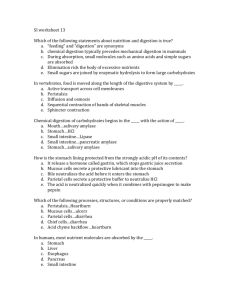
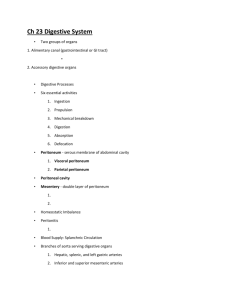
1 Objectives for the Gastrointestinal System Lecture 1. Identify the organs of the digestive tract & the accessory organs 2. State the function of the digestive tract 3. Describe the histological cells of the GI tract and their function 4. Describe the types of movement through the GI tract 5. Explain the nervous system innervation of the GI tract 6. Compare the differences of the parasympathetic & sympathetic nervous system on GI tract 7. Review the parts of the oral cavity and the function of the salivary glands 8. Explain the process of swallowing 9. Name the regions of the stomach 10. Discuss the structure of the gastric wall & the function of the gastric cells 11. Explain the process of digestion & motility 12. Discuss the hormone function & gastric secretion 13. List the divisions of the small intestine 14. Describe the structure of the intestinal wall 15. Discuss the hormonal & intestinal secretions & their function 16. List the division of the large intestine 17. Explain the process of motility, absorption, & defecation from the large intestine 18. Discuss the function of the pancreas as an exocrine organ and its role in digestion 19. Explain the structure and function of the liver and its role in digestion 20. Explain the function of the gallbladder 21. Discuss cellular metabolism & energy production comparing carbohydrates, lipids, proteins 2 Lecture 7: Gastrointestinal & Hepatobiliary System I. Structure and Organization A. Divisions (tract tube from mouth to rectum) 1. Upper (mouth, esophagus, stomach) – intake 2. Middle (small intestine – duodenum, jejunum, ileum) – digestion 3. Lower (cecum, colon, rectum) – storage & elimination channel 4. Accessory organs (slivary glands, liver, pancreas) – juices for dismantle, use, & storage of food B. Functions of the GI tract 1. Ingestion 2. Mechanical processing 3. Digestion 4. Secretion 5. Absorption 6. Excretion C. Histological Organization 1. Mucosa = inner lining a. Epithelial surface with glandular secretion & connective tissue lining 1) Mucosal folds – increases surface area for expansion & absorption 2) Villi – fingerlike projections in small intestine – increase surface area b. Cells of mucosa = columnar epithelium with secretory cells c. Muscularis mucosae = band of smooth muscle & elastic fibers 2. Submucosa – loose connective tissue around muscularis mucosae a. Contains blood vessels & lymphatic vessels & nerves b. Submucosal plexus = neural tissue for smooth muscle movement & glandular secretions 3. Muscularis Externa – smooth muscle in circular & longitudinal pattern a. Mixing and movement function b. Autonomic reflex of myenteric plexus 1) Parasympathetic 2) Sympathetic 4. Serosa – serous membrane over the muscularis externa a. Visceral peritoneum lines peritoneal organs b. Parietal peritoneum line abdominal wall c. Mesenteries – loose connective tissue connects visceral & parietal 1) Contains access route for blood, nerves & lymph 2) Suspends jejunum & ileum – double folded 3) Attached to dorsal abdominal wall = fan shaped 4) Greater omentum = double fold of peritoneal membrane a) Extend from stomach, covering transverse colon & intestines – helps control infection spread 3 5) Lesser omentum – between transverse fissure liver & lesser curve stomach D. Movement of Digestive Tract (propelling of food forward) SHOULD BE FORWARD 1. Smooth muscle movements with tonic/clonic movements a. Tonic – sphincters & continuous lasting minutes to hours b. Rhythmic movements – intermittent contraction for mixing & moving c. Peristaltic movements – contractile band forward movement 1) Wave movement 2) Propulsive movements/Contraction starts behind substance the longitudinal shorten, circular moves chyme forward d. Segmentation – churn substances no actual directional moving 2. Innervation – enteric nervous system – inside the wall of GI tract a. Intramural neurons (myenteric & submucosal plexuses) – ANS affects stretch & chemoreceptor for chemical balance (pH, protein & fats) 1) Myenteric plexus – between circular & longitudinal layers a) Interconnecting neurons extending entire length of GI b) Function- motility 2) Submucosal (Meissner) plexus – between mucosal & circular muscles a) Function- control of motility, intestinal secretions, absorption 3) Communicate with receptors in mucosal, muscle, mechanical & chemical responses b. Autonomic Nervous System (both parasympathetic & sympathetic) 1) Parasympathetic via vagus nerve to stomach, small intestine, cecum, ascending colon & transverse colon a) Parasympathetic fibers via pelvic nerve b) Excitatory 2) Sympathetic via thoracic chain of sympathetic ganglia, celiac, superior mesenteric & inferior mesenteric ganglia a) Mediated by neurons in intramural plexuses b) Function: control mucus secretion, reduces motility by inhibiting intramural plexus, enhances sphincter tone, increases smooth muscle tone of blood vessels 4 II. Organs of GI Tract A. Oral Cavity 1. Function a. Initial entry & sensation b. Initial dismantle through mechanical processes c. Lubricates d. Initial digestion of carbohydrates 2. Structure a. Buckle Cavity 1) Cheeks 2) Lips or labia 3) Vestibule – space between teeth & cheeks 4) Gingivae 5) Hard Palate – anterior 6) Soft Palate – posterior 7) Lingual frenulum – tongue connector 8) Uvula b. Tongue 1) Muscular 2) Mechanical processing 3) Manipulation 4) Taste 5) Lingual tonsils – lymph nodes 6) Sensation – touch, temperature, c. Salivary Glands (protect, lubricates, coats, antimicrobial, digestion) 1) Parotid salivary gland- below zygomatic arch in face (front of ear) 2) Parotid duct – empties into vestibule at 2nd molar 3) Sublingual salivary gland – floor of mouth – under front tongue 4) Submandibular salivary- floor of mouth behind teeth on side Lingual frenulum 5) Secretions (1.0-1.5 L/day; 99.4% H2O) a) Salivary amylase – enzyme breaks complex carbohydrates (starches & glycogen) (1) Buffer & mucus b) Change in pH to slightly basic c) Controlled by ANS d. Teeth 1) Function = mastication 2) Structure (28 for adult & 20 for child) a) Crown – exposed area above gum line b) Enamel – covers crown c) Dentin – bulk of tooth like bone but no live cells d) Pulp cavity – contains root, nerves, blood vessel sits in bony socket e) Periodontal ligament – root to surrounding bone 5 3) Types of teeth a) Incisors – clip & cut b) Cuspids – tearing c) Bicuspids- Crushing, mashing d) Molars – crushing, mashing B. Pharynx – common passage for food, liquids, air 1. Esophagus – muscular, collapsible tube connects mouth & stomach a. Muscles 1) Upper = skeletal 2) Middle – replacing with smooth muscles 3) Lower 1/3 – smooth b. Function – passage of food from mouth to stomach esophageal hiatus c. Sphincters 1) Upper- pharyngoesophageal = striated muscle & squamous Epitheal stratified cells 2) Lower – gastroesophageal – circular muscle a) Passes through diaphragm via esophageal hiatus 2. Swallowing & esophageal motility (bolus) a. Begins with chewing b. Swallowing reflex (starts as voluntary and moves to involuntary) 1) Tactile receptors in pharynx & esophagus stimulate medulla & pons = swallowing center 2) Cranial nerves – V (trigeminal), IX ( glossopharyngeal), X (vagus), XII ( hypoglossal) 3) Phases a) Oral b) Pharyngeal c) Esophageal C. Stomach – pouch ( volume 50-1000ml) 1. Function a. Temporary storage b. Mechanical breakdown - chyme c. Begins digestion – acids & enzymes d. Intrinsic factor – Vitamin B12 2. Regions a. Cardia b. Fundus c. Body – rugae 1) Muscles – longitudinal, circular & inner oblique 6 d. Pylorus e. Antrum f. Pyloric sphincter g. Cardiac sphincter 3. Gastric Wall (epithelium & mucous cells) a. Structure 1) Muscles 2) Rugae 3) Gastric pits a) Shallow depressions in wall contain gastric glands 4) Gastric glands – parietal & chief cells 5) Gastric Juices – secreted by parietal & chief b. Cells 1) Parietal Cells a) Secrete intrinsic factor & HCL (1) HCL – acid kills microbs, breaks down cell walls & connective tissue in food activates chief cells (2) Intrinsic factor – helps absorb Vitamin B12 2) Chief Cells a) Secrete pepsinogen (1) Pepsinogen inactive enzyme = pepsin (2) Pepsin – breaks proteins 3) Rennin & gastric lipase – infant stomach for milk digestion c. Regulation of activity controlled by CNS & hormones 1) Phases a) Cephalic – sight , smell, thought, taste - CNS (1) Vagus nerve parasympathetic nerves Stimulate (2) Chief, parietal, mucus,& endocrine cells (3) Gastric juices activated (500ml/h) b) Gastric phase – food arrival = gastrin (1) Stretch receptors & chemoreceptor active Mucosa that stimulate movement (2) Release of gastrin (hormone) (3) Chief & parietal cells active by gastrin Parietal most active & pH drops (4) Muscle movement = chime (5) Each muscle squirts through pyloric sphincter c) Intestinal phase – chyme enters small intestine (1) Control rate of empty most inhibitory (2) Secretin, cholecystokinin, & gastric inhibitory peptide released (3) Enterogastric reflex – stretch in intestine inhibits neural stimulation of gastrin production & gastric motility 7 (4) Allows time for intestines to deal with gastric acid arrival (5) High with large amounts in stomach & low protein diet (alcohol & carbohydrates leave quick) d. Digestion Process 1) Proteins by pepsin & carbohydrates by amylase continue initial 2) pH falls to 4.5 in 1-2 hours 3) pH falls to 2.0 = pepsin increased activity (protein digestion NOT completed in stomach only started) 4) Little absorption due to mucosal cells of lining, lack of transport In epithelial cells, lining impermeable to water Pain : Hollow organs diffuse but solid organs localized e. Motility 1) Churning & grinding starts in pacemaker area (middle) 2) Contractions 3-5/minute with duration 2-20 seconds 3) Forward & backward movement until smaller particles 4) Physiologic sphincter prevents backward gastric flow a) Bile salts toxic to stomach & stomach acid to SI 5) Enteric nervous system control (para & sympathetic NS) 6) Disorders of motility = too fast or too slow f. Hormones ( locally, distal, & with CNS & ANS) 1) Stomach (gastrin & ghrelin) a) Gastrin (1) Produced by G cells (2) Stimulates gastric acid secretion (3) Growth producing effect on mucosa SI, colon b) Ghrelin (1) Produced endocrine cells in mucosal layer of fundus (2) Growth hormone releasing activitiy (3) Stimulatory affect on intake & digestion g. Gastric secretion 1) Oxyntic (gastric) glands – parietal & chief cells a) Proximal 80% fundus of stomach b) Secrete HCL, pepsinogen, intrinsic factor, mucus c) Composed of glands & pits d) Lined with mucus producing epithelial cells e) Oxyntic cells – HCL & intrinsic factor with chief cells 2) Pyloric glands – a) Distal 20% stomach b) Secrete mucus, some pepsinogen & gastrin 3) Mucosal resistance to acid a) Damage by NSAID, alcohol, bile salts = ulceration 8 4) Prostaglandins protect mucosal surface h. Innervations 1) Parasympathetic = vagus 2) Sympathetic = celiac ganglia 3) Regulation D. Small Intestine (5 hours for passage through) – 90% nutrients absorbed here 1. Divisions – attached to abdominal wall by mesenteries a. Duodenum – receives chyme & pancreas, liver secretions 1) Common bile duct & pancreatic duct 2) Lies outside the peritoneal cavity b. Jejunum – most chemical & nutrient digestion 1) Supported by mesentery c. Ileum – flow ileum to cecum of large intestine; longest 2. Intestinal Wall a. Plicae – folds b. Villi – finger like projections (columnar epithelium) = brush border 1) Increase surface area absorption – 2200 sq ft 2) Capillary network – respiratory gases & nutrients to hepatic 3) Nerves 4) Lymph= lacteal (transport things can’t go vascular – milky) a) Chylomicrons 5) Intestinal glands at base – intestinal juices (1.8 liters/day) a) Osmosis b) Touch & Stretch 6) Duodenal glands or Submucosal glands – alkaline mucus 3. Intestinal Motility (5 hours movement through) a. Mixing & propulsive 1) Pacemaker cells keep contractions going 2) Segmental & propulsive movements a) Mixing with secretions b) Increasing post meals b. Gastroenteric reflex – increase glandular secretions & movement c. Gastroileal Reflex – gastrin release & opens ileocecal valve d. Parasympathetic stimulates GI but Sympathetic inhibits 4. Hormones ( neutralized acid chyme) a. Secretin – S cells in mucosa duodenum & jejunum 1) Inhibits secretion of gastric acid & increase water 2) Stimulates pancreas & liver secretion – high bicarbonate 3) Secreted when pH falls in duodenum b. Cholecystokinin (CCK) - dueodenum 1) Secreted by I cells in intestinal mucosa with large lipids & partially digested proteins 2) Stimulates pancreas – primary function 9 3) Intensifies secretin action, biliary & gallbladder , & gastric empty (gallbladder = bile) c. Glucose-dependent insulintropic polypeptide (previous gastric inhibitory peptide) = fats & carbohydrates 1) K cells mainly jejunum 2) Lower blood glucose by helping insulin release d. GLP-1 – L cells distal small bowel 1) Lower blood glucose levels 2) Suppress glucagons release 3) Slows gastric emptying 4) Helps glucose clearance 5) Decreases appetite & body weight e. Gastric inhibitory peptide – 1) Inhibits gastric acid secretion 2) Inhibits gastric motility & empty f. Vasoactive Intestinal peptide (VIP) 1) Mediates relaxation of GI smooth muscle 2) Relax vascular smooth muscle g. Gastrin-releasing peptide (GRP) 1) Gastric mucosa & function with release gastrin a) Duodenal cells & distal portion stomach 2) Increases stomach motility & production acids & enzymes h. Enkephalin 1) Slow transit of material thru gut 2) Inhibit intestinal secretions NOTE: pg. 602-603 5. Intestinal Secretions a. Brunner glands – mucus producing glands – 1) High concentration where stomach, liver, pancreas secretions meet in duodenum 2) Alkaline mucus 3) ANS control b. Crypts of Lieberkuhn – intestinal mucosal layer; serous fluid 1) Vehicle for absorption – 2000ml/day 2) Aids in absorption with enzymes c. Surface enzymes – aid in absorption 1) Peptidase – split amino acids & sugars E. Large Intestine 1. Division a. Cecum – blind pouch 1) Ileocecal valve – prevents return of feces into SI 2) Appendix b. Colon – haustra = pouches 10 1) Ascending – appendix tail 2) Transverse 3) Descending 4) Sigmoid c. Rectum – end tract d. Anal canal (sphincters) - defecation 1) Internal anal sphincter 2) External anal sphincter 2. Function a. Reabsorption water & final processing b. Absorption vitamins freed by bacterial action (Vitamin K, B5, Biotin) c. Storing fecal material for defecation 3. Motility a. Haustration – digging action – complete exposure to intestinal wall b. Propulsive movement c. Mass movement 4. Absorption a. Reabsorption water ( initial 1500 enters, 1300 reabsorbed, 200 leaves) b. Composition of feces ( 75% water, 5% bacteria, 20% digestive mix) c. Absorption of other 1) Vitamins generated by bacteria a) Vitamin K – clotting b) Biotin – glucose metabolism c) Vitamin B5 – steroid hormones & neurotransmitters 2) Bilirubin – break down of heme & secreted in urine post LI conversion 3) Bile Salts- cecum reabsorbs & transports to liver 4) Toxin – breaks toxins to nontoxin & excretions kidneys or gas producing hydrogen sulfide (odor) & excreted a) Ammonia, Nitrogen compound, Hydrogen sulfide d. Gases – undigestible polysaccharides 5. Defecation (voluntary or involuntary) a. Powerful peristaltic contraction; motility change= diarrhea b. Defecation reflex – 2 positive feedback loops 1) Stretch 2) Parasympathetic c. Sphincters – can fatigue 1) Internal – stretch relaxes 2) External – voluntary control a) Valsalva 6. Large Intestinal Secretion – mucus 11 F Accessory Organs 1. Pancreas – behind stomach toward spleen (exocrine & endocrine) a. Exocrine organ – primary digestive enzyme & buffer 1) Lobules a) Acinar Cells – digestive enzymes (1) Ducts together form larger ducts to one duct Pancreatic duct – duodenum (2) Pancreatic duct duodenal wall via common bile duct from liver & gallbladder (3) Trypsin inhibitor factor 2) Proteolytic enzymes – break proteins (trypsin, chymotrypsin, Carboxypeptidase) ***** Enzymes of pancreas for digestion ONLY become activated in intestines****** 3) Pancreatic amylase – starches & lipase 4) Enzymes from pancreas activated in intestine (self destruct) a) Secreted to bring pH of chyme more neutral levels sodium bicarbonate b) Enzymes (1000 ml/day) = pH 7.5-8 (1) Pancreatic amylase (2) Pancreatic lipase (3) Nucleases (4) Pancreatic proteases 5) Pancreatic agents a) Somatostatin – inhibits gastrin release & gastric acid secretions b) Histamine – potentiates action gastrin & acetylcholine on gastric acid secretion (1) Histamine type 2 (H2) antagonists reduce gastric acid secretion by blocking H2 b. Endocrine = islet cells – insulin & glucagon (1%) 2. Liver – largest organ located right upper quadrant abdominal cavity under lower Ribs a. Glisson Capsule – tough fibroelastic capsule b. 2 lobes anterior ( right & left) c. 2 lobes posterior ( caudate & quadrate) d. Blood supply = 25% blood supply & reservior 1) Hepatic artery (300 ml/minute) 2) Portal vein (1050 ml/minute)- valveless empties to inferior vena cava a) Blood from stomach, SI, LI, pancreas, spleen b) Supplies 60-70% oxygen needs liver c) Liver stores 450ml blood (reserve for needs) 3) Venous outflow – valveless – inferior vena cava 12 e. Lobules – functional units (50-100,000/lobule) – hepatocytes = cells 1) Organization a) Central vein empties into hepatic vein to vena cava b) Terminal bile ducts, portal vein & hepatic artery in periphery of lobule c) Radiation of cells outward from central vein like spokes of wheel d) Cells separated by sinusoids – peripheral lobule to central vein e) Sinusoid supplied by portal vein & hepatic artery (every cell exposed to blood due to 2 layer thickness) – filters f) Sinusoids 2 cell types (line the sinusoid) (1) Kupffer – removal & phagocytic for blood, bacteria, foreign material – filter (2) Endothelial cells g) Bile canaliculi – between cell membrane adjacent hepatocytes – bile drains h) Hepatobiliary Tree – intra & extrhepatic bile ducts (1) United = common bile duct i) Hepatopancreatic ampulla (ampulla of Vater) = junction of pancreatic duct with common bile j) Sphincter of Oddi – muscle tissue at the duodenum bile regulation 2) Hepatic Portal System Circulation a) Blood flows from celiac, superior & mesenteric arteries to liver via hepatic portal system b) Blood contains substances absorbed by GI with high glucose, amino acids, wastes, toxins c) Blood mixes from one capillary to another in system d) Liver regulates concentration of nutrients in body e) Flow pattern (1) Inferior mesenteric vein (2) Splenic vein (3) Superior mesenteric vein (4) Hepatic portal vein (5) Gastric veins (6) Cystic fein (7) Liver capillaries (8) Inferior vena cava 13 f. Metabolic function ( bile, metabolizes hormones & drugs, synthesizes proteins, glucose, blood clotting factors, stores vitamins & minerals, changes ammonia to urea, converts fatty acid to ketones) 1) Carbohydrates, proteins, lipid metabolism a) Carbohydrates (1) Glucose balance (2) Stores glucose as glycogen (3) Synthesizes glucose from amino acid, Glycerol & lactic acid (4) Converts excess carbohydrates to triglyceride & stores in adipose tissue b) Proteins (1) Albumin – plasma colloidal osmotic pressure (a) Binding & transport of hormone, fatty acids, bilirubin (2) Fibrinogen & blood clotting factors (3) Reactions – transamination & deamination (4) Affected by pancreatic enzymes trypsin, chymotrypsin, carboxypeptidase break to single amino acids c) Lipids (1) Oxidation of fatty acids for energy (2) Cholesterol, phospholipids synthesis (3) Formation of triglycerides from carb & protein (4) Fatty acids split into acetyl-coenzyme A = ATP, cholesterol & bile acids 2) Drugs & Hormone Metabolism – removal wastes & toxins a) Metabolizes substances kidneys can’t b) Reactions c) Biotransformation d) Hormone & antibody deactivation 3) Other Functions a) Synthesis of plasma proteins b) Synthesis of clotting factors c) Inactivation of angiotensinogen d) Phagocytosis of RBC e) Blood storage g. Bile production = emulsification 1) Bile = digestion fats & fat-soluble vitamins from intestine 2) Produce 600-1200 ml /day 3) Contents – water, bile salts, bilirubin, cholesterol, fatty acid 14 Lecithin, electrolytes 4) Bile salts a) Emulsify fats b) 94% enter intestine & reabsorb by portal circulation c) Recycled in liver 3. Gallbladder a. Function 1) Bile storage (40-70 ml when full) 2) Bile modification b. Cholesterol is soluble by action of bile c. Food causes contraction with movement bile into duodenum d. Stimulus hormonal 1) Cholecystokinin – gallbladder contraction e. Bile passage regulated by pressure in common duct 1) Muscle around sphincter = hepatopancreatic sphincter f. Bile secretion essential for digestion dietary fats, absorption of fats & fat-soluble vitamins from intestine g. Bile produced in liver stored in gallbladder 1) Sphincter of Oddi – entry to SI with bile h. Symptoms = 4 F’s (female, fertile, 40, fat) – R shoulder pain III. Metabolism = chemical reactions of body to form energy (ATP) A. Cellular – nutrient enter cell across cell membrane to produce energy to survive 1. Catabolism – breakdown to release energy 2. Anabolism – making of new organic compounds (ATP driven) a. Structural maintenance b. Support growth c. Produce secretions 3. Carbohydrate (glycolysis = 2, Krebs = 2, Electron = 36) - monosaccharides a. Glycolysis – glucose breakdown to pyruvic acid (2 ATP )- no O2 b. Mitochondrial energy – mitochondria gets all the energy possible 1) Aerobic (oxygen) environment – citric acid a) Citric acid cycle – inside the mitochondria b) Krebs cycle c. Electron Transport system – inside mitochondria membrane – O2 1) Produces most energy at 36 molecules ATP from 1 glucose 2) Eventually produces H2O d. Anaerobic (lack of O2) stops Krebs & electron transport – pyruvic acid 1) Glycolysis can continue with still 2 ATP 2) Pyruvic acid builds to lactic acid – shifts pH acidic e. Gluconeogensis – generation of glucose from other carbohydrates, glycerols 1) Stored in liver as glycogen- used when glucose not in fluids f. Digestion of Carbohydrates 1) Begins 2) Duodenum 3) Diffusion 15 4) Empty to portal vein 4. Lipid – (Chylomicrons – blood) a. Lipids broken to pyruvic acid - lipolysis b. Energy reserve c. Stored in cytosol –difficult for water soluble enzymes to reach & active d. Mobilized in mitochondria which needs O2 – unable to give large amounts in short time e. Synthesis- most occurs in liver 1) Lipogenesis – synthesis 2) Linoleic, aracidonic, & linolenic acids – essential fatty acids NOT produced by body – dietary needed a) Synthesize prostaglandins & phospholipids for cell membrane b) Unsaturated fat found in plants corn, peanut, soy f. Transport & distribution ( lipoproteins – complex) 1) Lymphatic capillaries transport triglycerides absorbed by Skeletal, cardiac muscles, adipose tissue & liver a) Transported as triglycerides in lipoprotein b) Stored in adipose tissue 2) Low density lipoproteins (LDL) – transport cholesterol Between liver & tissues – arterial plaque 3) High-density lipoproteins (HDL)- transport excess Cholesterol from tissue to liver for storage & excretion 4) Free fatty acids – diffuse easily across cell membrane Bound to albumin & utilized by liver, cardiac, muscle Skeletal cells for energy g. Fat metabolism can produce ATP but also Ketones 5. Protein – can be utilized for energy but less yield ATP (amino acids – blood) a. Requires a Vitamin B6 derivative for transamination b. Needed for protein synthesis c. Quick source they are not 1) Byproduct = ammonia 2) Difficult to break 3) Important component & excessive breakdown = threat d. Protein synthesis 1) Protein intake is essential for body’s ability to synthesize 2) Needs 10 elements essential amino acids only makes 2 3) Dietary intake necessary for rest e. Transamination – ammonia = urea 6. Vitamins a. Water soluble – B, Folic, C, Biotin 1) Not stored with rapid exchange & excreted b. Fat soluble – A,E,K,D – absorbed via GI 16 1) Reserve 2) Can be a problem if excessive intake 7. Minerals (K, Cl, Mg, Iron, Copper, Ca) a. Functions b. Dietary c. Small storage 8. Water intake a. Most via oral intake b. Small amount from metabolic functions 9. Thermoregulation – changes with age a. Exchange 1) Radiation 2) Conduction 3) Convection 4) Evaporation b. Loss & Gains in heat c. Heat production 1) Metabolic 2) Shivering 3) Nonshivering thermogenesis (hormones) IV. Nausea , Vomiting A. Anorexia 1. Factors affecting appetite a. Hunger b. Hypothalmus regulation c. Smell, fear, depression, anxiety d. Drugs B. Nausea 1. Stimulation 2. Causes a. Anorexia b. Food/Drugs c. Duodenum distention 3. ANS manifestation a. Saliva b. Vasoconstriction C. Vomiting – reverse peristalsis 1. Preceeded by nausea 2. Protection 3. Function/process 17 a. Vomiting center 1) Chemoreceptor trigger zone – medulla & stimulated by release serotonin in neurons & GI mucosa 2) Anti-vomiting drugs (Zofran, Compazine, Phenergan, Reglan) block serotonin receptors in chemoreceptor trigger zone b. Chemo receptor Proper dietary intake is essential for proper body function. Also, a healthy GI tract is also important to get those nutrients where they are needed most for proper cellular function!!!!!!!!!!!!!