Learning Supplement:
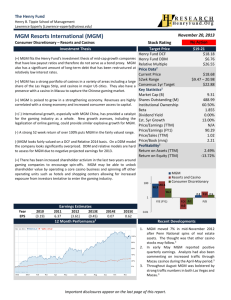
advertisement
Antipsychotic Medications 1. Antipsychotic Medications A. Typical - the “old” ones primarily block dopamine from the receptors and have serious side effects. They only effect the “positive symptoms” of schizophrenia. B. Atypical – the “new” medications effect dopamine and serotonin. Also, they have a much better side effect profile and decrease the “positive” and “negative” symptoms. They are very expensive. 2. Typical antipsychotics: A. High Potency - 1 to 20 mgm-High EPS, low anticholinergic side effects 1. Haldol (haloperidol) 2. Prolixin (fluphenazine): both these meds come in PO, IM and Depot IM B. In-betweens - 4-20 mgm 1. Stelazine (trifluoperazine) 2. Trilaphon (perphenazine) 3. Navane (thiothixene) 4. Loxitane (loxapine) 5. Moban (molindone) C. Low Potency - 50 to 1000 mgm 1. Thorazine (chlorpromazine) 2. Mellaril (thioridazine) 3. Serentil (mesoridazine) 3. Atypical Antipsychotics: less EPS side effects, decrease BOTH positive and negative symptoms A. B. C. D. E. F. Clozaril - 300 mgm (clozapine) Risperdal - 6-12 mgm (risperidone) Zyprexa - 10 mgm (olanzapine) Seroquel - .150-300 mgm (quetiapine) Geodon – 20- 80 mem BID (ziprasidone) Abilify (Aripiprazole) 4. Antiparkinsonian Agents A. B. C. D. Cogentin 1-2 mgm (benztropine) Artane 1-2 mgm (trihexyphenidyl) Benadryl 50 mgm (diphenhydramine) Symmetrel 100 mgm (amantidine) 5. Side Effects of Typical Antipsychotics A. Drowsiness: common during the first few days of treatment; usually disappears in one to two weeks. Clients should avoid alcohol and medications such as antihistamines and sleeping aids. B. Extrapyramidal side affects (EPS): 1. Dystonias: usually occur during the first 5 days of treatment, almost never after the first 3 months of treatment. They can occur after each injection of IM medication. Risk factors include high potency agents, large doses, and parental (IM or IV) route of administration. These affects are readily reversible with intramuscular injections of diphenhydramine (Benadryl), or benztropine (Cogentin). Oral antiparkinson agents may need to be continued for a few weeks to prevent recurrence of the reaction. Clients will often times refer to these reactions as “drug allergies” or “seizures”. These however are not allergic or epileptogenic in nature, and do not preclude continued use of the agent. These reactions include spasms of the: eye-oculogyric crisis neck-torticollis back-retrocollis/opisthotonus tongue-glossospasm or other muscles 2. Pseudoparkinsonism: Due to an imbalance of acetylcholine and dopamine in the basal ganglia, similar to idiopathic Parkinson’s disease except in pseudoparkinsonism this effect is reversible. Treatment consists of reducing the dose, changing to a different agent, or using oral antiparkinson agents such as benztropine (Cogentin), trihexyphenidyl (Artane), diphenhydramine (Benadryl), biperiden (Akineton), or amantidine (Symmetrel). Symptoms include: decrease movements (bradykinesia, akinesia), muscle rigidity (cogwheel and lead pipe), resting hand tremor, drooling, mask-like face, and shuffling gait. 3. Akathisia: can’t remain still, constantly pacing. Clients may describe this effect as a feeling of inner restlessness. This effect can easily be confused with anxiety and agitation. Differences between akathisia and anxiety/agitation improves with increases in antipsychotic doses, and vice-versa; and the client can usually control anxiety/agitation for a period of time whereas the client cannot typically control akathisia. This effect can be treated by changing to a different agent, reducing the dose if possible, or by the use of an antiparkinson agent or benzodiazepine. 4. Tardive Dyskinesia: symptoms consist of involuntary lip and tongue movements, and writhing movements (choreoathetoid) of the arms and legs. Movements disappear during sleep. Risk factors include increased age, long duration of therapy, use of high potency agents, and large doses. There is no effective treatment for tardive dyskinesia. Reducing the dose of the antipsychotic agent and addition of an antiparkinson agent result in worsening of the symptoms. C. Anticholinergic side affects: tolerance usually develops to these side affects over 1-2 months. – dry month - use of ice chips, sugarless gum, or sugarless sour candy may be helpful – blurred vision - reading in well lighted areas and varying the distance of the material being read may be helpful – constipation - exercise, drinking plenty of fluids daily, and increasing the amount of bulk food (bran, salads) intake may relieve this effect. Chronic problems may require short term use of topical nasal decongestant. – increase in heart rate – ejaculation inhibition - most common with mellaril D. Cardiovascular side effects: most common with low potency agents. – postural hypotension (dizziness or fainting) - commonly occurs with sudden changes in position e.g. laying or sitting to standing position, or in hot temperatures such as hot showers, saunas, and summer heat. Clients should be told to change positions slowly, and use good judgement in extreme heat. – arrhythmias/palpitations (changes in heart rhythm) E. Miscellaneous side effects: – skin rash: usually 2 to 8 weeks after initiation of treatment – photosensitivity: severe sunburn, most common with Thorazine. Clients should be instructed to wear hats, and long sleeve clothing until the effects from the sun are determined for that client. A sunscreen is also useful. A Sun Protection Factor (SPF) number 15 sunscreen is best. Good choices are Presun 15, and Solbar 15 plus. Rare side effects – Neuroleptic Malignant Syndrome – agranulocytosis – jaundice – lowered seizure threshold – galactorrhea, gynecomastia – menstrual irregulations – body temperature alterations – pigmentary retinopathy – increase in blood sugar – weight gain Neuroleptic Malignant Syndrome 1. Predisposing factors; Youth, male; High-potency neuroleptic, client who is pharmacologically naïve. 2. Four Cardinal Symptoms a. Febrility: usually the first symptom b. Lead pipe rigidity c. Automatic instability; tachycardia d. LOC Changes Lab results will include elevated CPK 3. Medical emergency; DC all meds. May resume meds after crisis. Syndrome is very RARE. Resume medication with an atypical antipsychotic after CPK has returned to normal. Atypical Antipsychotic Medications A. Clozaril 1. Atypical antipsychotic 2. Decreases negative symptoms of schizophrenia 3. No Extrapyramidal symptoms (EPS) 4. May decrease symptoms of tardive dyskinesia 5. Affects both dopamine and serotonin 6. Side effects: drowsiness and drooling 7. Very costly $9,000 per year. 8. Side effects: a. Agranulocytosis, weekly blood draws b. Sedation, excessive salivation, dizziness, seizures c. Hyperglycemia/weight gain, NIDDM B. Risperidone 1. Medication is costly - $400 for 1 month supply 2. Atypical; effects serotonin and dopamine 3. 1st line; affects both positive and negative symptoms 4. Can cause EPS, but lower incidence 5. Side effects: CNS insomnia, drowsiness (most common), agitation, headache, anxiety – Orthostatic hypotension – Hyperglycemia 6. GI: constipation, nausea, vomiting and dyspepsia 7. High potency - 8 mgm per day in 2 doses 8. Available in long lasting IM form (2 weeks) C. Olanzapine / Zyprexa 1. 1st line drug: Positive and negative symptoms 2. High potency: 10 mgm a day - up to 20 3. 4. 5. 6. 7. Side effects: Drowsiness, constipation, dry mouth, headache. Rare EPS, NMS Affects both serotonin and dopamine Weight gain long term/Hyperglycemia/NIDDM Drug is costly - 10 mgm per day for 30 days is $250 Available in short acting IM form D. Seroquel (Quetiapine) 1. Atypical antipsychotic, low potency 2. Effective for positive and negative symptoms 3. EPS profile same as placebo 4. No increase in prolactin levels 5. Sexual dysfunction problems are rare 6. Side effects: somnolence and hypotension 7. Doses: effective at 150 mgm to 750 mgm per day 8. Average: 300 mgm; 100 in AM-200 in PM 9. Titrate doses: begin at 50 mgm per day E. Ziprasidone 1. Geodon/Atypical Antipsychotic – Antagonizes Dopamine and Serotonin 2. Low EPS 3. No increase in prolactin levels 4. Side effects: somnolence in short term and insomnia in long term use 5. Weight gain neutral 6. Big issue: prolongs the QT interval 7. Contraindiciated for clients with cardiac pathology or prone to electrolyte imbalance 8. Monitor serum potassium and magnesium 9. Starting dose of 80 mgm per day in 2 doses 10. Can go to 160 mgm 11. Available in short acting IM form F. Aripiprazole / Abilify 1. Atypical antipsychotic, affects both dopamine and serotonin, antagonizing some receptors and serving as a partial agonist for others 2. Decrease in the EPS side effects and minimal weight gain, minimal sedation, no problems with QT interval 3. Side effects: headache, anxiety, insomnia, somnolence, occasional stomach upset 4. Dosage: 10 to 15 mgm daily can go up to 30