Introduction to Psychopharmacology
advertisement
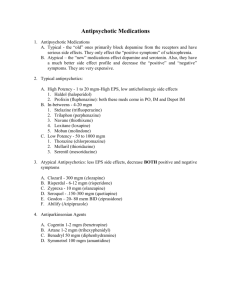
INTRODUCTION TO PSYCHOPHARMACOLOGY CHARLES P. SAMENOW, MD, MPH OBJECTIVES • Identify major classes of somatic treatments for the major DSM-IV-TR Diagnoses • Describe basic mechanism of action of somatic treatments • Explain how mechanism of action related to major side effect profiles ANTIDEPRESSANTS TRICYCLIC ANTIDEPRESSANTS • Block the re-uptake of three neurotransmitter systems: • Serotonin • Norepinephrine • Dopamine • Utilized in: • • • • • Major Depressive Disorder Dysthymia Generalized Anxiety Disorder Panic Disorder Obsessive-Compulsive Disorder TRICYCLIC ANTIDEPESSANTS • Older “Dirtier” Medication: • 3-4 weeks for onset (sometimes even 4-6 weeks) • Can be lethal in overdose (cardiotoxic) • Have side effect profiles: • Anticholinergic: dry mouth, constipation, confusion, urinary retention • Histaminic blockade: sedation and weight gain • Alpha-adrengergic blockade: orthostatic hypotention • Serotinergic: sexual side effect MAOI • Block Monoamine Oxidase in the wall of the gut, CNS and platelets leading to build up of Dopamine and Norepinephrine • Utilized in: • Major Depressive Disorder • Atypical Depression • Anxiety Disorders MAOI • Inhibition of MAO in the gut leads to increased Tyramine absorption. Hence, patients must avoid Tyramine containing foods (fava beans, aged meats and cheeses, wines, sauerkraut, etc…) • Ingestion of Tyramine can lead to hypertensive crisis • Require 3-4 weeks (sometimes 6-8 weeks) • Fatal in overdose • Cannot be combined with other serotinergic acting drugs (Tricyclic’s, SSRI’s) due to risk of serotonin syndrome. • Overdose can be fatal SSRI • Blockade of serotonin reuptake from the synapse • Utilized in: • • • • • • • • Major Depression Dysthymia OCD Panic Disorder PTSD Social Phobia Bulimia Nervosa Depressed phase of Bipolar (only with a mood stabilizer) SSRI • Take 2-4 weeks for onset • Fewer side effects than older medications – “Cleaner” and more easily tolerated • First line agents in pregnancy (although Class C) • Major side effects: • • • • • Gastrointestinal (first few days) Sexual Side Effects Black Box Warning: Increased Suicidality in Adolescents Treatment emergent mania in bipolar disorder Discontinuation Syndrome SNRI • Blocks Re-uptake of Serotonin and Norepinephrine • Careful balance between two neurotransmitter systems • Utilized in Depression, Anxiety and Pain Syndromes • “Cleaner”/More Easily Tolerated • Major Side Effects: • Blood Pressure • Discontinuation Syndrome MISCELLANEOUS • Wellbutrin (Buproprion) Inhibition of Norepinephrine Re-uptake No sexual side effects Also marketed as Zyban for smoking cessation Contraindicated in eating disorders due to lowering seizure threshold • Main side effect is anxiety • • • • • Remeron (Mirtazapine) • Alpha-2 Antagonist (net effect -> increased norepinephrine) • May cause sedation or increased weight gain • Often used in the elderly SEDATIVES/ANXIOLYTICS BENZODIAZAPINES • Use is determined by ½ life: • Long (Diazepam, Chlorediazepoxide) • Medium (Alprazolam) • Short (Lorazepam) • Utilized for panic and insomnia • Potentiation of GABA receptors by binding to special binding site • Long-term use may lead to tolerance, withdrawal and physiologic dependence • Side effects are sedation and amnesia OTHERS • Beta-Blockers – • Utilized for performance anxiety • Centrally acting/lipophilic propranolol ANTIPSYCHOTICS TYPICAL ANTIPSYCHOTICS • High Potency (Haldol) • • • • Primary action is blocking D2 receptors (antagonist) High affinity for D2 = lower dose Good control of positive symptoms Major Side Effects: • EPS -dystonic reactions, prolactin, akasthesia, parkinsonism • Neuroleptic Malignant Syndrome – • Mid/Low Potency (Thorazine) • Lower affinity for D2 = higher dose • Less EPS • More anticholinergic, alpha-adreinergic, and histiminic side effects DOPAMINE HYPOTHESIS OF SCHIZOPHRENIA Mesocortical pathway Hypoactivity: negative, cognitive, and mood symptoms Tuberoinfundibular pathway (inhibits prolactin release [D2]) Nigrostriatal pathway (part of EP system) Mesolimbic pathway Hyperactivity: positive symptoms (hallucinations, delusions) Clinical profile: Dopamine (D2) blockade Mesolimbic D2 EFFICACY: (+) SSX MesocorticalD2 INEFFICACY: (-) SSX, cognition, mood Nigrostriatal D2 SIDE EFFECTS: EPS D2 Tuberoinfundibular SIDE EFFECTS: HPL SCHIZOPHRENIA (TREATMENT) HIGH Fluphenazine (D) Trifluoperazine Thiothixine Haloperidol (D) MEDIUM Perphenazine Prochlorperazine Loxapine Acetophenazine Triflupromazine Chlorprothixine Mesoridazine LOW Thioridazine Chlorpromazine EPS, HPL EPS, HPL Anti-H1: Sedation, wt gain Anti-H1 Anti-α-1: Orthostasis, reflex tachycardia Anti-α-1 Anti-M1: Blurry vision, dry mouth, constipation, urinary retention, tachycardia, memory problems or delirium in susceptible patients Anti-M1 Seizure, arrythmias, retinitis, skin discoloration, photosens EPS • Dystonia – acute, involuntary muscle spasms often seen in ocular muscles and neck • Parkinsonism – tremor, cogwheel rigidity, masked facies, and shuffling gait • Akasthesia – a subjective sense of restlessness. • Tardive Dyskinesia – long-term involuntary jerking of face, neck, trunk or extremities. May be permanent. http://www.youtube.com/watch?v=R0EbgpyztCA ATYPICAL (SECOND GENERATION) • Utilized in: • • • • • Acute Schizophrenia Maintenance of Schizophrenia Acute Mania Maintenance of Bipolar Treatment of Bipolar Depression • Mechanism of Action: Blockade of D2 and 5HT-2A. Serotonin modulate dopamine, particularly in the nigrostriatal pathways. Hence, more Dopamine blockade in the mesolimbic as opposed to nigrostriatal pathways. A. 5HT B. DA C. 5HT DA release D. DA +/- DA release ATYPICALS • • • • • • Often first line Efficacy on positive and negative symptoms NMS and EPS unlikely Side Effects are based on receptor profile Prolongation of QTc (Cardiovascular) Metabolic Syndrome • Weight Gain • Glucose Intolerance • Increased Lipids and Triglycerides MOOD STABILIZERS LITHIUM • Indicated for acute mania and maintenance bipolar • Specific evidence to support use in preventing suicide • Blocks inositol-1-phosphatase • Narrow therapeutic range: dangerous in overdose • Side Effects: • • • • Tremor Renal Impairment Thyroid Dysfunction Cardiovascular ANTICONVULSANTS • Major Agents: Carbamazepine, Valproic Acid and Lamotrigene • May prevent kindling • Each agent has side effects that are outside scope of this lecture SUMMARY Disorder Treatment Depression SSRI, SNRI, Buproprion, Mirtazepine Atypical Depression MAOI Anxiety Disorders Short-Term: Benzodiazepine Long-Term: SSRI, SNRI OCD High Dose SSRI, Tricyclics PTSD SSRI Performance Anxiety Beta-Blocker Psychosis Atypical Antipsychotic Acute Mania Atypical Antipsychotic, Lithium, Carbamazepine Bipolar Maintenance Atypical Antipsychotics, Lithium Carbamazepine Bipolar Depression Lamotrigine, Some Atypicals Rapid Cyclling/Mixed Episodes Valproic Acid