ACLS-Key-Points
advertisement
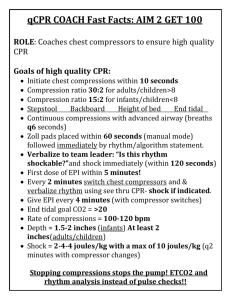
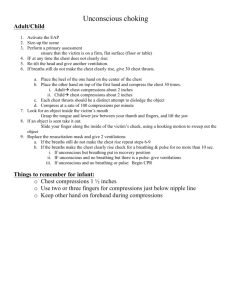
ACLS Key Points After having read and studied the new 2010 AHA ECC Guidelines for ACLS, I came up with some key ACLS points to share with you all. Looking forward to our upcoming ACLS class. It will be a good one!!= * Remember the key to good ACLS is good BLS. Compressions of at least 100 per minute. Quick defibrillation when indicated by AED or Manual. * Defib at 360 joules. * 12 lead EKG should be performed as soon as possible in patients with chest pain. Also patients with other cardiac involvement such as tachy or brady rates. Patients with an acute onset of abdominal pain. * M-O-N-A Morphine 2-6 mg titrate to effect. BP over 100. Oxygen, if the patient is dyspanic or sats are below 94.... chest pain is often symptom of hypoxia of the myocardium. Nitroglycerin administered sublingual again we need the patient to have a BP Systolic over 100. Aspirin 325 mg * We can deliver medications most effectively during an emergency through peripheral intravenous. * First drug in all cardiac arrest is Epinephrine. 1 mg in 1:10,000. Epi 1:1000 is used for asthma, bradycardia, pediatrics and allergic reaction. * A common fatal mistake of cardiac arrest management is prolonged interruptions in chest compressions. * Allow the chest to recoil completely when doing chest compressions. * Quantitative capnography in the intubated patient allows for the monitoring of CPR quality. * Once an advanced airway is in place continuous chest compressions should be performed at 100 per minute. * A rhythm without a pulse is Pulseless Electrical Activity. * The dose for Atropine in symptomatic Bradycardia is .5 mg. Atropine is not used in the cardiac arrest algorithm. * S/S of hemodynamic instability. Chest pain, dyspnea, acute pulmonary edema, hypotension, cool, clammy skin with other signs of shock. * What is the significance of at PETCO2 level of 8mm Hg in an intubated patient? * Hand free defib pads allow for more rapid defibrillation. * The dose for Amiodarone in refractory v-fib is 300 mg. * Don't forget vagal maneuvers on a stable tachy rhythms. * Dosage for Adenosine for stable narrow complex SVT is 6 given rapidly followed by a “NS bolus of 20ml; then raise the extremity...” * Review reasons to terminate attempts of resuscitative efforts. * Suction on the way out and not for longer than 10 seconds. * Stroke patients must go to facilities able to provide CT and other neurological services. * Care should be given not to hyperventilate or over inflate the lungs. As the intrathoraic pressure increases there can be adverse effects on the circulation to and from the lungs and from the heart to the peripherals. * General Assessment and Stabilization of the Stroke Patient: * Assess and support the ABC’s * Establish IV Access and draw labs * Check glucose * Perform neurologic assessment (Cincinnati Prehospital Stroke Scale) * Cat scan w/o contrast needs to be performed. * When a Supra ventricular rhythm is unstable synchronized cardioversion is required. * I know I said it before and will say it again, compress and allow full chest rise. * Treat Hypotension (SBP <90 mm Hg) with * IV Bolus 1-2 liters of normal saline or lactated Ringers. Fluids cooled to 4 degrees celsius maybe used * Epi 0.1-0.5 mcg/kg per minute IV infusion to achieve and maintain a SBP>90 mm Hg * Dopamine 5-10 mcg/kg per minute IV infusion titrate to a min SBP >90 mm Hg * Norepinephrine .... open for discussion.