Nov 11 - Genesee County Medical Control Authority
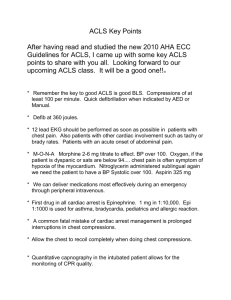
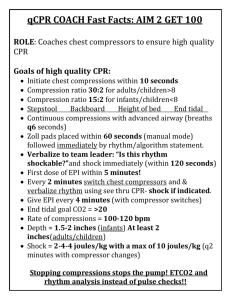
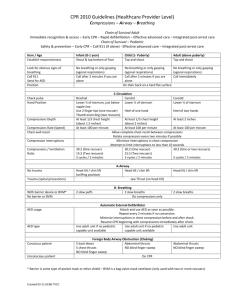
advertisement

The Genesee County Medical Control Authority’s Newsletter for EMS Providers - Also now available on line at GCMCA.org 3927 Beecher Rd Flint 48532 Office Phone 766-8898 12 lead Test for Paramedics and coming mandatory training As we moved into transmitting 12 Lead EKG’s to the hospitals when there was: A. ST” elevation ≥ 1mm in 2 contiguous leads B. Chest pain patient with left bundle branch block C. EMS personnel request assistance by hospital for interpretation of ECG D. Hospital requests ECG be sent. we found that there were a number of barriers to the hospitals receiving them. The transmission’s purpose was to allow the hospital to activate their cath lab as soon as possible. Given the problems in transmitting them the question was raised, could paramedics read the 12 lead findings accurately enough that they could know to activate the hospital’s cath lab from the field? National statistics indicated that paramedics spotted STEMI and ST elevations with the same accuracy as ED staff did. There was only one way to find out and that was to test our paramedics’ competency. A test for reading 12 lead EKGs has been developed by the Education Committee. Dr. Michael Jule and Dominic Foster gathered 32 12 lead strips that cover the primary 18 types of findings. Forty paramedics were chosen at random to take the test. The Board of the GCMCA has mandated that all paramedics who want to work in the county must take a GCMCA sponsored 12 lead education program. More information will be coming on the dates for this course in the near future. Even if a paramedic has recently taken a 12 lead course, all paramedics will be required to take this course. November 2011 Keeping Track of CE Credits It should go without saying, but it is worth saying anyway. It is your responsibility to keep track of Continuing Education credits. This is especially true for when you take trainings outside of your agency. The state does do audits of CE’s and will revoke the license of personnel who cannot show that they have taken the required number of credits. It is a good idea to keep records on all of your CE’s for up to six years. Just a friendly reminder. Changes to Protocols After a very long process, there are now standardized treatment protocols that are in place for all MCAs in the state. There are some variations from one MCA to another. So, especially if you are new to Genesee County make sure you familiarize yourself with them. The protocols can be accessed through our website, gcmca.org. New Pocket Protocol Book Available Soon There have been many people asking if there is a new pocket protocol book out yet. By the time you read this there will be!! Many agencies are giving them out for no charge to their employees. We will have a number of copies available for $5.00. There is also an app for the iPhone that can be obtained through the Apple App Store or at http://www.acidremap.com the web site of the app creator. New ACLS Guidelines now in Protocol On October 1, 2011, the new ACLS guidelines went into effect for our county. Every five years, the American Heart Association evaluates available research and reviews existing first aid and life support guidelines. The goal? To determine if changes need to be made to improve the effectiveness of lifesaving procedures such as advanced cardiac life support (ACLS), pediatric advanced life support (PALS), basic life support (BLS) and cardiopulmonary resuscitation (CPR). New ACLS guidelines were announced in late 2010, and Health Education Solutions will reflect the new recommendations to ACLS and PALS courses by January 2011. Michael Huckabee, PhD, PA-C, director of the Union College Physician Assistant program and curriculum developer for Health Education Solutions, offers this overview of the updates to ACLS standards: A-B-C to C-A-B The A-B-C approach (Airway-Breathing-Circulation) has been changed to the C-A-B approach (CirculationAirway-Breathing). The emphasis is on quickly initiating chest compressions in individuals with life-threatening loss of heart function so that blood flow is maintained. It primarily applies to CPR performed by a single rescuer. In the hospital setting and with teams, management of circulation and respirations are achieved simultaneously. Chest compression changes The chest compressions should depress the adult sternum at least 2 inches, rather than the previous recommendation of 1 ½ to 2 inches, and complete recoil of the chest is required. The chest compressions should be performed at a rate of at least 100 per minute, rather than the previous recommendation of about 100 per minute, to maximize critical blood flow. Checking for a pulse in an unresponsive individual should now require less than 10 seconds so that chest compressions aren't delayed. Mistakenly doing chest compressions on someone with a pulse does little harm compared to not doing compressions on someone without a pulse. Quantitative Waveform Capnography recommendation Use of quantitative waveform capnography is recommended for confirmation and monitoring of endotracheal tube placement. The continuous measurement provides the partial pressure of exhaled carbon dioxide in mm Hg over time. Individuals requiring endotracheal intubation are at risk of tube displacement during transport and transfer and the continuous waveform capnography reflects any changes. The capnography also provides a monitor of effective chest compressions. The return of spontaneous circulation is sometimes difficult to assess and is clearly demonstrated on the capnography measure by an abrupt increase in the CO2 readings. New medication protocols Four new medication protocols are recommended. One, atropine is no longer recommended for routine use in the management of pulseless electrical activity (PEA) or asystole, due to a lack of any observed therapeutic benefit. Two, adenosine is recommended for the treatment of stable, undifferentiated wide-complex tachycardia when the rhythm is regular and the QRS waveform is monomorphic. Three, intravenous chronotropic agents are recommended as an effective alternative to external pacing for individuals with symptomatic or unstable bradycardia. Finally, oxygen supplementation for uncomplicated acute coronary syndromes is no longer routinely indicated and should only be applied if the oxyhemoglobin saturation is less than or equal to 94 percent. Emergency care priorities To avoid interruptions to chest compressions or delays in use of defibrillators, the use of advanced airways, gaining vascular access and administering drugs doesn't take priority over high quality CPR and access to immediate defibrillation. Post-cardiac arrest care A new section was created for Post-Cardiac Arrest Care, emphasizing a structured interdisciplinary system of care following a cardiac arrest. Therapeutic hypothermia treatment and percutaneous coronary interventions, such as coronary angiography with revascularization, should be provided when indicated after cardiac arrest. Genesee County Sheriff Department Has Lucas Device. The Sheriff’s paramedics have purchased the automated chest compression device know as the Lucas Device. Only one paramedic carries it, but it is known to be a highly effective means of delivering quality CPR compressions. The LUCAS device is an electric powered device that automates the chest compression part of CPR. The great benefit of this device is it never tires. Even the most well trained EMT’s can become tired administering CPR and that can unfortunately lead to death. The LUCAS device automatically delivers 100 chest compressions per minute or two 2 compressions per second consistently. The consistent compressions of the LUCAS device along with the use of an AED will help the heart start beating in a regular rhythm. By automating the compressions free up the caretakers hands to help the patient in other aspects such as giving the patient medication or getting the patient ready for transport.