Dermal fillers should be regarded as prescription-only
advertisement
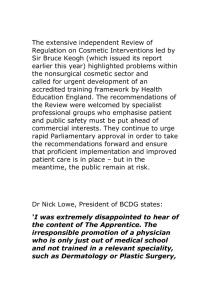
NEW RECOMMENDATIONS TO PROTECT PEOPLE WHO CHOOSE COSMETIC SURGERY The independent review into cosmetic interventions, today sets out how it would like to see the sector better regulated, practitioners better trained and people having proper redress if things go wrong. The key elements the review group feel would contribute to a successful and safe industry include: making all dermal fillers prescription only; ensuring all practitioners are properly qualified for all the procedures they offer. This needs to include all people from cosmetic surgeons offering breast enlargement through to people offering injectables such as dermal fillers or Botox®; an ombudsman to oversee all private health care including cosmetic procedures to assist those who have been treated poorly. The review, led by NHS Medical Director, Professor Sir Bruce Keogh, has been looking at how to protecting patients and tackle unsafe practices in an industry believed to be worth £2.3 billion a year. Commissioned by the Government following the PIP breast implant scandal, the review has looked at the products used for surgical and non-surgical procedures, the people who administer them, the way they are advertised and the advice and support patients and consumers are given. It has found that, despite the popularity of non-surgical procedures like Botox®, dermal fillers or laser hair removal – which account for nine out of ten procedures in the UK – there is almost no regulation. This is despite the fact that they can have major, permanent effects on people’s health and wellbeing. The committee was determined that the production of dermal fillers should fall under the same controls as other implants as this will ensure that only those fillers have passed vigorous appraisals of safety will be available, and only those with appropriate skill will be able to administer them Other key recommendations are: surgical providers should provide a record of implants and operations to both the person undergoing a procedure and their GP; a registry should be established for breast implants and other devices, this should alert the authorities to any signs of concerns at an early stage, and will provide critical intelligence in the event of product failure or recall; obtaining consent should not be dismissed as a casual irrelevance, providers are obliged to ensure that people are aware of the implications and risks of procedure and that they have adequate time to consider this information before proceeding with surgery; an advertising code of conduct should be developed and compliance should be mandatory for all practitioners; and insurance products should be developed to protect patients in the event of product failure, or provider insolvency. Review chairman Professor Sir Bruce Keogh said: “At the heart of this report is the person who chooses to have a cosmetic procedure. We have heard terrible reports about people who have trusted a cosmetic practitioner to help them but, when things have gone wrong, they have been left high and dry with no help. These people have not had the safety net that those using the NHS have. This needs to change. “We would like to see everyone who chooses to have any cosmetic procedure better protected. We would like to see people who carry out procedures trained to a high standard. We would like the public to feel confident they are going to be well looked after and, if things go wrong, that they will be supported. And ultimately, if someone needs to step in on the side of patients, we think there should be an ombudsman to do that. “This isn’t just about the past and present, this is about protecting people for years to come. We very much hope that our report will lead to a safer environment for patients and this industry in the future.” The review has assessed the current rules in England for: Products or devices used in cosmetic interventions, e.g. breast implants or dermal fillers Practitioners of cosmetic interventions, be they health professionals or non-health professionals Providers, be they large providers or small high-street beauty clinics Procedure that range from surgical operations to non surgical treatments Insurance and indemnity requirements Patient information and consent The advertising and marketing of cosmetic interventions The review was commissioned by ministers following the PiP breast implant scandal, which exposed significant lapses in product quality, after care and record keeping. It also drew attention to widespread use of misleading advertising, inappropriate marketing and unsafe practices across the sector. Background A full copy of the report will be available from 00.01 hours on 24 April at www.gov.uk/xxx The Review Committee members were: • Professor Sir Bruce Keogh, (Chair), NHS Medical Director • Doctor Andrew Vallance-Owen, former Group Medical Director of BUPA • Catherine Kydd, campaigner on PIP implants • Professor Sir Ian Kennedy, Emeritus Professor of Health Law, Ethics and Policy at University College London • Trish Halpin, Editor of Marie-Claire magazine • Dr Rosemary Leonard, GP and media doctor • Professor Shirley Pearce, clinical psychologist and former Vice Chancellor of Loughborough University • Mr Simon Withey, plastic surgeon • Vivienne Parry, writer and broadcaster For more information, contact Department of Health Press Office on 0207 210 5472 / 5504 / 5896.