Finding a Way to Treat Cisplatin and Multiple Drug Resistant Cancers
advertisement

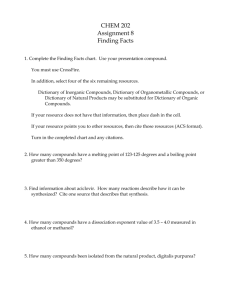
Finding a Way to Treat Cisplatin and Multiple Drug Resistant Cancers Shelly Jozwiak The objective of this research was to determine if any of the new platinum and palladium compounds synthesized by the Dr. Granger research team would kill cancer cells that are resistant to cisplatin or multiple drugs in addition to killing cells that are not resistant. Background Cancer remains an elusive disease for doctors in many cases and a scary diagnosis for patients. One reason cancer is difficult to treat is that each type of cancer is different; even the same type of cancer can vary from person to person in its cellular characteristics. Two characteristics shared by all cancers are uncontrolled growth and invasiveness to other parts of the body. Cancer is typically treated with surgery, radiation, chemotherapy, immunotherapy, and/or gene therapy. While surgery and radiation are ideally used for isolated tumors whose cells have not spread throughout the body, cancer that has spread into other parts of the body is usually treated with one or more of the other three options. One widely used chemotherapeutic agent is cisplatin, especially for testicular, bladder, germ cell, head and neck, small cell lung cancer, and ovarian cancer. Ovarian cancer is one of the four leading causes of death among women in the United States. Over 80 percent of patients with ovarian cancer relapse after the first treatment, and a majority of these develop resistance to the chemotherapy. Five year survival rates for women diagnosed with this type of cancer for stages I, II, III, and IV are 74, 58, 30, and 19 percent, respectively. This would not be bad except for the fact that 74 percent of women with ovarian cancer are diagnosed in stages III and IV. The initial response rates to chemotherapy (usually cisplatin-based) are high; cisplatin resistance is the reason for the low survival rates. It is the limiting factor in chemotherapy treatment of ovarian cancer. 50 percent of all ovarian cancers are intrinsically resistant to cisplatin (having never been treated), so a woman diagnosed with ovarian cancer has a 50 percent chance of even responding to the chemotherapy. Resistance Resistance occurs when, due to certain cell mechanisms, the cells are not affected by a particular drug/substance. There are three different types of resistance: intrinsic, acquired, and cross-resistance. Intrinsic resistance occurs when the cells are not affected by the drug the very first time they come in contact with it. Acquired resistance occurs after repeated treatments with a drug; a few resistant cells that are not killed by the first few treatments grow and multiply until most of the cell population is now resistant. Cross resistance occurs when cells that are resistant to one drug are also resistant to another drug, usually by some similarity between the drugs. How does a cell “resist” cisplatin? There are many ways: decreased intake, increased efflux (output), enhanced DNA repair of damage caused by cisplatin, and defective cell death pathways are some of the main mechanisms thought to account for resistance. However, it is still unknown how much each of these reasons is responsible; it does seem that there is usually a combination of two or more reasons. Current attempts to circumvent cisplatin resistance have not resulted in large increases in successful treatment. Treating the patients with compounds that reverse a certain resistance mechanism increase response rates but only a small amount; this is because resistance occurs by multiple mechanisms. The drugs used target only one specific mechanism, such as a protein or enzyme that is found in levels too high or not high enough. Combinations of drugs are also used that work more effectively together than alone. However, the increases in response rates do not rise satisfactorily high. Other drugs are constantly being tested, but none have been found yet that overcome all of the current problems with cisplatin. Goal and methods The goal of this research was to determine if any new platinum and palladium compounds were effective against cisplatin and multiple-drug resistant ovarian and uterine cancer cells. The cells used include two cisplatin resistant ovarian carcinomas (OVCAR-3 and SK-OV-3), two cisplatin resistant uterine sarcomas (MES-SA and its multi-drug resistant derivative MES-SA/Dx5), an untreated ovarian carcinoma (MDAH 2774), a radiation treated uterine sarcoma (SK-UT-1), and a non-cancerous uterine line (NUT). The compounds used were those synthesized by Dr. R. Granger and his research team of the Sweet Briar College chemistry department. These compounds were first synthesized in 1996 by Dr. Granger and previously believed to be impossible to make. Therefore, research involving these as possible anti-cancer agents has been very limited. All of the compounds used in this particular study except for one were palladium compounds. Cells were grown in culture flasks in an incubator. When there was a sufficient amount for an experiment, they were passed into well-plates, plastic plates with 96 small wells. They were allowed to sit for a day, and the compounds were then added to the wells for the cells to take up. Each well-plate had two controls, wells with untreated cells and wells with cells treated with dimethyl sulfoxide (DMSO), which is used to dissolve the compounds before adding them. After the addition of the compound, the cells were allowed to sit for two days. The MTT assay was then used to assess cell survival rates. Cell survival rates were measured on the basis of metabolic activity. A compound called MTT was added at the end of the experiment. Cells that were alive would taker the MTT up and metabolize it, and the dead cells would not. MTT in solution is yellow, but it is a blue precipitate when metabolized by these human cells. Therefore, wells with more living cells would have more blue precipitate than the wells with mostly dead cells. MTT was added, and then the growth medium solution was removed four hours later, leaving just the cells (adhered to the plastic) and metabolized MTT in the wells. DMSO was put in the wells, which served to break open and kill the cells while dissolving the MTT. The plates were then read in a microplate reader, which measured the absorbance of each well at 540 nanometers. This was based on the use of absorbance as a function of concentration—with higher metabolized MTT concentration, the absorbance is higher. Therefore, a relative determination of the survival rates of the cells (compared to the two controls) could be made. Results and Discussion After many weeks of testing (each experiment takes four days), results show that almost all of these compounds kill the resistant as well as the non-resistant cell lines. When compared with cisplatin, many of our compounds seem to be much more effective. MDAH 2774, ovarian carcinoma 120 100 Pd(dione)Cl4 Pt(dione)Cl4 Pd(phen)Cl4 Pd(phen)2Cl2 Pd(dione)2Cl2 Pd(dione)(bipy) Cisplatin Pd(dione)(phen) Pd(dppz)2 Pd(dione)Cl2` Pd(dppz)(phen) Percent survival 80 60 40 20 0 1 Compound A comparison of the compounds used against MDAH 2774, an untreated ovarian carcinoma line. Cisplatin was included in this study for comparison of effectiveness. Although MDAH 2774 was untreated, it turned out to be intrinsically resistant to cisplatin. Almost all of the compounds were more effective than cisplatin against all of the cancerous cell lines tested. Several compounds consistently resulted in survival rates of 20 percent or below against all of the cell lines. Others were obviously more effective than cisplatin as well, although not as effective against some cell lines as others. The normal cell line was included in this study for added information about how selective the compounds were against cancer cells vs. normal cells. The best outcome would have been low survival rates against cancer cells and high survival rates against normal cells. However, what we found most of the time was only a slight difference. A few of the compounds, though, showed more selectivity than the others. Cisplatin did not kill very many normal cells; it killed even less cancer cells, though. This proves, then, that in many cases, more normal cells are killed than cancer cells during treatment. There is more unknown about these specific compounds than there is known at this particular point concerning their actions in cells. Exactly how the compounds interact with the cells, in what way the cells are dying (accidental or programmed death), why they work better than cisplatin, and if acquired resistance could be a problem is still unknown. Further testing could shed some light on these questions. Overall, the results show what was hoped for; these compounds show potential for use as anti-cancer agents. However, this was only the first step. The next step involves submitting our testing results and compound structural information to the National Cancer Institute. They may then begin testing these compounds, first against a panel of three cell lines and then against 60 cell lines; if these tests are promising, clinical trials will then begin.