Multifocal Atrial Tachycardia
advertisement
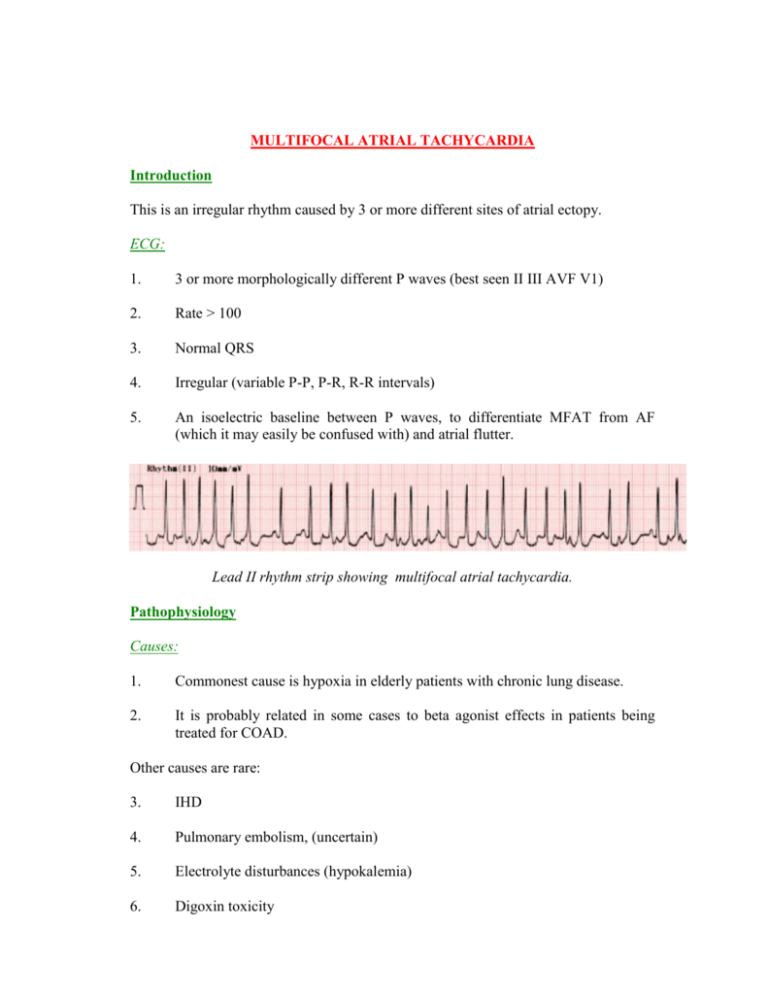
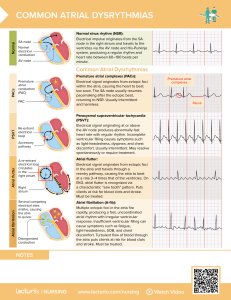
MULTIFOCAL ATRIAL TACHYCARDIA Introduction This is an irregular rhythm caused by 3 or more different sites of atrial ectopy. ECG: 1. 3 or more morphologically different P waves (best seen II III AVF V1) 2. Rate > 100 3. Normal QRS 4. Irregular (variable P-P, P-R, R-R intervals) 5. An isoelectric baseline between P waves, to differentiate MFAT from AF (which it may easily be confused with) and atrial flutter. Lead II rhythm strip showing multifocal atrial tachycardia. Pathophysiology Causes: 1. Commonest cause is hypoxia in elderly patients with chronic lung disease. 2. It is probably related in some cases to beta agonist effects in patients being treated for COAD. Other causes are rare: 3. IHD 4. Pulmonary embolism, (uncertain) 5. Electrolyte disturbances (hypokalemia) 6. Digoxin toxicity 7. In younger patients with underlying cardiac problem eg MVP. Clinical Features Of itself the arrhythmia is usually fairly benign. MFAT is usually a transient arrhythmia, which may spontaneously revert to sinus rhythm, AF or atrial flutter. Investigations These will be directed according to the index of suspicion for a particular cause. These may include: 1. FBE 2. CRP 3. U&Es/ glucose, (urgent potassium level) 4. Cardiac enzymes, (if an ACS is suspected). 5. Serum digoxin level 6. TFTs Management Specific treatment of this arrhythmia is rarely needed and is often not helpful. 1. Treatment should be aimed at the underlying disease process, most commonly exacerbation of COAD or attention to beta agonist therapy if this is thought to be a contributory factor. 2. Rate control may be attempted with: ● IV beta-blocker, esmolol infusion, because of its short half life, may be the best option as beta blockers are relatively contraindicated in COAD. ● IV MgSO4 ● IV verapamil (is probably the least effective treatment, however) Digoxin may cause increased mortality in patients with MFAT 3. Cardioversion is not effective. References: McCord J, Multifocal Atrial Tachycardia: Chest 1998: 113: 203-209. Dr J. Hayes Reviewed 8 December 2003