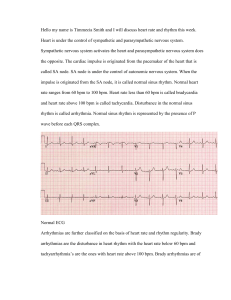
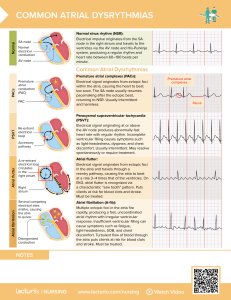
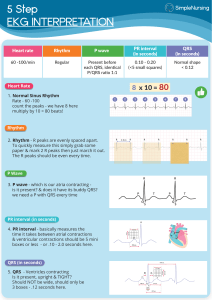
GEMECHIS Is a set of clinical interventions for the urgent treatment of cardiac arrest and other lifethreatening medical emergencies, as well as the knowledge and skill to deploy those skills. Adenosine Amiodarone Atropine Dopamine Epinephrine Lidocaine Magnesium sulfate Procainamide Sotalol 1 False regarding shock energy for defibrillation A biphasic initial dose 125-200J,if unkown use the maximaum dose B monophasic,360J C second or subsequent doses should be equal or higher D defib is indicated for PEA 2 Which one is a wrong statement? A shock refractory VF/pulselessVT refers to when the rhythm persists/recurs after 1 or more shocks B an anti-arrythmic alone is unlikely to pharmacologically convert VF/pulseless VT to an organizing perfusing rhythm C Amiodarone or lidocaine may be considered for VF/pulseless VT that is unresponsive to defibrillation D The routine use of magnesium for cardiac arrest is recommended in adult patients How about in covid19? 1. OXYGENATION AND VENTILATION Hypoxia during the early phase of reperfusion after ROSC harms post ischemic neurons and increases brain lipid peroxidation The suggested ventilator parameters during the post-ROSC phase are as follows: PaCO2 between 35 and 45 mm Hg (5 to 6 kPa); SaO2 between 94% and 98%; tidal volume between 6 and 8 mL/kg ideal body weight; PETCO2 between 35 and 40 mm Hg; and 10 to 12 ventilations per minute. HEMODYNAMIC MANAGEMENT Obtain 12-lead ECG after ROSC and repeat at 8 hours or as needed The target for blood pressure is a mean arterial pressure of 65 to 100 mm Hg. Brain cooling decreases cerebral oxygen demand, reduces cellular effects of reperfusion, and decreases the production of reactive oxide radicals. Targeted temperature management (cooling to 32 to 36°C goal is controversial) during the first 24 hours after ROSC improves survival and neurologic recovery GLYCEMIC CONTROL Maintain blood sugar levels between 100 and 180 milligrams/dL (6 and 10 mmol/L). NEUROLOGIC ASSESSMENT Features of brain injury after ROSC include coma, seizures, myoclonus, and various degrees of neurocognitive dysfunction ranging from memory deficits to a persistent vegetative state and finally brain death A 72 year old male patient Known IHD after CABG is in E-ICU with palpitations. Initial spo2 is 94% on room air &patient put on monitor. Go on managing the patient. What went well? What do you improve? Participant Audience Narrow Complex Regular Sinus Tachycardia SVT A flutter with 2:1 block Junctional tachycardia Irregular SVT Atrial fibrillation Atrial Fibrillation Atrial Flutter w variable block Multifocal Atrial Tachycardia Atrial flutter with variable block Wide Complex Regular Ventricular tachycardia Ventricular Tachycardia SVT with aberrancy Irregular Ventricular fibrillation Torsades de Pointe Torsades de Pointe Pre-excited Atrial fib. SVT with aberrancy A 52 year old lady known DM,HTN admitted to ED with severe chest discomfort and dizziness. Spo2 84% and BP=90/60 What went well? What do you need to improve? Participant? Audience? Six person Clear roles and responsibilities Closed loop communication Know your limitations Mutual respect Knowledge sharing The end!