Tissue: The Living Fabric- Chapter 4

Sexual Reproduction, Development and Tissues
Meiosis: gamete formation
-two nuclear divisions, meiosis I and meiosis II, half the number of chromosomes in the four daughter cells
Steps leading up to meiosis 1:
-all organelles are replicated during interphase
chromosomes replicate prior to meiosis I occurs during the S-phase of interphase
26
Steps of meiosis 1:
1) During prophase 1 ,
-the nuclear membranes break down
-the spindle forms
-the chromatin condenses
-homologous pairs of chromosomes undergo synapsis and form tetrads with their homologous partners
-crossover, the exchange of genetic material among tetrads, occurs during synapsis
2) Tetrads line up at the spindle equator during metaphase I
3) In anaphase I, homologous chromosomes still composed of joined sister chromatids are distributed to opposite ends of the cell
4) In telophase I :
-The nuclear membranes re-form around the chromosomal masses
- The spindle breaks down
-The chromatin reappears, forming two daughter cells
27
At the end of meiosis I each daughter cell has:
-Two copies of either a maternal or paternal chromosome
-A 2 n amount of DNA and haploid number of chromosomes
Meiosis II
Mirrors mitosis except that chromosomes are not replicated before it begins
Meiosis accomplishes two tasks:
-It reduces the chromosome number by half (2 n to n )
-It introduces genetic variability
Spermatogenesis
Cells making up the walls of seminiferous tubules are in various stages of cell division: these spermatogenic cells give rise to sperm in a series of events
1) Mitosis of spermatogonia, forming spermatocytes
2) Meiosis forms spermatids from spermatocytes
3) Spermiogenesis – spermatids form sperm
Mitosis of Spermatogonia
Spermatogonia – outermost cells in contact with the epithelial basal lamina
Spermatogenesis begins at puberty as each mitotic division of spermatogonia results in type A or type B daughter cells
-Type A cells remain at the basement membrane and maintain the germ line
-Type B cells move toward the lumen and become primary spermatocytes
28
Oogenesis
Production of female sex cells by meiosis
In the fetal period, oogonia (2 n ovarian stem cells) multiply by mitosis and store nutrients
Primordial follicles appear as oogonia are transformed into primary oocytes
Primary oocytes begin meiosis but stall in prophase I
Oogenesis: Puberty
At puberty, one activated primary oocyte produces two haploid cells
-The first polar body
-The secondary oocyte
The secondary oocyte arrests in metaphase II and is ovulated
If penetrated by sperm the second oocyte completes meiosis II, yielding:
-One large ovum (the functional gamete)
-A tiny second polar body
From Egg to Embryo
Pregnancy – events that occur from fertilization until the infant is born
Conceptus – the developing offspring
Gestation period – from the last menstrual period until birth
Preembryo – conceptus from fertilization until it is two weeks old
Embryo – conceptus during the third through the eighth week
Fetus – conceptus from the ninth week through birth
29
Accomplishing Fertilization
The oocyte is viable for 12 to 24 hours
Sperm is viable 24 to 72 hours
For fertilization to occur, coitus must occur no more than:
-Three days before ovulation
-24 hours after ovulation
Fertilization – when a sperm fuses with an egg to form a zygote
Preembryonic Development
The first cleavage produces two daughter cells called blastomeres
Morula – the 16 or more cell stage (72 hours old)
By the fourth or fifth day the preembryo consists of 100 or so cells (blastocyst)
Blastocyst – a fluid-filled hollow sphere composed of:
-A single layer of trophoblasts
-An inner cell mass
Implantation
Begins six to seven days after ovulation when the trophoblasts adhere to a properly prepared endometrium
Implantation is completed by the fourteenth day after ovulation
Viability of the corpus luteum is maintained by human chorionic gonadotropin (hCG)
secreted by the trophoblasts
hCG prompts the corpus luteum to continue to secrete progesterone and estrogen
Chorion – developed from trophoblasts after implantation, continues this hormonal stimulus
Between the second and third month, the placenta:
-Assumes the role of progesterone and estrogen production
-Is providing nutrients and removing wastes
30
Placentation
Formation of the placenta from:
-Embryonic trophoblastic tissues
-Maternal endometrial tissues
-fully formed and functional by the end of the third month
Germ Layers
The blastocyst develops into a gastrula with three primary germ layers: ectoderm, endoderm, and mesoderm
-these give rise to the basic tissues of the body
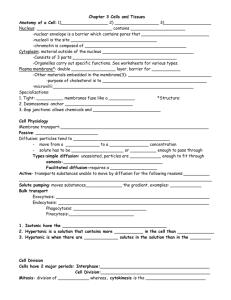
Tissues
Groups of cells similar in structure and function
The four types of tissues: Epithelial, Connective, Muscle, Nerve
Epithelial Tissue
Cellularity – composed almost entirely of cells
Special contacts – form continuous sheets held together by tight junctions and desmosomes
Polarity – apical and basal surfaces
Supported by connective tissue – reticular and basal laminae
Avascular but innervated – contains no blood vessels but supplied by nerve fibers
Regenerative – rapidly replaces lost cells by cell division
Classification of Epithelia
Simple or stratified- layering
Squamous, cuboidal, or columnar-cell shape
31
Epithelia: Simple Squamous
Single layer of flattened cells with disc-shaped nuclei and sparse cytoplasm
Functions:
-Diffusion and filtration
-Provide a slick, friction-reducing lining in lymphatic and cardiovascular systems
Epithelia: Simple Cuboidal
Single layer of cubelike cells with large, spherical central nuclei
Function in secretion and absorption
Epithelia: Simple Columnar
Single layer of tall cells with oval nuclei; many contain cilia
Goblet cells are often found in this layer
Function in absorption and secretion
Nonciliated type line digestive tract and gallbladder
Ciliated type line small bronchi, uterine tubes, and some regions of the uterus
Cilia help move substances through internal passageways
Epithelia: Pseudostratified Columnar
Single layer of cells with different heights; some do not reach the free surface
Nuclei are seen at different layers
Function in secretion and propulsion of mucus
Epithelia: Stratified Squamous
Thick membrane composed of several layers of cells
Function in protection of underlying areas subjected to abrasion
Forms the external part of the skin’s epidermis (keratinized cells), and linings of the esophagus, mouth, and vagina (nonkeratinized cells)
Stratified cuboidal
Quite rare in the body
Found in some sweat and mammary glands
Stratified columnar
Limited distribution in the body
Found in the pharynx, male urethra, and lining some glandular ducts
Transitional
Several cell layers, basal cells are cuboidal, surface cells are dome shaped
Stretches to permit the distension of the urinary bladder
Lines the urinary bladder, ureters, and part of the urethra
32
Epithelia: Glandular
A gland is one or more cells that makes and secretes an aqueous fluid
Classified by:
-Site of product release – endocrine or exocrine
-Relative number of cells forming the gland – unicellular or multicellular
Endocrine Glands
Ductless glands that produce hormones
Secretions include amino acids, proteins, glycoproteins, and steroids
Exocrine Glands
More numerous than endocrine glands
Secrete their products onto body surfaces (skin) or into body cavities
Examples include mucous, sweat, oil, and salivary glands
The only important unicellular gland is the goblet cell
Connective Tissue
Found throughout the body; most abundant and widely distributed in primary tissues
Connective tissue proper, cartilage, bone, and blood
Functions of Connective Tissue
Binding and support, protection, insulation, and transportation
33
Characteristics of Connective Tissue:
Mesenchyme as their common tissue of origin
Varying degrees of vascularity
Nonliving extracellular matrix, consisting of ground substance and fibers
Structural Elements of Connective Tissue
Ground substance – unstructured material that fills the space between cells
Fibers – collagen, elastic, or reticular
Cells – fibroblasts, chondroblasts, osteoblasts, and hematopoietic stem cells
Connective Tissue Proper: Loose
Areolar connective tissue
Gel-like matrix with all three connective tissue fibers
Fibroblasts, macrophages, mast cells, and some white blood cells
Wraps and cushions organs
Widely distributed throughout the body
Adipose connective tissue
Matrix similar to areolar connective tissue with closely packed adipocytes
Reserves food stores, insulates against heat loss, and supports and protects
Found under skin, around kidneys, within abdomen, and in breasts
Local fat deposits serve nutrient needs of highly active organs
Connective Tissue Proper: Dense
Regular
Parallel collagen fibers with a few elastic fibers
Major cell type is fibroblasts
Attaches muscles to bone or to other muscles, and bone to bone
Found in tendons, ligaments, and aponeuroses
34
Irregular
Irregularly arranged collagen fibers with some elastic fibers
Major cell type is fibroblasts
Withstands tension in many directions providing structural strength
Found in the dermis, submucosa of the digestive tract, and fibrous organ capsules
35
Connective Tissue: Cartilage
Hyaline Cartilage
Amorphous, firm matrix with imperceptible network of collagen fibers
Chondrocytes lie in lacunae
Supports, reinforces, cushions, and resists compression
Forms the costal cartilage
Found in embryonic skeleton, the end of long bones, nose, trachea, and larynx
Elastic Cartilage
Similar to hyaline cartilage but with more elastic fibers
Maintains shape and structure while allowing flexibility
Supports external ear (pinna) and the epiglottis
36
Fibrocartilage Cartilage
Matrix similar to hyaline cartilage but less firm with thick collagen fibers
Provides tensile strength and absorbs compression shock
Found in intervertebral discs, the pubic symphysis, and in discs of the knee joint
Connective Tissue: Bone (Osseous Tissue)
Hard, calcified matrix with collagen fibers found in bone
Osteocytes are found in lacunae and are well vascularized
Supports, protects, and provides levers for muscular action
Stores calcium, minerals, and fat
Marrow inside bones is the site of hematopoiesis
Connective Tissue: Blood
Red and white cells in a fluid matrix (plasma)
Contained within blood vessels
Functions in the transport of respiratory gases, nutrients, and wastes
Nervous Tissue
Branched neurons with long cellular processes and support cells
Transmits electrical signals from sensory receptors to effectors
Found in the brain, spinal cord, and peripheral nerves
37
Muscle Tissue
Skeletal
Long, cylindrical, multinucleate cells with obvious striations
Initiates and controls voluntary movement
Found in skeletal muscles that attach to bones or skin
Cardiac
Branching, striated, uninucleate cells interlocking at intercalated discs
Propels blood into the circulation
Found in the walls of the heart
38
Smooth
Sheets of spindle-shaped cells with central nuclei that have no striations
Propels substances along internal passageways (i.e., peristalsis)
Found in the walls of hollow organs
39