Calcific deposits
advertisement

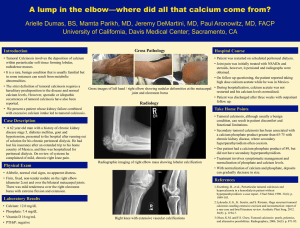
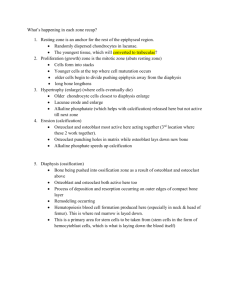
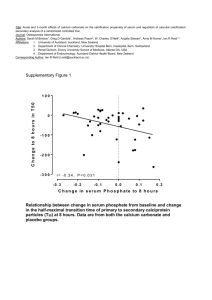
Calcinosis Cutis insoluble compounds of calcium are deposited within the skin due to local and/or systemic factor (mainly calcium hydroxyapatite or amorphous calcium phosphate Classification 1. Dystrophic calcification o calcium deposits in the soft tissues but have no generalized disturbance in calcium or phosphorus metabolism o often seen at sites of previous inflammation or damage to the skin or may occur in association with connective tissue disease, such as in systemic sclerosis (scleroderma) or polymyositis-dermatomyositis. o May go on to ossify – heterotrophic ossification o Causes (VINDICATE – surgical sieve): 1. Vascular – venous insufficiency 2. Infective – parasitic 3. Neoplasm o Pilomatrixoma, or calcifying epithelioma of Malherbe, is the most common tumor that becomes calcified. 4. Drugs – vitamin D 5. Iatrogenic 6. Congenital 7. Autoimmune – scleroderma 8. Trauma – burns, insect bites, injection granuloma 9. Ediopathic 2. Metastatic calcification o Calcification occurring as the result of systemic hypercalcemic or hyperphosphatemic states (renal failure, hyperparathyroidism, sarcoidosis, paraneoplastic syndrome) 3. Idiopathic - occurs in the absence of known tissue injury or systemic metabolic defect o Idiopathic calcinosis of scrotum, penis, or vulva: o Tumoral calcinosis: This may be caused by an error in renal phosphate metabolism resulting in hyperphosphatemia. General characteristics of the calcified nodules are a large size, a juxta-articular location, progressive enlargement, a tendency to recur after surgical removal, and the ability to encase the adjacent normal structures. o Calcinosis cutis circumscripta and calcinosis universalis: These forms are rare and may be due to altered ground substances. Calcinosis cutis circumscripta generally occurs earlier and tends to involve the extremities, whereas calcinosis universalis occurs later and is usually more widespread. o Transplant-associated calcinosis cutis 4. Iatrogenic o Parenteral administration of calcium or phosphate: o Tumor lysis syndrome o Repeated heel sticks in the newborn Investigations 1. Blood tests a. Ca, ALP, phosphate, albumin b. Urea/Cr c. Bicarbonate – milk-alkali syndrome in metabolic alkalosis d. SCL-70 in scleroderma (poor prognosis) 2. Xrays Treatment Nonsurgical 1. correct underlying problem 2. Intralesional corticosteroids may be beneficial because of their antiinflammatory and inhibitory effects on fibroblast activity. Surgical Indications for surgical removal 1. pain 2. recurrent infection 3. ulceration 4. Functional impairment. Because surgical trauma may stimulate calcification, initially treat a test site before pursuing a large excision. Recurrence is common after excision. Electric shock wave lithotripsy was successful in 1 case of dermatomyositisinduced tissue calcification. Calcium Pyrophosphate Deposition Disease arthritis caused by the deposition of calcium pyrophosphate crystals. Types 1. pseudogout 2. chondrocalcinosis - calcification within fibrous or hyaline cartilage structures Pathophysiology inflammatory cascade response to the deposition of calcium pyrophosphate crystals. Enzyme or saturation abnormalities allow the formation of excess pyrophosphate, which "salts out," especially in hyaline and fibrous cartilage. Individuals with CPDD may have more than 1 type of crystal present (eg, hydroxyapatite in addition to pyrophosphate). Heterotopic ossification defined as the formation of mature lamellar bone in soft tissues. The process involves true osteoblastic activity and bone formation 3 categories of HO have been described: 1. Myositis ossificans progressiva is a rare metabolic bone disease in children with progressive metamorphosis of skeletal muscle to bone and is characterized by an autosomal dominant pattern of genetic transmission. 2. Myositis ossificans circumscripta without trauma is a localized soft tissue ossification after neurologic injury or burns. This process also is referred to as neurogenic HO. 3. Traumatic myositis ossificans occurs from direct injury to the muscles. Fibrous, cartilaginous, and osseous tissues near bone are affected. The muscle may not be involved. Pathogenesis basic defect in HO is the inappropriate differentiation of fibroblasts to boneforming cells. Early edema of connective tissue proceeds to tissue with foci of calcification and then to maturation of calcification and ossification. Investigations Many clinicians rely on early detection of HO using triple-phase bone scan technology. Patient with dystrophic calcification in the Achilles tendon due to recurrent trauma and tendinitis. Patient with multiple "rice-grain" calcifications in muscles about knees due to cysticercosis 66 year old male with scleroderma, exhibiting acroosteolysis, skin atrophy over fingertips and calcinosis cutis. Heterotopic ossificiation after head injury Elderly female with tumoral calcinosis about hand and wrist. Beware primary bone forming tumor – like this osteosarcoma above






![2012 [1] Rajika L Dewasurendra, Prapat Suriyaphol, Sumadhya D](http://s3.studylib.net/store/data/006619083_1-f93216c6817d37213cca750ca3003423-300x300.png)