Package Insert for Unitized Sickle Cell Kit
advertisement

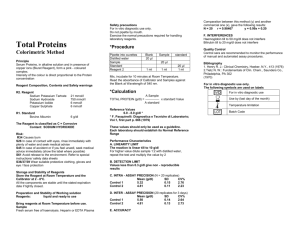
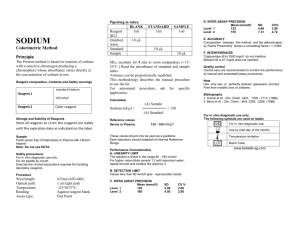
Cat. No. 2245 Sterling Diagnostics, Inc. For In Vitro Diagnostic Use Sterling Heights, MI 48312 U.S.A. SICKLE CELL UNI-TEST (Modified Nalbandian) INTENDED USE FOR IN VITRO DIAGNOSTIC USE in the qualitative determination of hemoglobin (HbS) in blood. CLINICAL SIGNIFICANCE (1-2) Sickle cell disease is an inherited disease characterized by the presence of an abnormal hemoglobin (HbS). In normal adults, 95% or more of the hemoglobin is hemoglobin A (HbS). Hemoglobin S can be inherited in the homozygous state (S/S), which results in sickle cell anemia, or in the heterozygous state (A/S), which is usually the benign, asymptomatic state (sickle cell trait). Hemoglobin S can also occur in the presence of other abnormal hemoglobins, i.e. HbC (S/C), thalasemia (Sthal), or HbD (S/D). These are referred to as the sickle cell variants and can produce symptoms of varying severity. About 8% of American blacks have a single HbS gene and 0.2% are homozygous for the gene. The HbS gene is essentially peculiar to Negroes, reaching a frequency of up to 59% in various regions of Africa. The HbS gene is also found in localized areas in countries bordering the Mediterranean Sea, e.g. Italy, Greece, Turkey, and some of the Arabic nations. About 2-3% of American blacks carry the hemoglobin C gene. The heterozygous state does not cause anemia or shortened red cell life span. But one in 6000 American blacks is homozygous for HbC. This causes a mild hemolytic anemia with striking morphologic abnormalities. TECHNICAL SUMMARY Erythrocytes are lysed by saponin and the released hemoglobin is deoxygenated by dithionite in a concentrated phosphate buffer (3). HbS, when deoxygenated, is insoluble in concentrated phosphate buffer and produces a visible turbidity. Since almost all other hemoglobins (i.e. Hb A, F, C, E, D) are soluble in the solution, blood specimens containing HbS are quickly identified. When a positive specimen is identified, the addition of urea to the reaction mixture will cause the solution to become clear if HbS is present. If the solution remains turbid after the urea addition, a non-S sickling hemoglobin is indicated. Electrophoretic confirmation is required for conclusive identification. The method presented here is based upon a modified Nalbandian (4-5) procedure. REAGENTS All of the following reagents can be used until the expiration date indicated on the individual bottles. STORE REAGENTS AT ROOM TEMPERATURE. 1. SICKLE CELL REAGENT: A solution containing phosphate buffer, saponin and preservative. Keep tightly capped and protect from contamination. Precautions: Sodium Dithionite (Hydrosulfite) is toxic! Wash hands after handling. If ingested seek immediate attention. Do Not Pipet by Mouth. For other reagents in this set, exercise the normal precautions required for the handling of all laboratory reagents. INDICATORS OF REAGENT DETERIORATION 1. Physical Appearance a. Any cloudiness observed in the Sickle Cell Reagent which will not readily dissolve upon mixing may indicate reagent deterioration. b. If the powder in the Sickle Cell Dithionite Reagent has become 2. Control Assays Failure to obtain accurate results in the assay of control materials may indicate reagent deterioration. Sterling Diagnostics cannot guarantee the stability of reagents, which have been: a. Transferred from their original containers; b. Improperly stored; c. Contaminated during use. SPECIMEN (6-7) Collect whole blood by venipuncture into vials or containers containing appropriate amount of anticoagulant, e.g. Heparin, EDTA, ACD CPD, CPDA-1 , Sodium or Potassium Oxalate, Sodium Citrate or use blood segments of whole blood or packed cells which have been mixed thoroughly. Specimens that have been kept for 1-2 weeks at 4-5oC are reportedly satisfactory for use in this period. No preliminary restriction of food or fluid is required for this test. MATERIALS PROVIDED Sickle Cell Reagent, 54 Vials with Sodium Dithionite and Sickle Cell Urea Reagent. ADDITIONAL MATERIALS REQUIRED Positive and Negative Sickle Cell Controls are available separately as Cat. No.2244-0 Reagent and sample pipets PROCEDURE 1. Transfer 2.0 ml of Sickle Cell Reagent to vials containing Sodium Dithionite, swirl to mix and label them: UNKNOWN, (+) CONTROL, (-) CONTROL. 2. Add 20 microliters of well-mixed whole blood to its respective vial and mix by gentle swirling. 2. 54 VIALS WITH SODIUM DITHIONITE: powdered sodium dithionite. Keep tightly capped and protected from moisture prior to reconstitution. 3. Allow to stand at room temperature for 5 minutes. 3. SICKLE CELL UREA REAGENT: Urea in aqueous solution. Keep tightly capped and protect from contamination. 4. Read the test by holding the test tube approximately 3-cm from the line scale provided with the test. Adequate illumination is necessary. 8. RESULTS Whitehead, T.P., Quality Control in Clinical Chemistry, John Wiley & Sons, New York (1977). READER SCALE POSITIVE: If HbS or any other sickling hemoglobin is present, the solution will be sufficiently turbid to prevent reading of the scale. NEGATIVE: If no sickling hemoglobin is present, the solution will be clear enough to allow the scale to be seen through the test vial. All doubtful tests, as well as all positive tests, should be confirmed by electrophoresis. FOR ALL POSITIVES, THE FOLLOWING STEP IS RECOMMENDED: NOTES 1. Transfer 2.0 ml of Sickle Cell Reagent to a vial containing Sodium Dithionite and mix by swirling. 2. Add 5 drops of Sickle Cell Urea Reagent and mix. 3. Add 20 microliters of positive whole blood and gently swirl to mix. 4. Let stand for 5 minutes and read against scale. The presence of HbS will be confirmed if the solution becomes clear in the presence of Urea Reagent. The only known variant that will also clarify is HbC (Harlem). PROCEDURE LIMITATIONS Severe anemia can cause false negatives; therefore, if the patient's hemoglobin is below 7.0 Gm/dl, the test should be repeated using 40 microliters of sample. False negative results may occur when HbS concentration is <15% of total hemoglobin, which may be the case when a patient is transfused with blood from a donor with HbS trait. The rare sickling hemoglobins C-Harlem, C-Georgetown, S-Travis, C-Ziguinchor and Hb Barts (if present in the blood of a fetus with hydrops fetalis due to a-thalasemia) reportedly (7) also give positive test results with this procedure. In patients who have had a splenectomy and have unstable hemoglobins, the test may appear positive due to the presence of numerous insoluble erythrocyte inclusions. In all cases where abnormalities are suspected or indicated, electrophoretic confirmation is recommended. PROCEDURE NOTES Samples that are highly lipemic or are borderline positive should have the following procedure performed: Centrifuge the whole blood specimen at 1500xg for 10 minutes and carefully remove the supernatant plasma and discard. Repeat the test using 20 microliters of the packed erythrocytes. QUALITY CONTROL Quality control samples should be used routinely to monitor test performance (8). We strongly recommend the use of Positive and Negative Sickle Cell Controls (Cat. No. 2244-0) for this purpose. BIBLIOGRAPHY 1. 2. 3. 4. 5. 6. 7. Widmann, F.K., Clinical Interpretation of Laboratory Tests, F.A. Davis Co., Philadelphia, pp. 57-60 (1983). Neel, J.V., Blood, 6:389 (1951). Itano, H.A., Arch. Biochem. Biophys., 47:148 (1953). Nalbandian, R.M., Nichols, B.M., Camp, F.R. et al, Clin. Chem., 17:10281032 (1971). Nalbandian, R.M., Nichols, B.M., Camp, F.R. et al, 17:1033 (1971). Calam, R.R. in Selected Methods of Clinical Chemistry, Vol. 9, Ed. by W.R. Faulkner and S. Meites, AACC Publications, Washington, pp. 3-10 (1982). Fairbanks, V.F. and Klee, G.G. in Textbook of Clinical Chemistry, Ed. N.W. Tietz, W.B. Saunders Co., Philadelphia, pp. 1540-1541 (1986). Product Availability Sickle Cell Reagent Set, 54 Tests, Cat. No. 2245-0: 110 ml 54 vials 10 ml Sickle Cell Reagent Sodium Dithionite Sickle Cell Urea Reagent Lit. No. 2245-0 (Rev B) Copyright 1986