Endocrinology of Pregnancy
advertisement
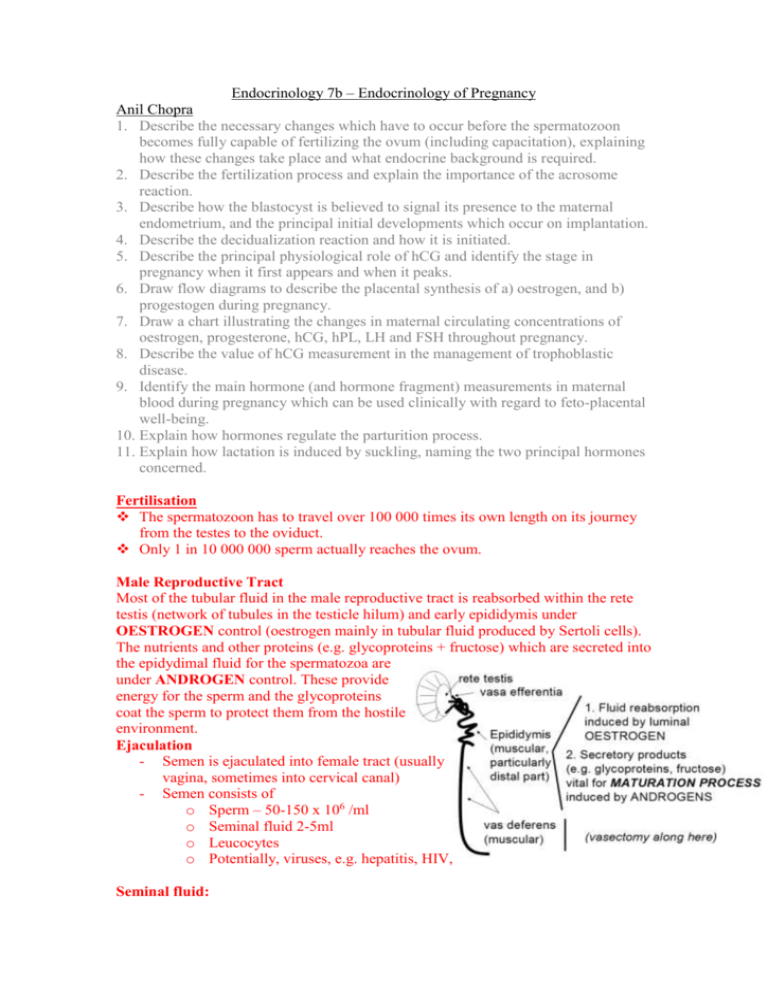
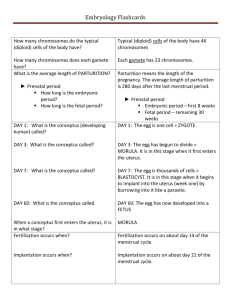
Endocrinology 7b – Endocrinology of Pregnancy Anil Chopra 1. Describe the necessary changes which have to occur before the spermatozoon becomes fully capable of fertilizing the ovum (including capacitation), explaining how these changes take place and what endocrine background is required. 2. Describe the fertilization process and explain the importance of the acrosome reaction. 3. Describe how the blastocyst is believed to signal its presence to the maternal endometrium, and the principal initial developments which occur on implantation. 4. Describe the decidualization reaction and how it is initiated. 5. Describe the principal physiological role of hCG and identify the stage in pregnancy when it first appears and when it peaks. 6. Draw flow diagrams to describe the placental synthesis of a) oestrogen, and b) progestogen during pregnancy. 7. Draw a chart illustrating the changes in maternal circulating concentrations of oestrogen, progesterone, hCG, hPL, LH and FSH throughout pregnancy. 8. Describe the value of hCG measurement in the management of trophoblastic disease. 9. Identify the main hormone (and hormone fragment) measurements in maternal blood during pregnancy which can be used clinically with regard to feto-placental well-being. 10. Explain how hormones regulate the parturition process. 11. Explain how lactation is induced by suckling, naming the two principal hormones concerned. Fertilisation The spermatozoon has to travel over 100 000 times its own length on its journey from the testes to the oviduct. Only 1 in 10 000 000 sperm actually reaches the ovum. Male Reproductive Tract Most of the tubular fluid in the male reproductive tract is reabsorbed within the rete testis (network of tubules in the testicle hilum) and early epididymis under OESTROGEN control (oestrogen mainly in tubular fluid produced by Sertoli cells). The nutrients and other proteins (e.g. glycoproteins + fructose) which are secreted into the epidydimal fluid for the spermatozoa are under ANDROGEN control. These provide energy for the sperm and the glycoproteins coat the sperm to protect them from the hostile environment. Ejaculation - Semen is ejaculated into female tract (usually vagina, sometimes into cervical canal) - Semen consists of o Sperm – 50-150 x 106 /ml o Seminal fluid 2-5ml o Leucocytes o Potentially, viruses, e.g. hepatitis, HIV, Seminal fluid: Produced by secondary sex glands: - Epididymis o inositol, carnitine, glycerylphosphorylcholine - Seminal vesicles and Prostate o Fructose o Fibrinogen o Citric acid o Acid phosphatase o Fibrinogenase Spermatozoon Activation & Capacitation - From seminiferous tubule o Spermatozoa unable to fertilize ovum - From vas deferens o Spermatozoa capable of movement (“whiplash activity”) and some capability for fertilizing an ovum. ACTIVATION - Full activity and capacity to fertilise is only achieved in the oviduct. CAPACITATION. - Only 1% of spermatozoon in ejaculate enters the cervix. 1. Loss of glycoprotein “coat” 2. Exposure of acrosome leading to ACROSOME REACTION (swelling, exposure 3. Whiplash movements of tail of contents to exterior) This all takes place in the oviduct (an ionic and proteolytic environment). They are all oestrogen dependent and the activation process is Ca2+ dependent. The Process of Fertilisation Once sperm have become “capacitated” in the oviduct, they bind to a binding site on the ZP3 glycoprotein (zona pellucida 3) on the ovum. The progesterone causes a huge influx of Ca2+ into the sperm and allows for the Ca-dependent acrosome reaction. This enables an exposed spermatozoon binding site to bind to a second glycoprotein (ZP2). The sperm releases proteolytic enzymes (e.g. hyaluronidase) and penetrates the zona pellucida and exposes itself to the egg. - occurs in the oviduct results in the expulsion of second polar body zona reaction occurs – prevents any other sperm from binding once diploidy (full set of chromosomes) is established, then the cell begins to divide into the conceptus. Conceptus • The conceptus continues to divide as it moves down from oviduct to uterus (3-4 days) => the free floating phase • Until implantation the developing conceptus receives its nutrients from uterine secretions • This free-living phase can last for about 9-10 days • Conceptus first compacts to 8-16 cell morula • Then it becomes a blastocyst: two distinct cell populations resulting in inner cell mass - which becomes the embryo - and outer trophoblast - which becomes the chorion. • It is transferred to the uterus at the blastocyst stage; this is facilitated by the increasing progesterone to oestrogen ratio (luteal phase) • It establishes physical and nutritional contact with maternal tissues 4-cell conceptus 2-cell conceptus 8-cell conceptus compaction Inner cell mass morula Fertilized egg Trophoblast cells Blastocoelic cavity blastocyst Implantation • In humans is INVASIVE • Involves an initial ATTACHMENT PHASE when outer trophoblast cells contact uterine surface epithelium • Within a few hours, results in DECIDUALIZATION of underlying uterine stromal tissue • This requires an endocrine background of PROGESTERONE DOMINATION in the presence of OESTROGEN. Uterine blastocyst secretory glands LIF OESTROGEN Makes stroma receptive (global) EGF receptors on trophoblast cells ZP dissolution and attachment/invasion of endometrium HSPG Release of HB-EGF In epithelial cells Initial signal from blastocyst? adjacent to blastocyst (local) LIF = Leukaemia Inhibitory Factor HB-EGF = Heparin-Binding EGF-epithelial growth factor HSPG = surface Heparin Sulphate ProteoGlycans Attachment • Oestrogen-induced release of leukaemia inhibitory factor (LIF) from endometrial secretory glands makes stroma receptive to implantation • Oestrogen-induced release of heparin-binding epithelial growth factor (HB-EGF) from endometrial cells. • HB-EGF binds to EGF receptors and HS proteo-glycans on outer trophoblast cells of blastocyst, and induces zona pellucida dissolution and promotes attachment and invasion of adjacent endometrium The Decidualisation Reaction • Involves the invasion of the underlying uterine stromal tissue by the trophoblast cells of the blastocyst • Within hours, results in increased vascular permeability in the invasion region associated with oedema of tissues, localized changes in intracellular composition and progressive sprouting and growth of capillaries; the DECIDUALIZATION REACTION • Factors involved in the decidualization reaction include histamine, certain prostaglandins, and TGFβ which promotes angiogenesis. Pregnancy In the first 5-6 weeks of pregnancy, the ovaries produce gonadal steroids to maintain the fetoplacental unit. After this point, hGC – human chorionic Gonadotrophin takes over this role and is produced by the developing implanting blastocyst (syncitiotrophoblast). Throughout pregnancy oestradiol and progesterone levels rise and LH and FSH are inhibited. From day 40 ovariectomy no longer has any effect on pregnancy since by this stage the role of the corpus luteum has been taken over by the fetoplacental unit. Parturition A number of different homones act on the myometrium to induce contraction including: - Oxytocin - Oestrogen - Progesterone This results in an influx of Ca2+ ions and which allows the contraction of the uterus through the action of calmodulin-myosin kinase. When the fetus reaches a certain size fetal oestrogen switches off the hormonal axis This acts to increase fetal steroid production so it is higher than the mother This initiates the parturition process – therefore the fetus is vital in dictating when parturition begins The myometrial smooth muscle cells are activated at the later stages of parturition, to enable contraction release of Ca stores is needed to increase intracellular Ca Oxytocin is released at the end stage of pregnancy Lactation Lactation is brought about by oxytocin and prolactin – both of which sit in neuroendocrine reflex arcs: Suckling induces neural pathways to the hypothalamus which stimulates the pituitary to produce oxytocin and prolactin which cause milk synthesis and ejection Hypothalamus SUCKLING (stimulus) Neural pathways Pituitary + Neurohypophysis Adenohypophysis Oxytocin Milk ejection Milk synthesis Prolactin