Pharmacokinetics and Drug Metabolism – Journey through
advertisement
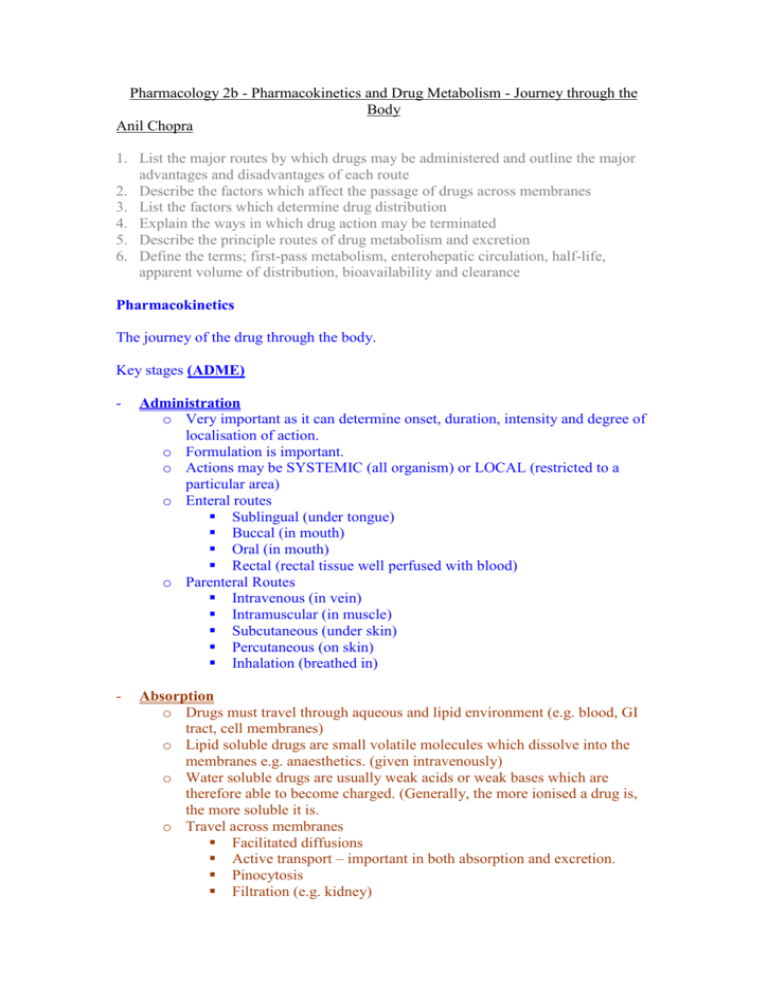
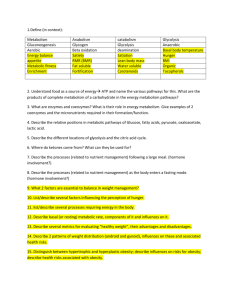
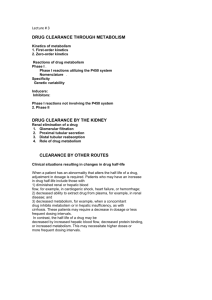
Pharmacology 2b - Pharmacokinetics and Drug Metabolism - Journey through the Body Anil Chopra 1. List the major routes by which drugs may be administered and outline the major advantages and disadvantages of each route 2. Describe the factors which affect the passage of drugs across membranes 3. List the factors which determine drug distribution 4. Explain the ways in which drug action may be terminated 5. Describe the principle routes of drug metabolism and excretion 6. Define the terms; first-pass metabolism, enterohepatic circulation, half-life, apparent volume of distribution, bioavailability and clearance Pharmacokinetics The journey of the drug through the body. Key stages (ADME) - Administration o Very important as it can determine onset, duration, intensity and degree of localisation of action. o Formulation is important. o Actions may be SYSTEMIC (all organism) or LOCAL (restricted to a particular area) o Enteral routes Sublingual (under tongue) Buccal (in mouth) Oral (in mouth) Rectal (rectal tissue well perfused with blood) o Parenteral Routes Intravenous (in vein) Intramuscular (in muscle) Subcutaneous (under skin) Percutaneous (on skin) Inhalation (breathed in) - Absorption o Drugs must travel through aqueous and lipid environment (e.g. blood, GI tract, cell membranes) o Lipid soluble drugs are small volatile molecules which dissolve into the membranes e.g. anaesthetics. (given intravenously) o Water soluble drugs are usually weak acids or weak bases which are therefore able to become charged. (Generally, the more ionised a drug is, the more soluble it is. o Travel across membranes Facilitated diffusions Active transport – important in both absorption and excretion. Pinocytosis Filtration (e.g. kidney) Paracelluar transport (in gaps around cells) Passive diffusion (most common) – an example of this is absorption from the stomach to the blood using the pH partition hypothesis. This states that in order for a drug to pass into the blood stream, it needs to be unpolarised so that it is lipid-soluble. - Distribution o Only once a substance has entered the blood or lymph is it truly absorbed o Once in the vascular system the drug can be distributed around the body o Factors affecting drug distribution: Regional blood flow Extracellular binding (plasma-protein binding) Capillary permeability (modifications – renal, hepatic, brain/CNS, placental) Localisation in tissues (special cases) - Metabolism - Excretion o Kidney – responsible for elimination of most drugs. Glomerulus – drug-protein complexes not filtered Proximal tubule – active secretion of acids and bases Proximal and distal tubules – lipid soluble drugs reabsorbed via passive diffusion. o Liver – occurs via the bile. Mainly occurs with drugs that have a large molecular weight. Liver has active transport systems which secrete the dugs into the bile. ENTEROHEPATIC CYCLING. (because bile is secreted in the GI tract and then reabsorbed) – a drug trapped in this process may persist in the body for longer. Other routes include lungs, gastrointestinal secretions, saliva, sweat, milk, genital secretions, integument Bioavailability – proportion of administered drug that is available within the body to exert its pharmacological effects Apparent Volume of Distribution – the volume in which a drug appears to be distributed – an indicator of the pattern of drug distribution Biological Half-Life – Time taken for the concentration of drug in blood or plasma to half its original value Clearance – Blood/plasma clearance is the volume of blood/plasma cleared of drug in a unit time. It is related to the volume in which the drug is dissolved and the rate at which it is eliminated. If several processes clear a drug then the total clearance is the sum of the individual clearances Therapeutic Concentration – concentration of drug that gives the desired effects Toxic Concentration – concentration of drug which is toxic Therapeutic Window – Difference from therapeutic dose to toxic dose, the bigger the window the more likely to be self-administered.