Detection, Prevention and Treatment in the Newborn
advertisement

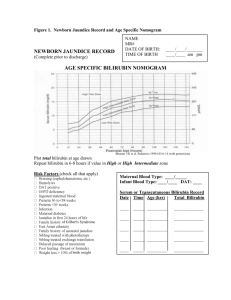
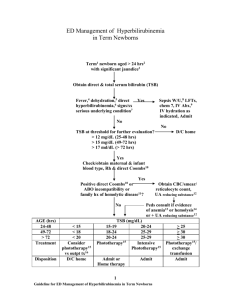
POLICY/PROCEDURE TITLE: Hyperbilirubinemia: Detection, Prevention and Treatment in the Newborn Women & Infant Services RELATED TO: [ ] Medical Center Policy (MCP) [ ] Nursing Practice Stds. [ x ] TJC [ x ] Patient Care Stds. [ ] QA [ ] Other [ ] ADMINISTRATIVE [ x ] CLINICAL PAGE _ OF _ Effective date: 10/04 Reviewed date: 4/09 Revision date: 11/06, 12/08 Unit/Department of Origin: Other Approval: [ ] Title 22 POLICY STATEMENT: To detect hyperbilirubinemia during the initial hospital stay for healthy infants >36 weeks in the Infant Special Care Center (ISCC), Family Maternity Care Center (FMCC) and Birth Center (BC) at UCSD Medical Center. Approximately 60% of all newborns will develop clinical jaundice; detecting elevated bilirubin levels may be beneficial in allowing prompt diagnosis and treatment of babies at risk for severe hyperbilirubinemia. Prevention of kernicterus is the goal of observation for and treatment of hyperbilirubinemia. 1. Promote and support successful breastfeeding as per the UCSD Lactation Policy and Baby Friendly Hospital Initiative guidelines. 2. All newborns will have vital signs per unit protocol, which involves a visual examination of skin color by the nurse. Every newborn will have a daily examination in good light by the medical team. 3. Infants with Rh sensitization will have a cord total serum bilirubin (TSB) sent stat at delivery and be admitted to the ISCC. 4. Every newborn that is found to have ABO or other blood group incompatibility will have a 12-hour blood draw including CBC, reticulocyte count, total and direct bilirubin. 5. All well newborns will have a TSB drawn at the time of their newborn metabolic screening. This is generally done at 24-48 hours of life. 6. A total and direct bilirubin will drawn on any infant who appears jaundiced in the first 24 hours of life or appears significantly jaundiced. 7. All TSB results will be plotted on the Hour Specific Bilirubin Nomogram (D436) by nursing staff, and the pediatrician on call notified if it exceeds the 95th percentile. 8. The pediatric team will also plot and chart all TSB values on the Hour Specific Bilirubin Nomogram (D436). This will remain in the infant’s medical chart. 9. Late preterm infants <38 weeks gestation are cared for according to the W&IS P&P: Late Preterm Infants. These infants receive additional assistance with feeding, temperature regulation, observation for jaundice, and have to meet specific discharge criteria. UCSD Medical Center page 2 10. All Newborns will have a risk assessment for hyperbilirubinemia performed by the medical team at discharge. The Hour Specific Bilirubin Nomogram (D436) contains a list of risk factors that can be used for this purpose. Any infant who appears jaundiced for his age, or has risk factors for the development of delayed hyperbilirubinemia shall have another serum bilirubin or transcutaneous bilirubin despite a normal initial screen value prior to discharge. 11. All parents receive “A New Beginning” book and parental handout on jaundice deriverd from the AAP’s “FAQs About Jaundice”. In addition, the Pediatric Team has a handout, “Jaundice and Phototherapy”, for parents who need or ask for additional information. 12. At discharge, all infants will either be given a follow up appointment with their medical provider, or the parents will be instructed to call and make an appointment at a specific time. The Newborn Record (which has the TSB levels) will be faxed to the provider/clinic. The current standard is that any baby discharged at 24 hours or less must have an appointment the next day, or within 48 hours if the clinic is closed on the next day. Healthy babies that go home on or after day 2 of life are to see their provider within 2-3 days. 13. The medical team will evaluate any baby with hyperbilirubinemia. Infants may require additional testing to investigate the cause of hyperbilirubinemia, as well as lactation assistance. Intensive phototherapy will be initiated if appropriate, and any baby who fails to respond to treatment or has severe hyperbilirubinemia will be transferred to the ISCC. RESPONSIBLE PARTY: Nurses in L&D, ISCC, FMCC and Birth Center EQUIPMENT: Quick Heel Lancet: green (term infant), pink/lavender (preemie) Green or yellow microtainers Chlorhexidine or alcohol. Sterile 2x2 gauze for chlorhexidine. Gauze. 3 or 5ml syringe. Oral sucrose. PROCEDURE: 1. All well infants will have a TSB drawn at the time of their newborn metabolic screen according to blood drawing policy. This generally occurs between 24-48 hours of age. Additional testing will be done per the above policy. Please see W&IS P&P: Blood Sampling, Heel Stick, Venipuncture. 2. The infant’s nurse will check the result. The result will then be plotted on the Hour Specific Bilirubin Nomogram (D436). D436.pdf UCSD Medical Center page 3 3. If the TSB falls above the 95th percentile, the nurse will call the on-call pediatrician to evaluate the infant. 4. Infants may not be discharged to home prior to TSB result review. If an infant is an early discharge and the TSB is > 75th percentile the nurse must discuss the result with the baby’s provider. REFERENCES: American Academy of Pediatrics, Subcommittee on Hyperbilirubinemia. (2004). Clinical Practice Guideline: Management of Hyperbilirubinemia in the Newborn Infant 35 or More Weeks of Gestation. Pediatrics: 14:297-316. Alpay F, Sarici SU, Tosuncuk HD, Serdar MA, Inanc N, Gokcay E. (2000). The Value of First-Day Bilirubin Measurement in Predicting the Development of Significant Hyperbilirubinemia in Healthy Term Newborns. Pediatrics:106:e16. Bhutani VK, Johnson L, Sivieri EM. (1999). Predictive Ability of a Predischarge Hour-Specific Serum Bilirubin for Subsequent Significant Hyperbilirubinemia in Healthy Term and Near-Term Newborns. Pediatrics: 103:6-14. Johnson LH, Bhutani VK, Brown AK. (2002). System-Based Approach to Management of Neonatal Jaundice and Prevention of Kernicterus. J Pediatr:140:396-403. Kenner, C. and Lott, J. (2003) Comprehensive Neonatal Nursing; A Physiologic Perspective. Saunders, New York: 597-799. Merenstein, G. & Gardner, S. (2002) Handbook of Neonatal Intensive Care, Mosby, St. Louis: 443-459.