File - THE Portfolio
advertisement

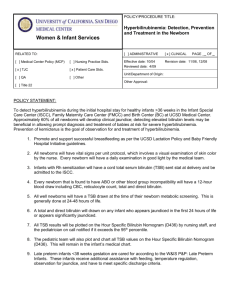
Velazquez1 Emilie Velazquez Wolcott ENC1102 Literacy Review Hyperbilirubinemia is a very common among disease newborns. It deals with the total serum bilirubin (TSB) levels on infants. Right before the nineties it was believed that the disease was almost disappearing. During the 1990’s there was a trend that caused the number of hyperbilirubinemia cases to rice again. That trend was the early discharging of newborns and their mothers (De Luca, et al., Lauer and Spector). Early discharging lead to a difficulty in the diagnosing and treating part of the disease. In order to diagnose this problem, specialists recommend a hyperbilirubinemia evaluation after the birth of the infant, which in some cases was not done. This evaluation is a physical one followed by a laboratory one if there is a reason to believe hyperbilirubinemia might occur. Different researchers discussed different methods to be used to detect the onset of hyperbilirubinemoia. There are various methods discussed are the use of nomograms, clinical assessments, the Kramer, the Minolta JM-102, and the BiliCheck (Arlettaz, Romaine, et al.). The American Academy of Pediatrics recognizes the challenges in diagnosing hyperbilirubinaemia in infants after their discharge (Schwartz et al). The reason for this is the fact that parents do not have follow ups right after being discharged. The follow ups usually happen a few days or they are delayed (Stark et al.). Since they do not test for the TSB levels immediately, the newborn’s TBS levels may rise and have or be at a high risk of developing hyperbilirubinaemia. It is advised by the American Academy of Pediatrics that these methods should be used to check for hyperbilirubinemia before the discharge of the newborn. This will Velazquez2 give an idea to whether the newborn has a high risk or low risk of developing hyperbilirubinemia. There has been a debate within the community over which type of procedures should they use to test for hyperbilirubinemia, invasive or noninvasive. The use of nomograms is strongly recommended by the Academy of Pediatrics. Nomograms are the most frequently used method around the world. The APA has three steps to be followed by neonatologists before discharging newborns. The first is to recognize physical factors that might show that the infant can be on the risk of developing neonatal jaundice. Second, they stressed that a test for hyperbilirubinemia is done before discharge and they recommend the hour specific nomogram since it is the most accurate (De Luca et al., Lauer and Spector). The nomogram requires hourly serum bilirubin checks. The results of this test will indicate under which percentile the newborn is. While diagnosing, the doctors should follow the population’s averages and the specific race of the infant. If the newborn falls within the 95th percentile of his respective race and population’s nomogram the newborn should stay for further testing (De Luca et al.). The use of nomograms can be seen as controversial since it requires the taking of blood samples multiple times.There have been new approaches towards detecting hyperbilirubinemia and these new methods are noninvasive. Those noninvasive methods are the use of the Kramer, the Minolta JM-102, and the BiliCheck. They compared the bilirubin values collected from these methods to the values received from a nomogram. In their study, the Minolta JM-102 was the most accurate and had the best performance (Arlettaz, Romaine, et al.) The use of these noninvasive methods is a breakthrough in detecting hyperbilirubinaemia in newborns. The newborns will not have to go through painful extractions of blood samples to detect their bilirubin levels, which can also leave scaring. Velazquez3 It was also discovered that there is not always a need for these scientific approaches to detect hyperbilirubinemia. In Be’er Sheva, Israel newborns go through a clinical assessment to determine how likely they are to develop hyperbilirubinemia. In this area of Israel there are services outside the hospitals that are provided to new mothers. These services are offered in a postnatal home where the mother could stay up to two weeks (Hammerman et al.). They have nurses who will stay and assist the mother and check on how the newborn is doing. In Cathy Hammerman study it was found that the rate of readmission due to hyperbilirubinemia had decreased. There will always be the potential for hyperbilirubinemia but with the risk assessment administered before discharge, the availability of follow-up services and the community and religious support system, there have been less readmission of newborns. There are various methods to use when it comes to detecting hyperbilirubinemia. Even though there are differences in the approaches, whether it is invasive or not, there is one thing that it is clear and that is the time frame when they are done. It is necessary that before discharge, newborn are tested for their bilirubin levels. Those who are becoming parents for the first time need to be educated about this topic. These new parents are in the process of development and learning as well as their newborn. In contrast those who are becoming parents for the second or third time are already educated and know about what hyperbilirubinemia is and its testing. There needs to be more attention brought to this specific disease since it is the most common one in newborns and maybe by bringing awareness to it the readmission rate for newborns will lower. The goal would be to hopefully get the readmission rate as low as it was in the 1990’s. Velazquez4 Works Cited Arlettaz, Romaine, et al. "Detection Of Hyperbilirubinaemia In Jaundiced Full-Term Neonates By Eye Or By Bilirubinometer?." European Journal Of Pediatrics 163.12 (2004): 722727. MEDLINE. Web. 03 Apr. 2013. De Luca, Daniele, Virgilio P Carnielli, and Piermichele Paolillo. "Neonatal Hyperbilirubinemia And Early Discharge From The Maternity Ward." European Journal Of Pediatrics 168.9 (2009): 1025-1030. MEDLINE. Web. 03 Apr. 2013 Hammerman, Cathy, et al. "Evaluation Of Discharge Management In The Prediction Of Hyperbilirubinemia: The Jerusalem Experience." The Journal Of Pediatrics 150.4 (2007): 412-417. MEDLINE. Web. 03 Apr. 2013. Lauer, Bryon J, and Nancy D Spector. "Hyperbilirubinemia In The Newborn." Pediatrics In Review / American Academy Of Pediatrics 32.8 (2011): 341-349. MEDLINE. Web. 03 Apr. 2013. Schwartz, J S,et al. "Identifying Newborns At Risk Of Significant Hyperbilirubinaemia: A Comparison Of Two Recommended Approaches." Archives Of Disease In Childhood 90.4 (2005): 415-421. MEDLINE. Web. 03 Apr. 2013. Stark, Ann R, et al. "Delayed Pediatric Office Follow-Up Of Newborns After Birth Hospitalization." Pediatrics 124.2 (2009): 548-554. MEDLINE. Web. 03 Apr. 2013.