Hemolytic disease of the new born (HDN) HYPERBILIRUBINEMIA
advertisement
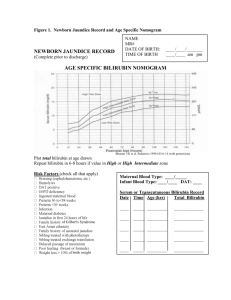
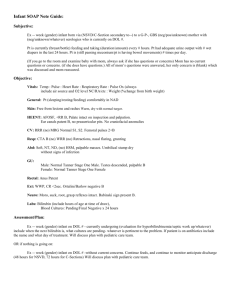
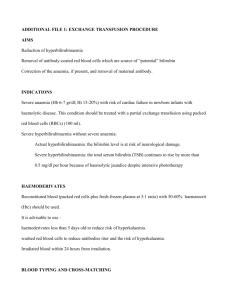
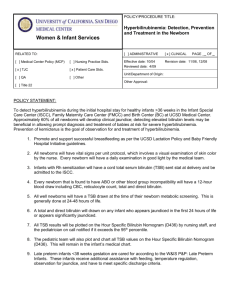
Hemolytic disease of the new born (HDN) HYPERBILIRUBINEMIA Dr. Nihad Al Doori 5th lecture Objectives: • At the end of the lecture the student will be able to: 1. Describe the concept of bilirubinemia 2. Recognize the causes of bilirubinemia 3. Evaluate the prognosis of the condition of the infant receiving the different types of therapy for hyperbilirubinemia e.g. phototherapy and exchange blood transfusion 4. Develop awareness for the serious side effects of hyperbilirubinemia 5. Recognize the need of the parents for support and comforting • Hyperbilirubinemia: Refers to the increased level of accumulated bilirubin in the blood & characterized by jaundice or icterus. • Normally there is balance between the destruction of RBCs and the use or secretion of it’s products Causes of Hyper bilirubinemia: 1. physiologic (developmental) factors such as, prematurity 2. An association with breast-feeding or breast milk 3. Excess production of bilirubin e.g. hemolytic disease, biochemical defects, and bruises 4. Disturbed capacity of the liver to secrete conjugated bilirubin, e.g. enzyme deficiency, bile duct obstruction. 5. Combined over production and under secretion e.g. sepsis 6. Some disease states e.g. hypothyroidism, galactosemia, and infants of diabetic mothers • Anemia in this condition is caused by the destruction of the RBCs which stimulate the ↑ production of +++ RBC leading to more hemolysis. • Hyperbilirubinemia in the first 24hrs after birth result of: • Erythroblastosis fetalis in which there is an abnormally rapid rate of RBCs destruction. The major cause of erythrocyte destruction is: Isoimmunization primary Rh & ABO incompatibility. Blood incompatibility • Antibodies in the serum of a blood group will produce agglutination or clumping reaction when mixed with antigens of a different blood group. • The maternal blood type is O and the fetal blood type is A; it may also occur when the fetus has type B or AB blood. Rh incompatibility (Isoimmunization) • The blood group consists of several antigens, the Rh +positive (presence of antigen) & the Rh-negative (absence of the antigen). • If the Rh blood types are the same in the mother & the fetus NO problem • If the Rh blood type of the mother is Rh + positive & the infant is Rh- negative also NO problem • Difficulty will occur when the blood of the mother is Rh -negative & the infant is Rh + positive, the Rh antigen from the fetus will cross the placenta though minute break in the vessels • The mother’s natural defense mechanism will produce anti Rh antibodies in respond to the alien RBCs of the Rh positive from the fetus. • This usually occurs during labor, so this first baby is not affected. • During subsequent pregnancies with Rh positive fetus, the previously formed maternal antibodies enter the fetal circulation and attack and destroy the fetal erythrocytes • In the severe cases of Erythroblastosis fetalis hydrops fetalis the progressive hemolysis causes: • Fetal hypoxia • Cardiac failure • Generalized edema • Effusion of the pericardial, pleural & peritoneal spaces • Fetus may be delivered stillborn or in severe respiratory distress • Complications of hyperbilirubinemia: Uncojugated bilirubin is highly toxic to the neurons bilirubin encephalopathy (Kernicterus) sever damage of the brain, which occurs when the serum concentrations reaches toxic levels & crosses the blood-brain barrier in the newborn causing irreversible brain damage. Signs of bilirubin ncephalopathy: • • • • • • Rigid extension of all limbs Opisthotonus Fever Irritability Cry Seizures Diagnostic evaluation: • Amniocentesis & analysis of bilirubin levels in the amniotic fluid if it is increasing then there is progressive hemolysis • Rh-antibody tiers in the maternal blood can be evaluated (indirect coomb,s test) • can be confirmed by detecting antibodies attached to the circulating RBCs in the infant’s blood (direct coombs test). Management & Treatment: • The aim is prevention of isoimmunisation by: • Administration of RhO — Immuno-Globin (Rh.OGAM) injection to all unsensataised Rh negative mothers after delivery or abortion of an Rh positive infant or fetus • The injection to be given within 72 hrs after delivery. • Injection of anti - Rh antibodies destroy the fetal erythrocytes passing into the maternal circulation before they can exert their immunogenic effect, this injection has to be given after the first delivery to be repeated after subsequent ones • Administration of the injection at 26 — 28 weeks of gestation is also recommended to decrease antibody formation but it is not effective on the already formed antibodies. • Physiologic ( NON pathologic )jaundice: Is the most common cause and is relatively mild self-limited. It appears 2nd or 3rd day and peaks on 3rd or 4th and decreases on the 5th day to 7th day • • • • Causes are : Higher concentration of circulating RBCs Immature liver Absence of intestinal flora in the NB which is responsible for reducing urobilinogen to be excreted by feces. The ↓ intestinal motility if feeding is delayed Therapeutic management:Primary goals are to prevent bilirubin encephalopathy. Early Initiation of br. Or bottle feeding. • Photo therapy → photoisomirization • Florescent light spectrum . • Exchange transfusion (hemolytic disease). • Use of Phenobarbital (hemolytic disease ) • Early initiation of feeding (breast feeding) if bilirubin is 17mg /dl stop breast feeding for 24 hrs and resume when it decreases. Exchange transfusion: this will help to: 1. Remove the sensitized RBCs 2. Decrease the serum bilirubin level to prevent Kernicterus 3. Correct anemia 4. Prevent cardiac failure Indications for exchange transfusion: • Positive direct coomb’s test • Hb<12g/dl • Bilirubin level of 20 mg/dl in the full term infant or 15 mg/dl in the premature infant • An infant born with Erythroplastosis fetalis is a candidate for immediate exchange transfusion with fresh whole blood • Small amounts of the infant’s blood (2-10 ml) of the infant’s blood is removed & replaced with compatible blood • Amount of blood used is double the newborn’s blood volume(85 ml/Kg) 500ml • Sterile procedure is used to introduce the umbilical catheter and is passed into the inferior vena cava • (5-10)ml of the infants blood is withdrawn within 15 — 20 sec • the same amount of blood is withdrawn from the donor blood & infused into the infant’s circulation within 60 — 90 sec • Calcium gluconate is given after each 100 ml of blood transfusion to prevent hypocalcaemia • This procedure will replace 55% of the newborn’s blood Phototherapy • Phototherapy, in which the baby is placed under a fluorescent light are placed 12 to 30 inches , lowers the bilirubin in the neonate's blood. Term newborns are generally scheduled for phototherapy when the total serum bilirubin level rises to 10 to 12 mg/dL at 24 hours of age; Fibro optic blanket It is ideal for home care. The infant is undressed except for a diaper so as much skin surface as possible is exposed to the light Nursing considerations: • Recognition of hyperbilirubinemia is very important antenatal & perinatally by history assessment & looking for early signs of jaundice in the newborn • If exchange transfusion is needed the nurse will reassure the parents • Assist the physician with the procedure by keeping accurate records of the amount of blood given & removed • Observing the vital signs • keeping the infant warm. • Observe the umbilical catheter & is kept covered with sterile gauze after the procedure is finished in case another exchange is needed. Thank You