High Risk Neonate
advertisement

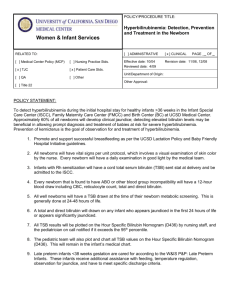
High Risk Neonate Christina Hernandez RN, MSN The High Risk Newborn Susceptible to illness or death due to dysmaturity, immaturity, physical disorders, or complications at birth. Risk Factors: Low socioeconomic status, poor nutrition Exposure to environmental dangers Obstetric factors such as age, parity, or other premature births Medical conditions related to the pregnancy such as PIH, PROM, or infection Gestational Age Classification of High Risk Newborns Gestational Age Preterm – less than 37 weeks gestation (Late Preterm – 34 – 36.6 weeks gestation) Term – 38-41 weeks gestation Postterm – greater than 42 weeks gestation LGA – large for gestational age - above the 90th percentile AGA – appropriate for gestational age – between the 10th and 90th percentile SGA – small for gestational age – below the 10th percentile Assessment of Gestational Age Ballard Scale or Dubowitz scale Neuromuscular characteristics Physical Characteristics Classification of High Risk Newborn Large for Gestational Age LGA Appropriate for Gestational Age AGA Small for Gestational Age SGA Maturity and Intrauterine Growth Grid The Preterm Infant Characteristics of Preterm Infants Appear frail & weak Underdeveloped flexor muscles & muscle tone Head is larger in comparison with the rest of the body Lack subcutaneous fat (white fat) Skin appears red and translucent Barely apparent small flat nipples Plantar creases are absent in infants <32 wks The pinna of the ear is soft and flat Female – Male – Physiologic challenges of the premature infant - Respiratory Insufficient production of surfactant Immaturity of alveolar system Immaturity of musculature and insufficient calcification of bony thorax Respirations 40-60/min., shallow, irregular, usually diaphragmatic. Nursing interventions - Respiratory Assess for signs of Respiratory Distress Nasal Flaring Circumoral Cyanosis Expiratory Grunting Retractions Tachypnea Apneic episodes Administer O2 ◦ ◦ ◦ ◦ ◦ Warmed and humidified Oxihood Nasal Cannula CPAP Analyze oxygen concentration. Nursing interventions - Respiratory Positioning Position with head slightly elevated and neck slightly extended Side-lying or prone Suctioning Only use when necessary Be gently so as not to damage fragile mucus membranes Physiologic Challenges in the preterm infant - Thermoregulation Heat regulation unstable Body temperature may be normal but it fluctuates Higher ratio of body surface in proportion to body weight. Lack of subcutaneous fat Poor capillary response to environmental changes. Decreased brown fat Thinner skin Signs of Inadequate Thermoregulation Axillary temperature <36.3 or >36.9 degrees C Abdominal skin temperature <36 or >36.5 degrees C Poor feeding or feeding intolerance Irritability Lethargy Weak cry or suck Decreased muscle tone Cool skin temperature Skin pale, mottled, or acrocyanotic Signs of hypoglycemia Signs of respiratory difficulty Poor weight gain Nursing Interventions Thermoregulation GOAL: Neutral thermal environment. Thermal Neutrality – Nursing Interventions Incubator or radiant warmer Warm surfaces Warm humidified oxygen Warm ambient humidity Warm feedings Keep skin dry and head covered Isolette / Incubator Radiant Warmer/ Open Warmer Physiologic ChallengesFluid & Electrolyte Balance Preterm infants lose fluid very easily Rapid respiratory rate and use of oxygen increase fluid lose from the lungs Lack of keratin, which helps maintain water in the skin Large surface area & lack of flexion increases insensible water losses Radiant warmers heighten insensible water loss Physiologic ChallengesFluid & Electrolyte Balance Development of kidneys is not complete until approximately 35 weeks. In ability of preterm kidneys to concentrate or dilute urine. Kidneys unable to regulate electrolytes. Physiologic ChallengesFluid & Electrolyte Balance Dehydration Overhydration Urine output >2 ml/kg/hour Urine output >5 ml/kg/hour Urine specific gravity >1.020 Urine specific gravity <1.001 Weight loss greater than expected Edema Dry skin and mucous membranes Weight gain greater than expected Sunken anterior fontanel Bulging fontanels Poor tissue turgor Blood: Decreased sodium, protein, and hematocrit levels Blood: Elevated sodium, protein, and hematocrit levels Moist breath sounds Difficulty breathing Nursing InterventionsFluid and Electrolyte Balance Weigh diapers (1gm = 1ml of urine) Obtain specific gravity Carefully regulate IV fluids Dilute IV medications in as little fluid that is recommended (include medications on intake measurements) Assess IV sites frequently Physiologic ChallengesSkin The Preterm infants skin is: • Fragile • Transparent • Permeable Nursing InterventionsSkin Nursing Care No use of alcohol or betadine on skin All skin products should be rinsed off with water No use of adhesives, use pectin barriers and back tape with cotton Use semi-permeable adhesives such as tegaderm Reposition frequently, as tolerated Physiologic ChallengesInfection Exposure to maternal infections Lack of transfer of immunoglobulin G (IgG) from mother during third trimester Immature immune response to infection Subject to invasive procedures (IV’s, lab’s) Prolonged hospital stays Signs and Symptoms of Infection in the preterm infant Behavioral changes Color changes Temperature instability Cool, clammy skin Feeding intolerance Hyperbilirubinemia Tachycardia followed by apnea and bradycardia Nursing InterventionsInfection Maintain skin integrity Maintain sterile technique with procedures ‘Scrub’ before entering – EVERYONE Hand sanitizer at every bedside and used in between care No entry if sick – EVERYONE No artificial nails / short nails Single infant incubators, clean weekly Report early signs of infection immediately Assess infants response to treatment (possible resistance) Position change, use sheepskin Physiologic Challenges – Hepatic System Poor glycogen stores -increased susceptibility to hypoglycemia. Inability to conjugate bilirubin - increase hyperbilirubinemia. Decrease ability to produce clotting factors, low plasma prothrombin levels. Physiologic Challenges – Renal System Decreased glomerular filtration rate Inability to concentrate urine Decreased ability of kidneys to buffer Decreased drug excretion time Pain in preterm infants High-pitched, intense, harsh cry Whimpering, moaning “Cry face” Eyes squeezed shut Mouth open Grimacing Bulging or furrowing of brow Tense, rigid muscles or flaccid muscle tone Rigidity or flailing of extremities Color changes: Red, dusky, pale Increased or decreased heart rate and respirations, apnea Decreased oxygen saturation Increased blood pressure Sleep-wake pattern changes Nursing Interventions Swaddle, wake slowly Pacifier, may use Sucrose Medications Signs of Overstimulation in Preterm Infants Oxygenation changes Respirations Pulse Blood pressure Oxygen saturation levels Color Sneezing, coughing, hiccupping Behavior changes Posture Facial expression Gaze Regurgitation Yawning Fatigue Physiologic Challenges – Digestive System Decreased gag and suck reflexes Hypotonic cardiac sphincter Suck and swallow reflexes may be uncoordinated Small stomach capacity Vomiting Intolerance of fats Immature absorption of nutrients Maintaining Nutrition Nursing Care Assess Daily weights Monitor I&O Accurate IV rates to prevent circulatory overload Provide feedings via nasogastric if unable to feed orally Initiate oral feedings and assess for tiring with feedings Monitor urine pH and specific gravity Involve parents in feedings Nursing Interventions Pre-feeding assessment Respirations Measure abdominal girth Bowel sounds Gastric residual Sucking , swallowing , and gag reflexes Readiness for Nipple Feeding Rooting Sucking on gavage tube, finger, or pacifier Able to tolerate holding Respiratory rate <60 breaths per minute Presence of gag reflex Signs of Nonreadiness for Nipple Feedings Respiratory rate >60 breaths per minute No rooting or sucking Absence of gag reflex Excessive gastric residuals Parenting Facilitating Parent-Infant Attachment Prepare parents for first visit Establish safe/trusting environment Equipment, tubes etc. Provide support, reassurance, encouragement Encourage visitation Involved in care taking Repeat explanations Promote touching, talking, rocking, cuddling Refer to infant by name Allow parents to phone as desired Common Complications of Preterm Infants Respiratory Distress Syndrome Respiratory Distress Syndrome Pathophysiology Primary absence, deficiency or alteration in the production of surfactant Decrease in Surfactant = increase in atelectasis = lack of gas exchange Leads to hypoxia and acidosis which further inhibit surfactant production and causes pulmonary vasoconstriction. Common Clinical manifestations: Nasal Flaring Circumoral cyanosis Expiratory grunting Retracting Tachypnea Respiratory Distress SyndromeNursing Interventions Maintain airway, oxygenation, ventilation Supplemental oxygen: Nasal prongs Oxyhood Continuous positive airway pressure (CPAP) Intubation with endotracheal tube Surfactant Replacement Therapy Surfactant preparation can be lifesaving and reduces complications, such as pneumothorax. Administered through an endotracheal tube Surfactant treatments may be repeated several times during the first days until respiratory distress syndrome resolves. Respiratory Distress SyndromeNursing Interventions Nutrition Support Newborns with RDS may be given food and water by the following means: Tube feeding—a tube is inserted through the baby's mouth and into the stomach Parenteral feeding—nutrients are delivered directly into a vein Support to Parents Allow parents to hold and feed when possible. Assist to decrease their fears Periventricular-Intraventricular Hemorrhage Periventricular-Intraventricular Hemorrhage Rupture of fragile blood vessels around the ventricles of the brain Usually associated with hypoxia Diagnosed via cranial ultrasound Signs – lethargy, poor muscle tone, decreased reflexes, seizures, apnea or cyanosis, full or bulging fontanels Nursing Care – daily measure FOC, observe for changes in LOC Retinopathy of Prematurity Retinopathy of Prematurity Formation of immature blood vessels in the retina constrict and become necrotic Most common in infants < 28 weeks gestation Also associated with O2 therapy Retinopathy of Prematurity Nursing Interventions to Prevent ROP Administer O2 in concentration ordered Ensure proper ventilatory settings Necrotizing Enterocolitis Necrotizing Enterocolitis An inflammatory disease of the intestinal tract frequently complicated with perforation of the gut. NEC develops when there is asphyxia or hypoxia in which cardiac output tends to be directed more toward the heart and brain and away from the abdominal organs. The intestinal cells become ischemic and damaged and stop secreting protective mucus infection occurs. Perforation may occur with overwhelming sepsis. Necrotizing Enterocolitis Signs and Symptoms Early: Increase in gastric aspirate - >5-25 ml. Increase in abdominal girth Decrease bowel sounds, abdominal tenderness or rigidity of abdominal wall. Subtle: Lethargy, sudden listlessness, temperature instability, decrease urine output, occult blood in stools, poor color, and apneic periods. Dramatic: Massive abdominal distention, vasomotor collapse. Necrotizing Enterocolitis Treatment and Nursing Care Surgery: Resection of necrotic sections and possible temporary colostomy. This allows bowel to recover. Medical: NPO with NG tube. Peripheral or central hyperalimentation Antibiotic therapy. Continue to monitor for changes in condition. Gradually introduce oral feedings Post-Term Newborn Greater than 42 weeks gestation Post Mature Infant Physical manifestations: Dry, cracking, parchment-like skin Reduced subcutaneous tissue -Loose appearing skin No vernix or lanugo Long fingernails Profuse scalp hair Long, thin body appearance Often meconium stained skin, cord, nails Post Mature Infant Complications of post term: Hypoglycemia Meconium aspiration Congenital anomalies Seizure activity Cold stress Small for Gestational Age Below the 10th percentile Risk Factors Maternal factors: ◦ High blood pressure. ◦ Chronic kidney disease. ◦ Advanced diabetes. ◦ Heart or respiratory disease. ◦ Malnutrition, anemia. ◦ Infection. ◦ Substance use (alcohol, drugs); Cigarette smoking. Factors involving the uterus and placenta: ◦ Decreased blood flow in the uterus and placenta. ◦ Placental abruption (placenta detaches from the uterus). ◦ Placenta previa (placenta attaches low in the uterus). ◦ Infection in the tissues around the fetus. Factors related to the developing baby (fetus): ◦ Multiple gestation (twins, triplets, etc.). ◦ Infection. ◦ Birth defects. ◦ Chromosomal abnormality. Complications of the SGA Newborn Asphyxia Aspiration syndrome Hypothermia Hypoglycemia Polycythemia Large for Gestational Age Greater than 90th percentile What condition is associated with the newborn being LGA? Complications of the LGA newborn Birth Trauma Increase of Cesarean births Hypoglycemia Polycythemia Hyperviscosity Asphyxia of the Newborn Asphyxia Lack of oxygen and increase of carbon dioxide in the blood Occurs in utero or after birth S/S asphyxia after birth: Cessation of respirations and rapid fall in heart rate Interventions: Primary apnea: stimulation and O2 Secondary apnea: positive pressure ventilation &/or chest compressions Naloxone 0.1mg/kg IM (if narcotics given to expectant mother shortly before birth) Meconium Aspiration Syndrome Meconium Aspiration Syndrome Meconium stained amniotic fluid Aspirated into the trachobronchial tree Occurs either in utero or after birth with the first breaths. Meconium in the lungs causes air to become trapped and results in alveoli over-distension and rupture. Meconium Aspiration Syndrome Measures for Prevention of Meconium Aspiration After delivery of the infant’s head while shoulders and chest are still in the birth canal, Suction oropharynx and nasopharynx After delivery of the infant’s body Crying - Stimulate - Suction with bulb syringe Not crying - Do not stimulate - Direct tracheal suction with endotracheal tube Meconium Aspiration Syndrome Intubation Suction Meconium Aspiration Syndrome Nursing Interventions: Maintain adequate oxygenation and ventilation Regulate temperature Accurate IV fluid administration Assess for hypoglycemia Administer antibiotics Prevent caloric requirements Provide support care if on ECMO Hyperbilirubinemia Hyperbilirubinemia Pathophysiology Unconjugated bilirubin is a break-down product of destroyed RBC’s. Unconjugated bilirubin is normally transferred in the plasma firmly bound to albumin to the liver where conjugation occurs. Conjugated bilirubin is water soluble and can then be excreted into the bile and eliminated with the feces. Unconjugated bilirubin is not in excretable form and remains in the circulation causing problems. Hyperbilirubinemia occurs when the body cannot conjugate the bilirubin released into the serum. Causes of Hyperbilirubinemia Hemolytic disease (Rh and ABO incompatibility) Extravascular bleed (cephalhematoma) Bilirubin conjugation defects (breastmilk jaundice, asphyxia) Hypoalbumin Physiologic jaundice (occurs after the first 24 hours of birth. Mainly due to immature liver and lack of glucoronyl transferase). Hyperbilirubinemia Clinical Manifestations: Sclerae appearing yellow before skin appears yellow – usually in the first 24 hours after delivery Skin appearing light to bright yellow – advances from head to toe Lethargy Dark, amber concentrated urine Poor feeding Dark stools Hyperbilirubinemia Diagnosis: Bilirubin levels on Cord Blood Average level of Unconjugated bilirubin is 2 mg/dl at birth Bilirubin levels should NOT exceed 5 mg/dl Coombs Test may be done on the fetal cord blood (direct Coombs test) or on the maternal blood (indirect Coombs test). Tests for the presence of maternal antibodies attached on the infant’s red blood cells. The test is positive if there are maternal antibodies. Hyperbilirubinemia Nursing Care Careful observation of infant for signs of increased jaundice Careful observation for and prevention of acidosis/hypoxia and hypoglycemia, which decrease binding of bilirubin to albumin and contribute to jaundice. Maintain adequate hydration Avoid cold stress Phototherapy – use of “bili” lights, special fluorescent Exchange Transfusion Hyperbilirubinemia Nursing Care Nursing Interventions for Phototherapy Exposure of skin Cover eyes (remove for feeding/parent visit) Monitor temperature – prone to hyperthermia or hypothermia Reposition newborn every 2 hours Increase fluids Assess for dehydration Perform T-Bili q 12 – 24 hr as ordered Explain need to keep under phototherapy except during feedings and diaper changes. Explain to parents and allow them to hold during feedings Hyperbilirubinemia Phototherapy Side Effects to Phototherapy Frequent loose, green stools Skin rash Increased basal body metabolism Dehydration Hyperthermia Hyperbilirubinemia Exchange Transfusion Exchange Transfusion Treat anemia Remove sensitized RBCs that will soon lyse Remove serum bilirubin Provides albumin to increase bilirubin binding sites Hyperbilirubinemia Rhogam Provides temporary passive immunity which prevents permanent active immunity (antibody formation) Given within 72 hours of delivery Prevents production of maternal antibodies Hyperbilirubinemia ABO incompatibility Occurs when type O pregnant woman with A, B or AB blood type fetus If woman has anti A or anti B antibodies, these antibodies cross the placental barrier Results in hemolysis of fetal RBCs Hyperbilirubinemia Complications of Hemolytic Disease Kernicterus – Deposits of conjugated and unconjugated bilirubin in the basal ganglia of the brain Neurologic damage Hydrops fetalis – severe anemia Marked edema Cardiac decompensation Multiple organ failure Possible death Infections TORCHA Infectious Diseases: TORCH Toxoplasmosis Other Syphillis Hepititis B Rubella Cytomegalovirus Herpes Simplex II HIV - AIDs Toxoplasmosis Protozoan infection in the pregnant woman Raw or under cooked meats Infected Cat feces Transmission: transplacental Affects on the fetus Retinochoroiditis (inflammation of the retina and choroid of the eye. Blindness Deafness Convulsions Microcephaly Hydrocephaly Severe mental impairment Other - Syphillis Transmission: Transplacental Clinical Manifestations: Rhinitis (Snuffles) Excoriated upper lip Red rash around mouth and anus Copper colored rash of face, palms and soles Irritability Edema Cataracts. Treatment: Culture orifices Isolation Penicillin Other – Hepatitis B Transmission Placental Birth Breast milk Treatment If mother + HbSAG - administer to newborn: Hepitisis B vaccine HBIG (administer within 12 hours of birth) Rubella Transmission: transplacental S/S of Newborn Congenital cataracts Deafness Congenital heart defects Sometimes fatal Intellectual disability (Affects are greatest if infected in 1st trimester) MMR Immunization of mother Give when not pregnant – usually in immediate postpartum period. Newborns are infectious: CONTACT ISOLATION Cytomegalovirus Herpatic virus Transmission: Crosses placental barrier Direct contact at birth Breast milk S/S of Newborn Severe neurological problems Eye abnormalities Hearing loss Microcephaly Hydrocephaly Enlarged liver Cerebral palsy Herpes Simplex II Transmission: Direct contact at birth S/S of Newborn Custer of vesicles Lethargy Encephalitis Mental delays Seizures Retinal dysplasia Apnea Coma CONTACT ISOLATION - culture vesicles Treatment: Antivial drugs HIV/AIDS Transmission: Transplacentally Exposure at birth Breast milk Diagnosis: Serology tests are performed within 48 hours of birth; repeated at 3 and 6 months HIV antibody ELISA CD4 + T-cell HIV/ AIDS Diagnosis HIV infected (two or more positive tests for HIV) Perinatally exposed (born to a mother know to be infected with HIV) Seroconverter (born to a mother known to be infected with HIV but has had two negative HIV tests HIV / AIDS Nursing Interventions HIV infected mothers should be identified and begin treatment with AZT during pregnancy and in labor All infants born to an infected mother should be treated prophylactically ◦ ◦ 6 weeks of AZT orally after birth Bactrim and Septra Provide care like that of any other newborn Infant of Diabetic Mother IDM Complications of Infants of Diabetic Mothers Hypoglycemia Hypocalcemia Hyperbilirubinemia Polycythemia Respiratory Distress Syndrome Infants of Diabetic Mothers Why are they prone to HYPOGLYCEMIA? High levels of glucose cross the placenta In response, fetus produces high levels of insulin High levels of insulin production continues after cord cut Depletes the infant’s blood glucose Infants of Diabetic Mothers Clinical Manifestations: Large size – Macrosomia; enlarged spleen, heart, liver Tremors Cyanosis Apnea Temperature instability Poor sucking and feeding Hypotonic muscle tone / Lethargy Nursing Interventions Assess blood glucose Intervene if < 45mg/dl: Feed infant Revaluate blood sugar 30-45 minutes pc If no improvement: IV of D10W Newborn of Substance Abuse Mother Infant of Addicted Mother The newborn of an alcoholic or drugdependent mother will also be alcohol or drug dependent. After birth, when an infant’s connection with the maternal blood supply is severed, the neonate suffers withdrawal. Fetal Alcohol Syndrome – FAS Clinical Manifestations Fetal Alcohol Syndrome - FAS Clinical Manifestations: Affected body systems: Jitteriness Abdominal distention Exaggerated rooting and sucking reflexes CNS GI system Long-term psychosocial implications: Feeding difficulties Mental retardation Infants of Addicted Mothers Clinical Manifestations of Infant Withdrawal Central Nervous System o IRRITABILITY • Hyperactivity • Shrill cry • Exaggerated reflexes • Facial scratches • Short non-quiet sleep Sneezing, coughing, yawning Gastroinestional System o Poor feeding o Disorganized vigorous suck o Vomiting and/or Diarrhea Vasomotor and Cutaneous Signs o Tachypnea o Sweating o Excoriated skin Infants of Addicted Mothers Nursing Care Soothing: Protect skin from excoriation Monitor V/S Feeding Swaddle with hands near mouth Offer pacifier Place in quiet dimly lit area of the nursery Provide small frequent feedings Position with HOB elevated Weigh every 8 hours (if vomiting & diarrhea) Assess with Finnegan Abstinence Scale Administer morphine, phenobarbitol, methadone Affects of Smoking on the Fetus during pregnancy Nicotine Causes vasoconstriction Reduces placental blood circulation Carbon Monoxide Inactivates fetal and maternal hemaglobin Reduced amount of oxygen to fetus results in prematurity or low birth weight Thank you! Christina Hernandez RN, MSN chernan1@austincc.edu