mins march 2013
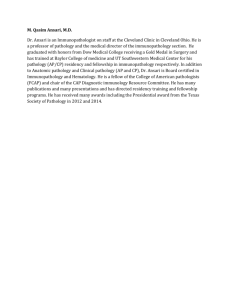
advertisement

Glasgow Obstetrical & Gynaecological Society, 112th session Minutes of the fifth meeting of the Glasgow Obstetrical and Gynaecological Society held in the Royal College of Physicians and Surgeons on 27th March 2013. The President, Dr Kevin Hanretty, was in the chair. Apologies were received from; Drs McGough, McLelland, Willocks, Hepburn, Panigrahy, Gate, Cassidy, Brennand, Kennedy and MacLean. There was one application for membership from Dr Nibedita Ray Gaheer. Dr Hanretty welcomed Professor Massimo Pignatelli, St Mungo-Notman Chair in Pathology and Head of Glasgow Medical School. He also extended a welcome to the Glasgow University Obstetrics & Gynaecology Society members. Prof Pignatelli’s talk was entitled ‘Pathology in the 21st Century’. He described how personalised (precision) medicine is the new face of pathology. Traditional pathology suggested that diseases originated from cells rather than the imbalance of fluids, and was based on the understanding of disease at a cellular level. Since 1894, until recently, morphological observation was the basis for pathology. An example of this basis includes Robin Warren’s discovery of the relationship between Helicobacter and peptic ulceration (Nobel Laureate in medicine 2005). Disease grading and prognosis was based upon various components including tissue architecture, location of nuclei, how cells are organised/structured within tissues. These pathological findings were associated with relevant clinical history. Thus pattern recognition is important. However, it is recognised that morphological evaluation can be subjective and unequivocal diagnosis is not always possible. Clinicians base prognosis and treatment upon pathological stage and grade. This issue has resulted in interest in molecular biomarkers to increase the prognostic and diagnostic abilities. Prof Pignatelli outlined his research interest in identifying new markers using cell communication and adhesion molecular morphology. Potential biomarkers include integrins, cadherins, Ig CAMS and selectins. He cited some examples, including fascin over expression in cancers, as a poor prognostic marker – can molecules inhibit this protein? New translational pathology is based upon discoveries in order to understand and eradicate disease. For example, Herceptin as a ‘blocker’ in breast cancer is ‘personalised’ medicine. The role of pathology in precision medicine involves the customisation of healthcare, targeting drugs for each genetic profile and has key requirements (molecular diagnostics, drug development progression and high quality pathology including good tissue sample history). The role of the pathologist is to provide high quality tissue samples, the evaluation and integration of morphology and interpretation of the results based on clinical context. Pattern recognition is still important; however, can the development of morphological evaluation which is les subjective lead to improved prognosis and treatment? This involves the integration of basic, translational and regulatory science. Prof Pignatelli went on to describe the new South Glasgow Hospital as a £900 million capital project, aimed to complete in 2015. In pathology, there will be different services including an academic block, clinical research facility and a research imaging centre. This will be the largest pathology block in Europe, with over 45 consultants and greater than 100000 tissue samples per year. There will be 30 trainees at one time on a single site. The Glasgow Biorepository at the SGH will aim to streamline the process of tissue acquisition and distribution, funded by a CSO grant. The samples will include tissue, blood, urine, and cytological preparations in both diseased and healthy cases. New legislation orders that tissues containing intact cells may only be stored in an accredited biorepository. Currently, there are national and local open collections of surplus human tissue. The Scottish Standards of Tissue Banking ensure that legal and ethical principles are complied with. Prof Pignatelli highlighted his research with Cancer Research UK, involving pathology, oncology and the biobank. The vision is to establish a national molecular diagnostic service leading to high quality cost effective tests for patients. There will be 7 clinical hubs (SHG is one), and Phase one is underway this year. The aims for phase one are to develop the NHS genetic lab and research infrastructure. There have been 1340 cases over 2 years with a range of tumours. Phase 2 will involve fewer tumour types but increased volume. Lessons from phase one will direct phase 2 and are likely to focus on lung cancer more specifically. Prof Pignatelli answered questions from the audience, and the vote of thanks was given by Dr Pringle. The next meeting will be on 17th April – visiting meeting, Larbert Hospital. Please remind your juniors to attend! ……………………………………………………… President.