Cellulitis Pathway - Swansea Acute GP Services homepage
advertisement

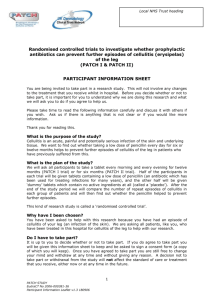
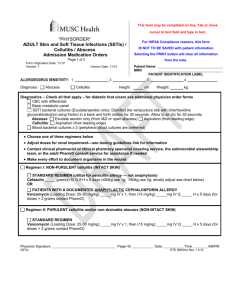
Singleton Minor Injuries Unit Typical Class II Cellulitis Pathway-Out Patient Ambulatory Treatment (OPAT) February 2010-Dr Chris Johns (07967806603) Background Many patients are often admitted to hospital unnecessarily for Intravenous antibiotics for Class II Cellulitis. Cellulitis in adults is a common medical condition taking up a large number of occupied bed days in Acute hospitals. In 1985 in the UK, skin and subcutaneous tissue infections resulted in 29,820 hospital admissions and a mean occupancy of 664 hospital beds each day 1. One survey concluded that it accounted for around 3% of emergency medical consultations at a UK district general hospital. The classification system Eron LJ (2000) devised this classification system of skin and soft tissue infections to aid the GP/Nurse diagnosis, treatment and admission decisions. Class I patients have no signs of systemic toxicity, have no uncontrolled co-morbidities and can usually be managed with oral antimicrobials. Class II patients are either systemically ill or systemically well but with a co-morbidity such as peripheral vascular disease, chronic venous insufficiency or morbid obesity which may complicate or delay resolution of their infection. Class III patients may have a significant systemic upset such as acute confusion, tachycardia, tachypnoea and hypotension or may have unstable co-morbidities that may interfere with a response to therapy or have a limb threatening infection due to vascular compromise. Class IV patients have sepsis syndrome or severe life threatening infection such as necrotizing fasciitis. Clinical findings alone are usually adequate for diagnosing cellulitis, particularly in non-toxic immunocompetent patients. In the past, it has been standard practice to hospitalize Class II patients with serious soft tissue infections, such as cellulitis. However, those of Class II severity can usually be treated safely and effectively with OPAT followed by transition to oral agents as the infection resolves. Ceftriaxone has been listed for the management of Class II infections. This agent is administered once daily making it a suitable agent if OPAT is locally available and considered appropriate. Its safety and efficacy in this situation is well established. It is relatively cheap ABMU Health Board presently buying a 2g vial of Ceftriaxone at £1.63p There are community pathways available that have been developed but there have been workload implications for already stretched community services and problems with patients needing to re-attend secondary care for cannulae care. In addition community medical assessment and review is not always possible. Singleton Minor Injuries Unit is ideal to deliver OPAT. Patients can be referred from Accident and Emergency and other secondary care specialities. Singleton MIU can provide daily iv antibiotics, cannula care, ongoing assessment and conversion to oral antibiotics when appropriate. Exclusion Criteria If the patient has any criteria listed below they are not suitable for outpatient IV treatment of cellulitis. 1. Hypersensitive (allergic) to Penicillin or Cephalosporins 2. Pregnant/lactating women [subject to clinical review] 3. Hepatic and/or renal disease 4. Neutropenia 5. Concurrent, uncontrolled illness 6. Inability to manage at home due to present circumstances - e.g.: Support services/Carer : Effects of condition 7. Likelihood of non-compliance 8. Facial/Orbital cellulitis 9. Class 3 & 4 Cellulitis 10. Known colonisation with Ceftriaxone resistant organism e.g. MRSA (discuss with Microbiology) 11. Age 16 or under Referrals Referrals are accepted by Singleton Minor Injuries for ambulatory management of Class II cellulitis by telephone on 0179 2281582 and patient details faxed to 01792 298347. Referrals can be accepted after diagnosis from the secondary care team. In most cases it is anticipated the first dose of iv antibiotics would be administered by the secondary care team at Morriston or Singleton Hospital. Specialities with access to pathway Morriston A+E Burns and Plastics Morriston Singleton MIU General Medicine Morriston and Singleton Morriston Trauma and Orthopaedics General Surgery Morriston and Singleton Singleton Dermatology DVT pathway The DVT pathway in MIU has been running for 6 weeks. Patients are being seen and treated very quickly and initial figures a good pick up rate with reference to positive scans. Some DVT patients will suffer secondary problems with post thrombotic syndrome and a cellulitis pathway facets in well with the DVT service Clinical issues (http://www.crestni.org.uk/cellulitis-guide.pdf) Cellulitis presents as the acute and progressive onset of a red, painful, hot, swollen and tender area of skin. The edge of the erythema may be well demarcated or more diffuse and typically spreads rapidly. Constitutional upset with fever and malaise occurs in most cases, and may be present before the localising signs. Blistering/bullae, superficial haemorrhage into blisters, dermal necrosis, lymphangitis and lymphadenopathy may occur . The leg is the commonest site and there may be an identifiable portal of entry, for example, a wound, an ulcer or signs of tinea infection. Bilateral leg cellulitis is extremely rare. The use of simple clinical diagnostic criteria should be encouraged and should avoid over diagnosis and inappropriate investigations and antibiotics . The absence of typical clinical features should make one think of the main differential diagnoses, especially: 1.Varicose eczema which is often bilateral with crusting, scaling and itch or other lower leg eczema. 2. DVT with pain and swelling without significant erythema. 3. Acute liposclerosis which may have pain, redness and swelling in the absence of significant systemic upset . Other differential diagnosis include lower leg oedema with secondary blistering, erythema nodosum, other panniculities or vasculitis and pyoderma gangrenosum. Complications include fasciitis, myositis, subcutaneous abscesses, septicaemia, post streptococcal nephritis and death.iianan II2 Investigations Although non-specific, nearly all patients have a raised white cell count and elevated ESR or C-reactive protein. Normal results make a diagnosis of cellulitis less likely. Culture of any local lesion is generally unrewarding – intradermal needle aspiration yielding positive culture results in around 10% of cases and punch biopsy in 20% 6. However where there is an open wound, drainage or an obvious portal for microbial entry, a swab should be taken for culture. Blood cultures are rarely positive (2-4%) and contaminants may outnumber pathogens . Blood cultures should not be undertaken routinely but be reserved for patients where the infection has been graded as Class III or Class IV where they are more likely to yield the causative organism. Serological tests such as ASOT or AntiDNAse B only provide retrospective evidence in selected refractory cases. Class II Cellulitis should be investigated with FBC, ESR/CRP, U+E and Culture of any skin break, serous leak or blister fluid. In this Class there is no evidence that Blood Cultures, Streptococcal Serology or Skin Biopsy is helpful Suitable Treatment Regimes for Typical Class II Cellulitis Flucloxacillin 2g iv qds or Ceftriaxone 1g iv od (OPAT) (no history of Penicillin allergy/anaphylaxis) Penicillin allergy: It is essential to obtain a detailed history of a patient’s reaction to penicillin as this may allow a clinician to exclude allergy. The vast majority of patients with a history of penicillin rash tolerate cephalosporins without significant reaction . If the patient has experienced an anaphylactic reaction or immediate urticarial rash to a penicillin, this class of drug must be avoided. Macrolide antibiotics or clindamycin are suitable alternatives. ( Clarithromycin 500mg iv bd or Clindamycin 600mg iv bd) In the past, it has been standard practice to hospitalize Class II patients with serious soft tissue infections, such as cellulitis. However, those of Class II severity can be treated safely and effectively with OPAT followed by transition to oral agents as the infection resolves. Ceftriaxone has been listed for the management of Class II infections. This agent is administered once daily making it a suitable agent if OPAT is locally available and considered appropriate. Its safety and efficacy in this situation is well established. Although criteria for the switch from parenteral to oral antibiotics for patients with community acquired pneumonia have been studied there is less information in relation to cellulitis. It has been suggested that patients can be switched safely to oral antibiotics within 3.5 days of therapy for uncomplicated cellulitis . Use of IV therapy for longer than 3-4 days in these uncomplicated cases does not correlate with better outcomes. Criteria for change to oral therapy • • • Pyrexia settling Co-morbidities stable Less intense erythema Falling inflammatory markers Suitable oral regimes • Flucloxacillin 500mg qds for 14 days • • Clarithromycin 500mg bd (Penicillin allergy) for 14 days Clindamycin 300mg qds (Penicillin allergy) for 14 days Minor Injury Unit Pathway Proposal Singleton Minor Injuries Unit is an ideal clinical environment for the delivery of OPAT for Class II cellulitis. Patients can be referred by secondary care after initiation of management. Benefits • • • • • • • • • • • Avoids unnecessary admission to hospital Transfers work from stretched Morriston A+E Close contact with other specialities-Podiatry, Dermatology, Vascular etc. Avoids Community problems with overstretched District Nursing and cannula care Quality of service for patients-waits etc Maximise MIU time when not functioning as Out of Hours Service. Joint working between GP’s and Hospital Ambulatory Care Model-future for Singleton Hospital Closer contact with Primary Care on discharge Enhance the position of MIU Test the water for future service provision?-direct GP referral? Timescales If the proposal is accepted the pathway could start 1st Sept 2010 which would allow 6 months of the DVT pathway to run and to develop the pathway further. Patient Numbers It is almost impossible to establish accurately the likely numbers of referrals as the exclusion criteria and multiple referral routes from specialities make measurements difficult. Morriston A+E are looking at likely referral numbers. It may be that the pathway will begin without an accurate forecast and will have to react to referral numbers and patterns accordingly. Resource Implications There may be need, particularly given the workload implications of the DVT pathway, the need to look at Nursing rota adjustments as two nurses during the day would be ideal to cover both the DVT pathway and the Cellulitis pathway in addition to “walk in” minor injuries. As the work in predictable the pathway will run 7 days a week 9am until 6pm, alongside the DVT pathway. It is unlikely there would be any medical staff resource issue as this work can be absorbed in present structures. Additional information http://www.crestni.org.uk/cellulitis-guide.pdf http://www.prodigy.nhs.uk http://www.cks.nhs.uk/clinical_knowledge/clinical_topics/previous_version/cellulitis.pdf Algorithm See below Algorithm for OPAT of Typical Class II CellulitisSingleton Minor Injuries Unit Patients presents to Morriston A+E (or other secondary care speciality) with Class II Cellulitis and suitable for OPAT. Patient assessed, investigated, observations recored, iv cannula sited, erythema marked. First dose of iv antibiotics given. Patient is referred by telephone/fax to MIU and appointment time given for next day Patient attends MIUdaily for iv antibiotics (Ceftriaxone iv), further assessment and cannula care No Clinical improvement or deteriorating signs and symptoms at any time Patient referred to appropriate secondary care team for further management or admissionMedical, Surgical, Dermatology or Microbiology Clinical improvement after 4 days iv antibiotics (Ceftriaxone 1g) Converted to oral antibiotics. Flucloxacillin 500mg qid for 14 days Patient discharge to GP with recommendations for follow up in 7 days and need for Outpatient referralDermatology, Surgical, Lymphoedema or antibiotic prophylaxis if 2 or more episodes at same site