Decontamination of Reusable Medical Devices Policy
advertisement

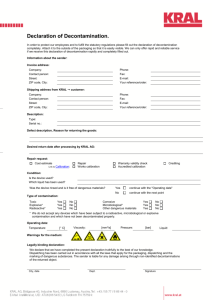
DECONTAMINATION OF REUSABLE MEDICAL DEVICES TRUST POLICY Version 3 Name of responsible (ratifying) committee Decontamination Committee Date ratified 28 January 2015 Document Manager (job title) HSDU Manager / Decontamination Lead Date issued 03 February 2015 Review date 01 February 2017 Electronic location Infection Control Policies Related Procedural Documents Hand Hygiene, Standard Precautions Key Words (to aid with searching) Decontamination of medical devices, cleaning, sterilisation, disinfection Version Tracking Version Date Ratified Brief Summary of Changes Author 3 28 January 15 Minor revision and review IPCT Decontamination of Reusable Medical Devices Policy Version: 3 Issue Date: 03 February 2015 Review date: 01 February 2017 (unless requirements change) Page 1 of 22 CONTENTS 1. Introduction 2. Purpose 3. Scope 4. Definitions 5. Duties and responsibilities 6. Process - Risk Assessment and Choice of decontamination methods - Compatibility - Regulatory framework for medical device decontamination - Decontamination Committee and the Management of Decontamination Services - Decontamination of invasive medical devices - Decontamination of non-invasive medical devices - Decontamination of Endoscopes - Record Keeping - Devices suspected of contamination with prions - Single Use medical devices - Decontamination of Equipment Prior to Service or Repair - Loan/Lease devices 7. Training Requirements 8. References and associated documentation 9. Equality Impact Statement 10. Monitoring compliance with procedural documents 11. Appendix A: Approved list of cleaning agents 12. Appendix B: Example of a Decontamination Certificate 13. Appendix C: Decontamination Committee Terms of Reference 14. Appendix D: Regulatory Framework for Medical Device Decontamination Decontamination of Reusable Medical Devices Policy Version: 3 Issue Date: 03 February 2015 Review date: 01 February 2017 (unless requirements change) Page 2 of 22 QUICK REFERENCE GUIDE This policy must be followed in full when developing or reviewing and amending Trust procedural documents. For quick reference the guide below is a summary of actions required. This does not negate the need for the document author and others involved in the process to be aware of and follow the detail of this policy. The quick reference can take the form of a list or a flow chart, if the latter would more easily explain the key issues within the body of the document 1. Decontamination is a combination of processes (cleaning, disinfection and/or sterilisation) which removes or destroys contamination so that infectious agents cannot reach a susceptible site in sufficient quantities to cause harm to a patient or device user. Differing levels of decontamination are used depending on the device and the procedure involved. 2. The choice of the decontamination method (cleaning, disinfection and/or sterilisation) centres around the infection risk associated with the use of the device, the type of device, the nature of the contamination, the organisms involved, the risk to patients and staff. 3. Medical devices must be checked for compatibility with the proposed decontamination method. 4. Invasive medical devices, such as surgical instruments, must be decontaminated in a compliant environment with validated processes such as the Hospital Sterilisation and Disinfection Unit (HSDU) 5. Non-invasive medical devices must be subjected to a suitable level of decontamination based on the use and type of device involved. 6. The decontamination of flexible endoscopes is to include cleaning and disinfection. These processes must be undertaken in dedicated Endoscope Decontamination Areas within the Trust. 7. If equipment is believed to be contaminated with prions then the equipment should not be decontaminated and should be quarantined. Seek advice from the Consultant Microbiologist, Decontamination Lead or the Infection Control Team 8. The reuse of ‘single-use’ devices has legal implications. It is the policy of the Portsmouth Hospitals NHS Trust that medical devices designated for a single episode of use are not to be reused under any circumstances Decontamination of Reusable Medical Devices Policy Version: 3 Issue Date: 03 February 2015 Review date: 01 February 2017 (unless requirements change) Page 3 of 22 1. INTRODUCTION High standards of cleanliness and hygiene related to equipment and medical devices are essential for the prevention of cross infection in the healthcare environment. The cleanliness of the environment and equipment used in patient care is the responsibility of all staff. The Health and Social Care Act 2008 requires the Trust to ensure that appropriate standards are maintained for the decontamination of equipment and reusable medical devices. This policy provides an explanation of the processes, responsibilities and requirements relating to the decontamination of medical devices. Whilst the advice contained within this policy relates particularly to microbiological hazards, equipment may also become contaminated with hazardous chemicals. The same requirements of decontamination to provide safe equipment apply and should be included in safe systems of work. 2. PURPOSE The purpose of this policy is To provide staff with the necessary information to decontaminate patient equipment safely in order to protect patients, public, members of staff from infection, injury or harm whilst maintaining the integrity and purpose for which each item of equipment was intended To promote the safest possible environment for patients through the identification and application of best practice in the decontamination of re-usable medical devices. To provide compliant guidance to all staff who undertake the decontamination of medical devices within Portsmouth Hospitals NHS Trust. To promote consistency in Decontamination practices across the Trust incorporating essential quality requirements and best practice. The principles of this policy are: That the Trust will continually review and develop practices in order to comply with all present and future medical device legislation within resources available. That equipment will be adequately cleaned, disinfected or sterilised according to its function so as to protect as far as reasonably practical the health, safety and welfare of its staff, patients and those recipients who are involved in inspection, service, repair or transportation of medical devices or equipment. That the Trust will ensure adequate provision of disinfectants, cleaning agents and equipment necessary to achieve the required standard of decontamination. 3. SCOPE This policy applies to direct employees of Portsmouth Hospitals NHS Trust and employees of other organizations managed by the Trust. ‘In the event of an infection outbreak, flu pandemic or major incident, the Trust recognises that it may not be possible to adhere to all aspects of this document. In such circumstances, staff should take advice from their manager and all possible action must be taken to maintain ongoing patient and staff safety’ Decontamination of Reusable Medical Devices Policy Version: 3 Issue Date: 03 February 2015 Review date: 01 February 2017 (unless requirements change) Page 4 of 22 4. DEFINITIONS Decontamination; The decontamination of re-usable medical devices is the combination of processes, which if not correctly undertaken, individually or collectively, may increase the likelihood of microorganisms being transferred to patients or staff. Decontamination is a process, which removes or destroys contamination and thereby prevents microorganisms or other contaminants reaching a susceptible site in sufficient quantities to initiate infection or any other harmful response. Three processes of decontamination are commonly used; - Cleaning - Disinfection - Sterilisation Cleaning; Cleaning is the mechanical process which physically removes soiling but does not necessarily destroy microorganisms. The reduction of microbial contamination is not routinely measured and will depend upon many factors, including the efficiency of the cleaning process and the initial bioburden. Cleaning removes micro-organisms and the organic material on which they thrive. Disinfection; Disinfection is a process intended to kill, reduce or remove, pathogenic micro-organisms but which may not necessarily inactivate some microbial agents, such as certain viruses and bacterial spores. Disinfection may not achieve the same reduction in microbial contamination levels as sterilisation. Sterilisation; Sterilisation is the process of rendering an article completely free from all living microorganisms including viruses. Standard sterilisation methods will not destroy abnormal prion proteins thought to be the causative agents of Creutzfeldt-Jakob disease (CJD). Bioburden; The population of viable infectious agents contaminating a medical device Single-use device; A medical device which is intended to be used on an individual patient during a single procedure and then discarded. It is not intended to be used on another patient. Staff who disregard this information and allow further use of these items, will transfer legal liability for the safe performance of the product from the manufacturer to themselves, or to the Trust HSDU; The Hospital Sterilisation and Disinfection Unit (HSDU) is a centralized department specifically designed and equipped to reprocess reusable medical devices. The department uses a range of decontamination equipment such as ultrasonic washers, washer-disinfectors and sterilisers to achieve medical device decontamination. CJD and vCJD; Creutzfeldt–Jakob disease and variant Creutzfeldt–Jakob disease (vCJD) are degenerative neurological disorders that are incurable and invariably fatal. Brain tissue develops holes and takes on a sponge-like texture. This is due to a type of infectious protein called a prion. Prions are misfolded proteins which replicate by converting their properly folded counterparts. Standard sterilisation methods will not destroy these abnormal prion proteins. Decontamination of Reusable Medical Devices Policy Version: 3 Issue Date: 03 February 2015 Review date: 01 February 2017 (unless requirements change) Page 5 of 22 5. DUTIES AND RESPONSIBILITIES The Chief Executive The Chief Executive is ultimately accountable for ensuring that there are effective arrangements in place for the decontamination of medical devices, including the provision of adequate decontamination facilities. The Chief Executive has authorized the delegation of these responsibilities to the Director of Infection Prevention and Control (DIPC) and the Trust Decontamination Lead. Director of Infection Prevention and Control (DIPC) The Director of Infection Prevention and Control (DIPC) is responsible for overseeing local control of infection policies (including decontamination) and their implementation. The DIPC nominates a Decontamination Lead to be responsible for the implementation of an operational policy for decontamination. The Decontamination Lead The Decontamination Lead reports to board level through the DIPC. The Decontamination Lead is responsible for the effective, and technically compliant, provision of decontamination services. The Decontamination Lead is responsible for the implementation of an operational policy for decontamination. He/she will ensure that the operational policy clearly defines the roles and responsibilities of all personnel who may be involved in the use, installation and maintenance of decontamination equipment. The Decontamination Lead is also responsible for monitoring the implementation of the policy and will form and chair a Decontamination Committee. The Decontamination Committee The Decontamination Committee is chaired by the Decontamination Lead. The Committee’s function is to provide direction to the Clinical Service Centres of the Trust. Representation on this committee includes the operational leads of those departments involved in decontamination of medical devises (i.e. HSDU, Endoscopy, Clinical Engineering). Authorising Engineer (Decontamination) - AE(D) The role of the AE(D) is fully independent of the healthcare facilities’ structure for maintenance, testing and management of the decontamination equipment. The AE(D) is defined as a person designated by Management to provide independent auditing and technical advice on decontamination procedures, washer-disinfectors, sterilisers and sterilisation and to review and witness documentation on validation. The AE(D) is appointed under the authorisation and direction of the Decontamination Lead. The AE(D) must be IHEEM registered and offer impartial advice to the Trust Management on all matters relating to medical device decontamination. Senior Operational Manager (Estates) The Senior Operational Manager is technically, professionally and managerially responsible (and accountable to the Decontamination Lead) for the engineering aspects of decontamination plant and environment. This function includes the management of the maintenance and testing programmes for decontamination machinery and physical environments. The Senior Operational Manager (Estates) has defined Competent Persons (Decontamination) to undertake repairs, maintenance, validation and testing of washers, sterilisers and associated decontamination equipment. Authorised Person (Decontamination) AP(D) An internally appointed person who has undertaken specialist training and possesses technical knowledge relating to the engineering aspects of decontamination. The person will manage the practical implementation of policy and procedure. Decontamination of Reusable Medical Devices Policy Version: 3 Issue Date: 03 February 2015 Review date: 01 February 2017 (unless requirements change) Page 6 of 22 Competent Person(s) Designated by management to carry our maintenance, validation and periodic testing of decontamination plant and equipment. Users The User is defined as the person designated by Management to be responsible for the management of decontamination processes. The User is also responsible for the Operators. Within Portsmouth Hospitals NHS Trust the User includes the HSDU Manager, Endoscopy Manager and Lead Clinical Engineer. The principal responsibilities of the User are as follows: to certify that the decontamination equipment is fit for use; to hold all documentation relating to the decontamination equipment, including the names of other key personnel; to ensure that decontamination equipment is subject to periodic testing and maintenance; to appoint operators where required and ensure that they are adequately trained; to maintain production records; to establish procedures for product release in line with the quality management system; to ensure that procedures for production, quality control and safe working are documented and adhered to in the light of statutory requirements and accepted best practice. The User may seek the advice of the Decontamination Lead, infection control teams, AE(D) or Microbiologist (Decontamination). Operators The Operator is defined as any person with the authority to operate decontamination equipment, including the noting of instrument readings and simple housekeeping duties. Operators have their tasks clearly defined in their job description. Operators have documented training records to demonstrate that they are competent at undertaking their assigned tasks. HSDU The HSDU provides a decontamination service to all operating theatres, wards, outpatients, clinics etc. and some external customers. The principle responsibilities of the HSDU are to; Provide decontamination which will comply with current legislation and guidelines processing surgical instrument sets, supplementary instruments, loan instrument sets, anaesthetic devices and rigid endoscopes. Provide specialist advice on decontamination and sterilisation as appropriate. Report any significant or major decontamination incidents to the Decontamination Lead, liaise with Infection Prevention and Control, and where appropriate Health and Safety. Endoscopy Decontamination Areas These areas are responsible for the safe and effective decontamination of flexible endoscopes to support the clinical activity of endoscopy units. The responsibility of these areas are to undertake endoscope reprocessing in accordance with Department of Health guidance. Infection Prevention and Control Team The IPC Team will provide specialist advice for the decontamination of equipment prior to purchase and during use. General Managers, Heads of Nursing, Department Managers Ensure that this policy and its associated procedures are fully adhered to within their area of responsibility. Employees Employees are expected to co-operate and assist with the implementation of this Policy, and its associated procedures. Decontamination of Reusable Medical Devices Policy Version: 3 Issue Date: 03 February 2015 Review date: 01 February 2017 (unless requirements change) Page 7 of 22 6. PROCESS 6.1 Risk Assessment and choice of decontamination method The choice of the decontamination method centres around the infection risk associated with the use of the device. Table 1 categorises the risk associated with the use of the device and the required level of decontamination for that device. Table 1: Decontamination requirements based on device use and risk Items in close contact with a break in skin or mucous membrane or introduced into a DEFINITION normally sterile body area. Surgical instruments EXAMPLES Syringes and needles HIGH RISK Intrauterine devices Cleaning and disinfection followed by SUITABLE Sterilisation. METHODS Use disposable, single use items where possible Items in contact with mucous membranes or other items contaminated with particularly DEFINITION virulent or readily transmissible organisms or items to be used on highly susceptible people. INTERMEDIATE Respiratory equipment RISK EXAMPLES Endoscopes, vaginal and rectal ultrasound probes SUITABLE Cleaning and disinfection required. Sterilisation METHODS preferred if the device is compatible. Items in contact with normal and intact skin. DEFINITION LOW RISK EXAMPLES SUITABLE METHOD Commodes, infusion pumps, syringe drivers Cleaning using a suitable detergent Other factors which may need to be considered when choosing an appropriate decontamination method will include: o The type of device o The nature of the contamination o The organisms involved o The risk to patients and staff o The heat, pressure, moisture and chemical tolerance of the medical device o The quality and risk associated with the decontamination method o The manufacturers guidance 6.2 Compatibility Personnel responsible for reprocessing reusable medical devices should: o Ensure that the decontamination agents used are compatible with both devices and reprocessing equipment. o Consult the medical device and reprocessing equipment manufacturer/supplier before changing any decontamination process and obtain their written approval for the change in decontamination process. o Decontaminate reusable medical devices in accordance with the instructions provided by the device manufacturer. o Ensure that appropriate decontamination facilities and compatible agents are available before purchasing new devices. Decontamination of Reusable Medical Devices Policy Version: 3 Issue Date: 03 February 2015 Review date: 01 February 2017 (unless requirements change) Page 8 of 22 o 6.3 Follow the instructions for use supplied by the manufacturer of the decontamination agent. Regulatory framework for medical device decontamination When undertaking decontamination activities Portsmouth Hospitals NHS Trust is required to demonstrate compliance with the following legislation: - European Medical Device Directive - Health and Safety at Work Act - Consumer Protection Act - Health and Social Care Act This legislation is supplemented by various regulations that require compliance. For further details refer to Appendix D. The Care Quality Commission (CQC) regulates all providers of healthcare activities in England through the Health and Social Care Act 2008. This includes requirements related to cleanliness, infection control, safety, availability and suitability of equipment. This includes requirements directly relating to the decontamination of medical devices. The Department of Health also provides specific guidance on the Management and Decontamination of Medical Devices in the form of HTM and CFPP documents. Portsmouth Hospitals NHS Trust are required to incorporate this guidance, where practicable. Enforcement and regulation of the legislation and standards falls within the remit of the following regulatory bodies: - Care Quality Commission (CQC) - Medicines and Healthcare products Regulatory Agency (MHRA) - Notified Bodies (i.e. BSI) The Trust will cooperate with these regulatory bodies to ensure compliance with essential requirements and best practice. 6.4 Decontamination Committee and the Management of Decontamination Services A Decontamination Committee is formed to ensure the Trust operates safely with respect to the management and decontamination of reusable medical devices. The committee will act as a management group ensuring that: - decontamination options are assessed to improve patient outcomes - decontamination procedures undertaken within the Trust encompass all statutory and regulatory requirements - benefits, efficiencies and risks are evaluated specifically relating to medical device decontamination - essential quality requirements with regards to medical device decontamination (as detailed in the standards) are attained and a plan is in place to work towards best practice - a risk register is maintained for medical device decontamination - a decontamination policy is defined and continues to be fit for purpose - representatives from each department/specialty undertaking medical device decontamination attend regularly - decontamination processes are monitored and audited regularly to demonstrate compliance The Decontamination Committee consists of the Trust Decontamination Lead (as designated by the DIPC) and representation from Infection Control, HSDU, Endoscopy, Clinical Engineering, Estates Management, Clinical Departments undertaking medical device decontamination and Clinical users. The terms of reference for the committee are defined in Appendix C. Decontamination of Reusable Medical Devices Policy Version: 3 Issue Date: 03 February 2015 Review date: 01 February 2017 (unless requirements change) Page 9 of 22 6.5 Decontamination of invasive medical devices As stated in Table 1 invasive medical devices entering the sterile body cavities or breaking the skin or mucous membranes (such as surgical instruments) require a decontamination process that includes cleaning, disinfection and sterilisation. Figure 1 represents the decontamination cycle that is applied to invasive medical devices. The Decontamination of surgical instruments is undertaken in the HSDU of Portsmouth Hospitals NHS Trust. The processes employed are as follows; o Cleaning: the removal of all organic debris is achieved through the use of water and detergent. A combination of manual cleaning and ultrasonic cleaning is used prior to devices being placed into an automated washer-disinfector. Automated washing is preferred to manual cleaning due to the ability of washer-disinfectors to achieve a reproducible process that can be validated. o Disinfection: is achieved by heat within the thermal disinfection stage of the automated washer-disinfector cycle. o Sterilisation: is achieved using moist heat (steam) vacuum sterilisers. These use a sterilisation stage at 134-137°C or alternatively 121-124°C. For devices that are heat sensitive Gas Plasma (Hydrogen Peroxide) sterilisation is available. The decontamination machinery used in the HSDU is subject to a testing and validation programme in accordance with Department of Health Guidelines (CFPP 01-01), British, European and International Standards. The Decontamination Services undertaken in the HSDU are monitored against the essential requirements of the Medical Device Directive (MDD) and the unit is subject to regular external auditing by a notified body (BSI). The HSDU is required to operate a Quality Management System that meets the standards of the MDD (Portsmouth Hospitals NHS Trust has opted to comply with BS EN ISO 13485). The Quality Management System is a documented system that is applied to all areas of the decontamination cycle. Decontamination of Reusable Medical Devices Policy Version: 3 Issue Date: 03 February 2015 Review date: 01 February 2017 (unless requirements change) Page 10 of 22 The HSDU ensures that its decontamination processes (Cleaning, disinfection and sterilisation) are validated and that the production of instrument packs is subject to internal quality control in a controlled environment. 6.6 Decontamination of non-invasive medical devices Non-invasive medical devices can become contaminated and present a risk of cross infection to patients, users and staff. This category of medical device includes diagnostic and therapeutic equipment such as syringe pumps, feeding pumps, suction pumps, resuscitation equipment, patient monitors, nebulisers etc. The following principles must be applied to these devices; Cleaning of the equipment must be performed immediately following patient use by the user of the equipment Clean the device using disposable detergent wipes or water and detergent with a disposable cloth (see appendix A for approved list of cleaning agents) Following cleaning use an approved disinfectant if the equipment has been used on a patient with a suspected or confirmed infection/colonization (see appendix A for approved list of disinfection agents). Store cleaned equipment separately from used equipment and away from areas where cleaning of devices is being undertaken to reduce the risk of recontamination Check manufacturers instructions for cleaning guidance Use a top down approach to cleaning Wear PPE (gloves and apron) when performing cleaning and disinfection Replace damaged or worn equipment as it may not be possible to clean this equipment effectively Following cleaning/disinfection the device may need to be checked by Clinical Engineering or be returned to the Medical Equipment Library Other types of non-invasive equipment There is a wide range of medical equipment located in the patient environment that may not be traditionally considered as a medical device. This includes items such as drip stands, commodes, bed pans, dressing trolleys, hoists, frames, standing/sitting aids etc. The principles detailed above must also be applied to this type of equipment as they can become contaminated and hence present a risk to patients, users and support staff. In addition to regular cleaning of this equipment by the users an additional deep clean of the items may be necessary and available via the HSDU service of the hospital. The HSDU provides an automated washing and disinfection service for this type of medical equipment. Contact the HSDU for further information on availability and compatibility of the equipment with this type of service. 6.7 Decontamination of Flexible Endoscopes As stated in Table 1 the decontamination of flexible endoscopes is to include cleaning and disinfection. These processes take place in dedicated Endoscope Decontamination Areas within the Trust. Endoscope decontamination is undertaken in compliance with the following standards: CFPP 01-06 BSG Guidelines JAG Guidelines Decontamination of Reusable Medical Devices Policy Version: 3 Issue Date: 03 February 2015 Review date: 01 February 2017 (unless requirements change) Page 11 of 22 6.8 Record keeping All decontamination facilities must have in place a record keeping regime to ensure the decontamination process is documented and medical device reprocessing is recorded. The records must show that the decontamination parameters have been met and the device is rendered safe for reuse. This is particularly important for sterile products whose records must detail process parameters used and achieved during the sterilisation of a device. Validation records for decontamination machinery (washers and sterilisers) must be held by the decontamination facilities. For surgical instruments and endoscopes records must be maintained and retained to enable devices to be traced to an individual patient. 6.9 Devices suspected of contamination with prions Prions are an abnormal protein thought to be the causative agent of Transmissible Spongiform Encephalopathies (TSE) e.g. Creutzfelt-Jacob Disease (CJD). The protein is highly resistant to conventional methods of disinfection and sterilisation. If equipment is believed to be contaminated with prions then the equipment should not be decontaminated and should be quarantined. Seek advice from the Consultant Microbiologist, Decontamination Lead or the Infection Control Team. Please refer to the Trust CJD Policy for further guidance 6.10 Single Use medical devices Single use refers to the medical device that is intended for use on an individual patient during a single procedure and then discarded after use (MDA DB2000:04). Single use devices are not intended to be reprocessed and used on another patient. If a device is reprocessed and it is not fit for its intended purpose, both the re-processor and the professional user may be committing an offence. The reuse of ‘single-use’ devices has legal implications. It is the policy of the Portsmouth Hospitals NHS Trust that medical devices designated for a single episode of use are not to be reused under any circumstances Single use devices will have the following symbol on either the packaging or the device itself; 6.11 Decontamination of Equipment Prior to Service or Repair Anyone who inspects services repairs or transports medical devices and equipment has a right to expect that they have been appropriately treated so as to remove or minimise the risk of infection or other hazards e.g. chemical or radiation. Medical devices should be decontaminated and all devices presented for service or repair must be provided with a decontamination certificate according to the Trusts procedure (see Appendix B). Decontamination of Reusable Medical Devices Policy Version: 3 Issue Date: 03 February 2015 Review date: 01 February 2017 (unless requirements change) Page 12 of 22 6.12 Loan/Lease Equipment Instrumentation or equipment may be loaned/leased to an organisation so that a particular procedure can be performed. The instruments are loaned both from manufacturers and other hospitals and are returned after use. This practice increases the risks associated with the decontamination and reprocessing of such devices because the organisation may not be familiar with them. Decontaminate all loan instrumentation both before and after use in accordance with the manufacturer’s instructions. Where appropriate they should be decontaminated in the HSDU. Ensure that loaned instrumentation is accompanied by relevant reprocessing instructions and a comprehensive list of contents. If these are missing or if you do not have the facilities to follow them (e.g. inappropriate sterilisation time/temperature relationships are quoted) the instruments should not be used. Ensure that adequate time is allowed to carry out effective decontamination both prior to and after use. Ensure that systems are in place to allow instrumentation to be tracked through the decontamination processes and to the patient upon which it is used. Check that indemnity forms have been completed and that responsibilities for the instrumentation have been identified and documented. 6.13 Transport of used medical devices Used non-invasive medical devices such as syringe pumps, feeding pumps, suction pumps, resuscitation equipment, patient monitors, nebulisers, drip stands, commodes, bed pans, dressing trolleys, hoists, frames, standing/sitting aids etc must be decontaminated immediately following patient use by the user of the equipment (in accordance with Section 6.6). If any items are being sent to Clinical Engineering for service, repair of checking then the items must be decontaminated prior to them being sent. The transport of used invasive medical devices must be undertaken to minimize the risk of cross infection during transport. The decontamination of invasive medical devices is to be undertaken in authorized units specifically designed for this purpose (i.e. HSDU, Endoscope Decontamination Areas). The transport of used medical devices to these units is to be undertaken using sealed leak proof containers (approved transport boxes or enclosed trolleys). These containers should carry a biohazard warning label. 7. TRAINING REQUIREMENTS The Trust understands the issues surrounding decontamination including its responsibilities to inform instruct and train employees in the safe effective decontamination practices including the use and disposal of chemical disinfectants. Managers must ensure that staff are aware of current decontamination methods and in the principles of Infection Prevention and Control, and that they have received approved and documented training in those methods and systems. . Designated Users and Operators (see Section 5; Duties and Responsibilities) are required to ensure they have undertaken the appropriate technical training and certified courses to equip them with the skills and knowledge to undertake the task. Guidance from the Decontamination Lead as to the relevant training to be undertaken should be sought. Decontamination of Reusable Medical Devices Policy Version: 3 Issue Date: 03 February 2015 Review date: 01 February 2017 (unless requirements change) Page 13 of 22 8. REFERENCES AND ASSOCIATED DOCUMENTATION CFPP 01-01: Management and decontamination of surgical instruments Health and Social Care Act 2008 ‘Code of Practice on the prevention and control of infection and related guidance’ CFPP 01-06: Decontamination of flexible endoscopes 9. EQUALITY IMPACT STATEMENT Portsmouth Hospitals NHS Trust is committed to ensuring that, as far as is reasonably practicable, the way we provide services to the public and the way we treat our staff reflects their individual needs and does not discriminate against individuals or groups on any grounds. This policy has been assessed accordingly All policies must include this standard equality impact statement. However, when sending for ratification and publication, this must be accompanied by the full equality screening assessment tool. The assessment tool can be found on the Trust Intranet -> Policies -> Policy Documentation Decontamination of Reusable Medical Devices Policy Version: 3 Issue Date: 03 February 2015 Review date: 01 February 2017 (unless requirements change) Page 14 of 22 10. MONITORING COMPLIANCE WITH PROCEDURAL DOCUMENTS This document will be monitored to ensure it is effective and to assurance compliance. Minimum requirement to be monitored Lead Tool Frequency of Report of Compliance Reporting arrangements Lead(s) for acting on Recommendations Decontamination Policy Quarterly Decontamination Committee CSC leads Regular meetings to monitor effectiveness of Policy Decontamination Lead Protocols and procedures defined Decontamination Lead Decontamination audits Annually Decontamination Committee CSC leads Register of activities Decontamination Lead Decontamination audits and risk register Quarterly Decontamination Committee CSC leads Decontamination of Reusable Medical Devices Policy Version: 3 Issue Date: 03 February 2015 Review date: 01 February 2017 (unless requirements change) Page 15 of 22 APPENDIX A: Approved list of cleaning agents; TYPE OF CLEANING CATEGORY APPROVED LIST Equipment Disposable wipe Clinell detergent wipe (yellow packet) Work Surfaces Detergent + Chlorine Actichlor plus General environment Detergent + Chlorine Actichlor plus Approved list of disinfectants; Type of Disinfection Environment Equipment Categories Approved List Comment NaDCC (Chlorine) Haz-tab tablets Haz-tab granules Actichlor Chlorine dioxide Difficil-S Chlorhexidine & Cetrimide Travasept Pharmacy Phenolics Hycolin For use in Mortuary and laboratory. Alcohol 70% IPA Spray, Azo-wipes, Alcowipes Pharmacy only Peracetic acid Aperlan, For use in Endoscopy suite Chlorine dioxide Tristel wipes Nasendoscopes, TOE and invasive probes only Decontamination of Reusable Medical Devices Policy Version: 3 Issue Date: 03 February 2015 Review date: 01 February 2017 (unless requirements change) For use on Blood spillages Page 16 of 22 APPENDIX B: Example of a Decontamination Certificate that must accompany any medical device leaving the hospital site for service, repair or loan purposes. Page 1 Certificate of Decontamination Decontamination of Reusable Medical Devices Policy Version: 3 Issue Date: 03 February 2015 Review date: 01 February 2017 (unless requirements change) Page 17 of 22 APPENDIX B (continued): Page 2: Certificate of Decontamination Decontamination of Reusable Medical Devices Policy Version: 3 Issue Date: 03 February 2015 Review date: 01 February 2017 (unless requirements change) Page 18 of 22 APPENDIX C: Decontamination Committee Terms of Reference Purpose A Decontamination Committee is formed to ensure the Trust operates safely with respect to the management and decontamination of reusable medical devices. The committee will act as a management group ensuring that decontamination procedures undertaken within the Trust encompass all statutory and regulatory requirements and the benefits, efficiencies and risks are evaluated to improve patient outcomes. Functions of the Group To receive and review reports from those responsible for, or involved in, medical device decontamination within the Trust; As a result of the point above, to monitor decontamination issues and update the decontamination risk register; To provide guidance to the Trust on purchases of decontamination equipment; To be responsible for keeping up-to-date with all decontamination regulations, standards and guidance and to disseminate information to members of the group regarding changes in decontamination practice, regulation, standards or guidance; To recommend, review and implement policies or procedures that comply with current decontamination regulations, standards and guidelines; To monitor the Trust’s compliance with the decontamination aspects of Care Quality Commission Outcomes To ensure essential quality requirements with regards to medical device decontamination (as detailed in the standards) are attained and a plan is in place to work towards best practice To maintain and review where necessary the Trust decontamination policy for medical devices and ensure it continues to be fit for purpose To form any sub-groups as necessary to conduct the business of the Group. Chair The Group shall be chaired by the Trust Decontamination Lead. The Lead may temporarily delegate chairmanship to a nominated deputy during times of absence. Membership The membership shall include: The Trust Decontamination Lead; Director of Infection, Prevention & Control (DIPC) or nominated representative Representative of Infection Prevention and Control Clinical Engineering Representative The Estates Engineering Manager (Trust) Senior Operational Manager (Carillion) The Trust’s appointed Authorising Engineer (Decontamination); Those responsible for providing/managing directly or indirectly the decontamination services across the Trust (Users and department representatives) including but not limited to: - HSDU Manager; - Endoscopy manager; - Representation from Operating Theatres; - Representation from wards and departments as applicable; Advice and attendance from other representatives, such as the Trust’s appointed Authorising Engineer (Decontamination), may be required when undertaking specific projects. Decontamination of Reusable Medical Devices Policy Version: 3 Issue Date: 03 February 2015 Review date: 01 February 2017 (unless requirements change) Page 19 of 22 APPENDIX C (continued): Decontamination Committee Terms of Reference Reporting Arrangements The Decontamination Group is responsible to the Trust Infection Prevention & Control Committee and with respect to the Decontamination Risk Register, the Trust Risk Management Group. Minutes of the Group can be made available on the Trust intranet if requested. Decisions made by the Group and policies and procedures which are reviewed and updated shall be put on the agenda of the Trust Infection Prevention & Control Group for final approval. Quorum Attendees must include the Group’s Chair (usually the Decontamination Lead) and at least three other members for the meeting to be quorate. Majority A course of action requires support from the Group chair, the representative of Infection Prevention and Control and more than 50% of group members who attend the meeting. Meeting Frequency The Group shall meet at quarterly intervals. Agenda, Minutes and documentation A package will be prepared and sent to members of the Group a minimum of three business days in advance of a meeting. This package will include the following: - Agenda for the upcoming meeting; - Minutes of the previous meeting; - The decontamination risk register; - Any other documents/information to be considered at the meeting Decontamination of Reusable Medical Devices Policy Version: 3 Issue Date: 03 February 2015 Review date: 01 February 2017 (unless requirements change) Page 20 of 22 APPENDIX D: Regulatory Framework for Medical Device Decontamination Overview of the interaction between the different structures within the English legislative system [Source: Choice Framework for local Policy and Procedures 01-01: Management and decontamination of surgical instruments (medical devices) used in acute care. Part A: the formulation of local policy and choices manual, (May 2012), DH Estates & Facilities Policy Division, Leeds.] Decontamination of Reusable Medical Devices Policy Version: 3 Issue Date: 03 February 2015 Review date: 01 February 2017 (unless requirements change) Page 21 of 22 APPENDIX D (continued): Regulatory Framework for Medical Device Decontamination European Harmonised Standards relevant to decontamination processes and equipment: - BS EN ISO 11737. Sterilisation of medical devices. - BS EN ISO 14937. Sterilisation of health care products. - BS EN ISO 17665. Sterilisation of health care products. Moist heat. - BS EN 285:2006 Sterilisation. Steam sterilisers. - BS EN 13060. Small steam sterilisers. - BS EN ISO 15883 Washer-disinfectors. European Harmonised Standards relevant to decontamination management - BS EN ISO 13485. Medical devices. Quality managements systems. European Harmonised Standards relevant to safety requirements for decontamination equipment - BS EN 61010-2-040. Safety requirements for electrical equipment for particular requirements for sterilisers and washer-disinfectors used to treat medical materials. - BS EN ISO 13849-2. Safety machinery. European Harmonised Standards relevant to medical devices - BS EN 556 Sterilisation of medical devices. - BS EN 1041. Information supplied by the manufacturer of medical devices. - BS EN ISO 17664. Sterilisation of medical devices. Information to be provided by the manufacturer for the processing of re-sterilisable medical devices. - BS EN ISO 14971. Application of risk management to medical devices Decontamination of Reusable Medical Devices Policy Version: 3 Issue Date: 03 February 2015 Review date: 01 February 2017 (unless requirements change) Page 22 of 22