Introduction to Bioethics Case Study
advertisement

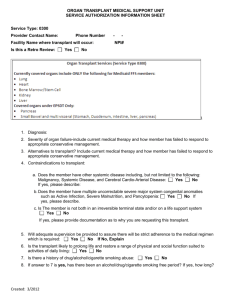
Cases – Introduction to Bioethics (Anita Ho) Case 1 A terminally-ill patient in palliative care was prescribed a morphine infusion for pain management. A few days into therapy, the nurse preparing the infusion discovered that the stock vial being used was incorrectly thought to contain 10mg/10ml, but rather had a concentration of 10mg/ml. She immediately informed the attending physician, and when they returned to the patient, they found out that he had just died. A meeting was then convened involving the hospital president, hospital lawyer, pharmacy staff, the patient’s physician, and the nurse who discovered the error. While the nurse believed that the hospital should reveal the error to the family, others disagreed - they believed that it was in the best interest of both the patient’s family (avoiding further pain) and the hospital not to reveal the error to the family. As the team was still discussing the situation, the patient’s daughter arrived at the hospital. She went to her father’s room and found that he was not there. She asked admission staff members for her father’s whereabouts. Case 2 A 25-year-old man, Smith received two donor hearts when he was a child and then a teenager. Since his second transplant about 10 years ago, his health had been relatively stable, except for reduced kidney function, typical of long-term transplant recipients. Smith's condition began to deteriorate last year -- it was determined to be the result of chronic rejection, the same syndrome that destroyed the first donor heart. The team is considering whether to put Smith on the transplant list once again. Smith's health is in decline; his kidneys are in ‘bad shape,’ leading clinicians to believe that the patient will experience renal failure post transplant, necessitating dialysis temporarily or permanently, as well as consideration for subsequent kidney transplantation. The team believes the patient is at ‘high’ risk of post surgical and three-month recovery period complications. It also observes that the patient’s liver is not functioning adequately as a result of heart failure. The team worries that the waiting period for a donor heart will necessitate other mechanical support that would pose significant risk of stroke. The patient has always been fully engaged in his treatment, following medication regimens as prescribed, and demonstrating faithfulness in clinical appointments. The patient has a loving and supportive family that is ‘keen’ in their support of his efforts to survive. The team has disclosed to the patient their understanding of his health concerns, including all the risks associated with a third transplant. The patient has indicated that despite the risks, he has a strong desire to undergo a third transplant procedure in order to achieve his life plan. However, given that organs are a scarce resource, the team members disagree on whether to place the patient on the transplant list for a third organ.