MS-Word
advertisement

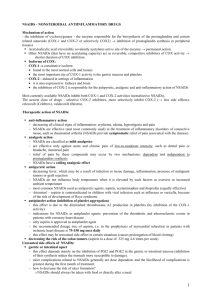
Antiinflammatory Drugs Nonsteroidal Antiinflammatory Drugs (NSAIDs) Aspirin (acetylsalicylic acid) -- only one that is an irreversable inhibitor; less likely to cause interstitial nephritis Ibuprofin (IBU, Motrin, etc..) -- t1/2 is only 2 hrs.; better tolerated than aspirin Fenoprofin (Nalfon) -- longer acting than ibuprofin; t1/2 is about 13 hrs. Ketoprofin (Orudis, Oruvail) -- inhibits both lipoxygenase AND cyclooxygenase Diflunisal (Dolobid) Sulindac (Clinoril) Etodolac (Lodine) Piroxicam (Feldene) -- long-acting Nabumetone (Relafen) -- long-acting Oxaprozin (Daypro) -- long-acting Mefenamic acid (Ponstel) Naproxen (Naprelan, Naprosyn, Anaprox) Indomethacin (Indocin) -- more toxic, but often more effective than the rest sometimes; used to treat patent ductus arteriosus Tolmetin sodium (Tolectin) Phenylbutazone -- weak analgesic and antipyretic, but it is a potent antiinflammatory agent; can cause agranulocytosis and aplastic anemia – treatment is limited to 1 week * Low dose aspirin gives analgesic and antipyretic effects * High dose aspirin is required for antiinflammatory actions * Aspirin is not effective for visceral pain *Low dose aspirin also inhibits platelet aggregation * Antipyretic effect of NSAIDs is due to the inhibition of interleukin-1 and other cytokine release * Death from aspirin OD is due to respiratory and renal failure (requires very high doses) * Aspirin is contraindicated in pregnancy and in children * Aspirin is highly protein bound and displaces methotrexate, phenytoin, probenecid and others Nonopioid analgesics Acetaminophen -- active metabolite of phenacetin; very little antiinflammatory activity; oxidation by cyp-450 pathway releases a reactive metabolite that causes centrilobular hepatic necrosis, unless it’s detoxified by glutathione Phenacetin -- not used any more because of its toxicities * N-Acetylcysteine can be used to treat acetaminophen poisoning if it can be administered w/in 20 hrs of OD. Arthritis drugs (slow-acting) Gold salts -- reduse symptoms and slow progression of rheumatoid arthritis; adverse effects include dermatitis and diarrhea; may even cause aplastic anemia; should follow NSAID treatment Chloroquine -- used if NSAIDs are ineffective, or in conjuction w/ NSAIDs; may cause blindness, but this is very rare; contraindicated in patients with psoriatic arthritis because of the possibility of exfoliative dermatitis D-Penicillamine -- reserved for patients unresponsive to gold or chloroquine; antiinflammatory effects take 3-4 MONTHS to set in; adverse effects are severe and include leukopenia and/or thrombocytopenia that may progress to (guess) aplastic anemia Methotrexate -- can cause a pneumonia-like condition Corticosteroids -- do not alter the progressive destruction of the bone and cartilage Drugs to treat Gout Colchicine -- drug of choice, except for its many adverse effects: vomiting, abdominal pain, alopecia, myopathy, agranulocytosis, and (again) aplastic anemia; usually given IV Indomethacin -- the drug most widely used to treat acute gouty arthritis; limit treatment to 3 days Phenylbutazone -- also limit treatment to 3 days Allopurinol -- a substrate of xanthine oxidase, blocks formation of uric acid from purines; used to treat the primary hyperuricemia of gout; often taken for life, usually well tolerated Probenecid -- block proximal tubule reabsorption of uric acid Sulfinpyrazone -- also blocks uric acid reabsorption * Aspirin is NOT used because in low doses it inhibits the tubular secretion of uric acid (not good) * Probenecid and sulfinpyrazone ALSO block uric acid secretion at low doses; these should not be used in patients excreting high levels of uric acid * Allopurinol may actually precipitate and acute gouty attack; this is prevented by co-administering colchicine during the first few weeks of therapy * Allopurinol also inhibits the metabolism of probenecid and oral anticoagulants Vaccines Bacterial vaccines Pertussis -- from inactive B. pertussis Cholera -- suspension of killed C. vibriae; boosters are needed every 6 months Typhoid -- acetone-killed S. typhi M. tuberculosis -- the BCG vaccine Plague -- suspension of inactivated Pasteurella pestis Rickettsial vaccines Epidemic typhus -- suspension of inactivated R. prowazeki from chicken egg embryos; frequent boosters Rocky Mountain Spotted Fever -- egg grown suspension of R. rickettsii Viral vaccines Influenza -- suspension of egg-grown Influenza virus; only get partial protection Poliomyelitis -- suspension of attenuated live virus types 1, 2, and 3; administered orally Smallpox -- active Vaccina virus; it has been declared eradicated by the WHO Measles -- suspension of attenuated live Rubeola virus Mumps -- suspension of attenuated live strains of the mumps virus Rubella Yellow fever -- suspension of live attenuated virus from chick embryos Rabies -- phenol-inactivated tissue from infected animals, in suspension; adverse effects are resultant of an ineffective vaccination.... paralysis, encephalomyelitis, etc. Passive immunizations Diphtheria toxoid Tetanus toxoid