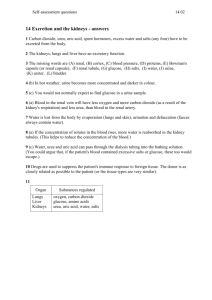
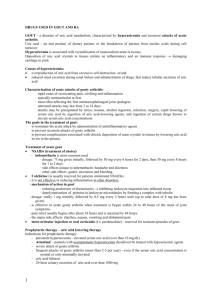
Treatment of acute gout
advertisement

NSAIDS - NONSTEROIDAL ANTIINFLAMMATORY DRUGS Mechanism of action - the inhibition of cyclooxygenase - the enzyme responsible for the biosynthesis of the prostaglandins and certain related autacoids (COX-1 and COX-2 or selectively COX2) inhibition of prostaglandin synthesis in peripheral tissues) Acetylsalicylic acid irreversible covalently acetylates active site of the enzyme → permanent action. Other NSAIDs (that have no acetylating capacity) act as reversible, competitive inhibitors of COX activity → shorter duration of COX inhibition Isoforms of COX: COX-1 -a constitutive isoform found in the most normal cells and tissues the most important site of COX-1 activity is the gastric mucosa and platelets COX-2 - induced in settings of inflammation it is also expressed in kidneys and brain the inhibition of COX-2 is responsible for the antipyretic, analgesic and anti-inflammatory action of NSAIDs Most currently available NSAIDs inhibit both COX-1 and COX-2 activities (nonselective NSAIDs). The newest class of drugs - selective COX-2 inhibitors, more selectively inhibit COX-2 (→ less side effects): celecoxib (Celebrex), valdecoxib (Bextra). Therapeutic action of NSAIDs: anti-inflammatory action decreasing all clinical signs of inflammation: erythema, edema, hyperalgesia and pain NSAIDs are effective (and most commonly used) in the treatment of inflammatory disorders of connective tissue, such as rheumatoid arthritis (NSAIDs provide symptomatic relief of pain associated with the disease) analgesic action NSAIDs are classified as mild analgesics are effective only against acute and chronic pain of low-to-moderate intensity, such as dental pain or headache, menstrual pain relief of pain by these compounds may occur by two mechanisms: dependent and independent to prostaglandins synthesis NSAIDs have a ceiling analgesic effect antipyretic action decreasing fever, which may be a result of infection or tissue damage, inflammation, presence of malignant tumors or graft rejection NSAIDs do not influence body temperature when it is elevated by such factors as exercise or increased ambient temperature most common NSAIDs used as antipyretic agents: aspirin, acetaminophen and ibuprofen (equally effective) Attention! - aspirin is contraindicated in children with viral infection such as influenza or varicella, because of the risk of development of Reye syndrome antiplatelet action (inhibition of platelet aggregation) this effect is due to the diminished thromboxane A2 production in platelets (by inhibition of the COX-1 activity) indications for NSAIDs as antiplatelet agents: prevention of the thrombotic and atherosclerotic events in patients with coronary heart disease only aspirin is approved as antiplatelet agent the recommended dosage size of aspirin, i.e. in the prophylaxis of myocardial infarction in patients with ischemic heart disease is 75-150 mg once daily this effect may be unwanted side effect in certain situations (causes prolongation of blood clotting) decreasing the risk of the colon tumors (aspirin in a dose of 325 mg 4-6 times per week) Unwanted side effects of NSAIDs: gastric or intestinal upset this effect depends mainly on the inhibition of PGI2 and PGE2 in the gastric or intestinal mucosa (inhibition of their synthesis makes the stomach more susceptible to damage). ulcer complications related to NSAIDs generally are dose dependent, and the likelihood of complications is greatest during the first month of treatment. how to decrease the risk of ulcer formation? o NSAIDs should always be taken with food or directly after a meal 1 o administration of drugs that decrease the gastric acid secretion ( receptor H2 inhibitors, proton pump inhibitors) or analogs of natural prostaglandins, such as mizoprostol. o administration of enteric-coated forms of NSAIDs impairment of renal function NSAIDs decrease renal blood flow and the rate of glomerular filtration in patients with congestive heart failure, chronic renal disease or in those who are hypovolemic NSAIDs promote the retention of salt and water by reducing the prostaglandin-related inhibition of reabsorption of chloride and the action of antidiuretic hormone (this may cause edema in some patients and may reduce the effectiveness of antihypertensive treatment) hyperkalemia, which occurs due to increased reabsorption of kalium ions at distal tubules and suppression of prostaglandin-induced secretion of renin low doses of aspirin (1-2 g per day) may decrease urate excretion and increase plasma urates concentrations hypersensitivity reactions (especially bronchoconstriction - due to the diversion of arachidonic acid metabolism toward the formation of increased amounts of leukotrienes, which cause constriction of muscles and have proinflammatory properties → NSAIDs are contraindicated in patients with asthma or other predisposing conditions) NSAIDs may displace certain others drugs from the binding sites (such interactions can occur in patients given NSAIDs together with warfarin - an oral anticoagulant, hypoglycemic agents, methothrexate or digoxin). This interaction can enhance therapeutic or toxic effects of either drugs teratogenic effect - any of the NSAIDs in pregnant women generally is not recommended. Drugs available: Salicylates ACETYLSALICYLIC ACID (Aspirin, Polopiryna) Indications: As antiinflammatory agent - rheumatoid arthritis, juvenile rheumatoid arthritis, degenerative joint disease, inflammation caused by trauma As analgesic agent – mild-to-moderate pain (headache, toothache, menstruation) As antipyretic agent - symptomatic treatment of fever associated with bacterial and viral infections. Attention! It is contraindicated in children with viral infections ! (risk of development of Rey’s syndrome As antiplatelet agent – prophylaxis of arterial thrombosis: ischemic stroke, transient ischemic attack, suspected acute MI, prevention of recurrent myocardial infarction (MI), unstable angina, chronic stable angina revascularization procedures during acute MI Propionic acid derivatives – IBUPROFEN, NAPROXEN, KETOPROFEN, OXAPROZIN Indications: as antiinflammatory agents: rheumatoid arthritis, osteoarthritis, and degenerative joint disease and as analgesic agents: for relief of headache, dental pain, dysmenorrhea and mild to moderate musculoskeletal and postoperative pain. KETOPROFEN - has also been shown to inhibit leukotriene synthesis. It seems to be more irritating to the gastrointestinal tract than aspirin. OXAPROZIN is currently approved for only rheumatoid arthritis and osteoarthritis. Acetic acid derivatives INDOMETHACIN - used as antinflammatory agent in the treatment of some joint disorders ETODOLAC, TOLMETINE - used as analgesics SULINDAC - used as antiinflammatory agents KETOROLAC – used as analgesic, in severe acute postoperative pain Ketorolac seems to be as effective as standard doses of intramuscular morphine or other opioid analgesics, longer acting and with fewer adverse effects. It is available as injectable form. Total course of therapy with ketorolac will not exceed 5 days, because of its high incidence of GI toxicity. Enolic acid derivatives exert potent analgesic and antiinflammatory properties are characterized by long duration of action – administered once daily 2 PIROXICAM MELOXICAM - a slight (10:1) preference for COX-2, which, however, is only clinically relevant at low doses N-Arylanthranilic acids (fenamates) MEFENAMIC ACID ETOFENAMAT – only as topically applied formulations Pyrazolidines PHENYLBUTAZONE – potent antiinflammatory, analgesic, antipyretic properties METAMIZOLE - analgesic and antipyretic a small risk of causing agranulocytosis uniqe spasmolytic effect Paraaminophenol derivatives – ACETAMINOPHEN = Paracetamol – a very weak anti-inflammatory drug, used first of all as an antipyretic and analgesic agent. o lacks certain side effects of NSAIDs, such as gastric ulceration and blockade of platelet aggregation. o mechanism of action: inhibit COX(3) in CNS – antipyretic and analgesic effect o recommended as an effective drug, alternative to aspirin for the treatment of headache and other mild-to-moderate pain; recommended as antipyretic agent, especially in small children with viral infections, when aspirin is contraindicated o metabolized in the liver: small amount is converted into hepatotoxic metabolite. Increased amounts of toxic metabolites are formed: after toxic doses, in chronic alcohol users. GOUT - a disorder of uric acid metabolism, characterized by hyperuricemia and recurrent attacks of acute arthritis. Uric acid - an end product of dietary purines or the breakdown of purines from nucleic acids during cell turnover. Hyperuricemia is associated with crystallization of monosodium urate in tissues. Deposition of uric acid crystals in tissues initiate an inflammatory and an immune response damaging cartilage in joint. Causes of hyperuricemia: overproduction of uric acid from excessive cell destruction or/and reduced renal excretion during renal failure and administration of drugs, that reduce tubular secretion of uric acid Characterization of acute attacks of gouty arthritis: · rapid onset of excruciating pain, swelling and inflammation · typically monoarticular at first · most often affecting the first metatarsophalangeal joint (podagra) · untreated attacks may last from 3 to 14 days · attacks may be precipitated by stress, trauma, alcohol ingestion, infection, surgery, rapid lowering of serum uric acid by ingestion of uric acid-lowering agents, and ingestion of certain drugs known to elevate serum uric acid concentrations. The goals in the treatment of gout: ∙ to terminate the acute attack by administration of antiinflammatory agents ∙ to prevent recurrent attacks of gouty arthritis ∙ to prevent complications associated with chronic deposition of urate crystals in tissues by lowering uric acid levels in the plasma. Treatment of acute gout NSAIDs (treatment of choice) - indomethacin is most common used ∙ dosage: 75 mg given initially, followed by 50 mg every 6 hours for 2 days, then 50 mg every 8 hours for 1 to 2 days. ∙ side effects unique to indomethacin: headache and dizziness ∙ other side effects: gastric ulceration and bleeding, Colchicine (is usually reserved for patients intolerated NSAIDs). - it is not effective in reducing inflammation in other disorders. - mechanism of action in gout: 3 ∙ reducing production of chemotaxins inhibiting leukocyte migration into inflamed tissue ∙ depolymerization of proteins in leukocyte microtubules by forming a complex with tubulin - dosage: orally 1 mg initially, followed by 0,5 mg every 2 hours until (up to total dose of 8 mg has been given) - is effective in acute gouty arthritis when treatment is begun within 24 to 48 hours of the onset of joint symptoms. - pain relief usually begins after about 18 hours and is maximal by 48 hours. - the major side effects: diarrhea, nausea, vomiting and abdominal pain intra-articular injection or oral corticoids (f.e. prednisolone) - reserved for resistant episodes of gout. Prophylactic therapy – uric acid lowering therapy Indications for prophylactic therapy: - persistent hyperuricemia - elevated serum uric acid (over than 10 mg/dL) - Attention! - patients with asymptomatic hyperuricemia should not be treated with hypouricemic agents - severe attack of gouty arthritis - frequent attacks of gouty arthritis (more than 2-3 per year) - even if the serum uric acid concentration is normal or only minimally elevated - uric acid lithiasis - 24-hour urinary excretion of uric acid over than 1000 mg Uricosuric drugs - increase renal excretion of urate - mechanism of action: ∙ increase the renal clearance of uric acid by inhibiting the renal tubular reabsorption of uric acid ∙ increase the concentration of uric acid in urine possible stone formation prophylaxis of renal stones: maintenance of adequate urine flow (by administration of adequate amount of fluids –2.5-3.0 L/day) alkalinization of the urine with sodium bicarbonate solution or potassium citrate - used in patients with normal renal function and no history of nephrolithiasis - indicated in underexcretors (with 24-hour excretion of urate less than 600 mg/day) - available uricosuric drugs: ∙ probenecid and sulfinpyrazone (commonly used in Europe, as well as in the USA) ∙ benzobromarone (available in Europe, but not in the USA) - there may be a temporary increase in uric acid blood levels and increased risk of an acute gouty attack prophylaxis of acute attack: beginning therapy with the administration of small dosages of colchicines Inhibitors of uric acid synthesis (Allopurinol, Febuxostat) - mechanism of action: xanthine oxidase inhibitor block the conversion of hypoxanthine to xanthine and xanthine to uric acid - indications for inhibitors of uric acid sythesis: ∙ drugs of choice in patients with a history of urinary stones or impaired renal function ∙ useful in both patients with increased synthesis (who are overproducers - individuals who excrete more than 600 mg/day on a purine-free diet) and decreased clearance of uric acid ∙ useful in patients with lymphoproliterative or myeloproliferative disorders - the major side effects: ∙ skin rash (hypersensitivity reaction) ∙ bone marrow suppression (leucopenia) ∙ occasional GI toxicity ∙ increased frequency of acute gouty attacks with the initiation of therapy (should be started with small doses of antiinflammatory agents) RHEUMATOID ARTHRITIS (RA) - a chronic, systemic inflammatory disorder involving peripheral joints (an inflammation in the synovial tissue) and extraarticular tissues and organs. The pathogenesis of RA is unknown, probably - an autoimmune disease. The activation of T cells and increased levels of t cell-derived cytokines (IL-1 and TNF-) are present. Signs and symptoms: pain, swelling, warmth, tenderness, stiffness, limitation of motion of joints, general signs weakness, anorexia, weight loss, fever. The major goals of treatment are to reduce pain and discomfort, reduce inflammation 4 prevent deformities and loss of joint function, prevent the disease progression (to the extent possible) maintain a productive and active life. Drug classes used in the treatment of RA: non-steroidal anti-inflammatory agents (NSAIDs), corticosteroids, disease modifying anti-rheumatic drugs (DMARDs) The mechanism of action of many of DMARDs, effective in RA, is uncertain!! NSAIDs - short onset of action, rapidly relieve signs and symptoms, have no effect on the progression of the disease. - Effects: reduce acute inflammation, decrease pain (mild to moderate analgesic properties). - Time required to achieving maximal effect – few hours to 1 month. Corticosteroids - short onset of action, inflammatory and immunoregulatory activity. - Systemic (administered orally) corticosteroids: indicated when there is an increase of inflammation in multiple sites usually given orally in small doses (10 mg of prednisone/or its equivalents/ daily) tapering of corticosteroid should be done slowly (over a few weeks) side effects of prolonged systemic treatment: weight gain cushingoid syndrome osteoporosis (particularly at doses 10 mg of prednisone daily). Prophylaxis: bone densitometry to assess fracture risk, hormone replacement therapy, bisphosphonates. hypothalamic-pituitary-adrenal suppression. Prophylaxis: once a day dosing of prednisone, given before 9 AM. - Intra-articular corticosteroids e.g., triamcinolone - 40 mg in a knee, 20 mg in a shoulder, or 2 mg in a finger for controlling a local inflammation, if only one or two joints are involved. Disease Modifying Anti-Rheumatic Drugs (DMARDs) - agents with delayed onset of action (the appearance of benefit from DMARD therapy is usually delayed for weeks or months) - may alter the disease course and improve long term outcomes. - exert minimal direct nonspecific anti-inflammatory or analgesic effects NSAIDs must be continued during their administration - improve serologic and biochemical evidences of disease activity (f.e. rheumatoid factor, C-reactive protein, the erythrocyte sedimentation rate are decline). - retard the development of bone erosions - indications: symptoms have not improved sufficiently after 3 months of NSAIDs the patient has aggressive seropositive disease there are radiographic evidences (erosions, joint space narrowing or joint destruction) - The currently available drugs include: • leflunomide • soluble interleukin–1 (IL–1) receptor therapy • tumor necrosis factor inhibitors • methotrexate • hydroxychloroquine, sulfasalazine • intramuscular gold • cytotoxic agents (cyclosporine A, azathioprine, and cyclophosphamide) Leflunomide (Arava™) - The mechanism of action: inhibition of tyrosine kinase activity, inhibition of de novo pyrimidine biosynthesis by the inhibition of dihydroorotate dehydrogenase, inhibition of mitogen and IL-2 stimulated T cells. - An alternative drug to patients who have failed or were intolerant to methotrexate. 5 - - In some yearlong study leflunomide was superior to methotrexate in preventing x-ray joint erosions. pharmacokinetic: half-life - 15 days extensively protein bound undergoes enterohepatic recycling. In patients, who must rapidly discontinue therapy (i.e. women wishing to become pregnant): “washing” from the body by cholestyramine (8 g 3 times daily for 11 days) to achieve documented serum concentration of leflunomide less than 0.02 mg/L). Usual time to maximal effect: 4-8 weeks. Side Effects: liver transaminase elevations, mild diarrhea, GI upset, alopecia (hair loss), teratogenic effects Soluble Interleukin–1 (IL–1) Receptor Therapy - IL–1 - has immune and pro–inflammatory properties - the level of disease activity in RA correlates with levels of IL–1. Anakinra (Kineret™) - a human recombinant IL–1 receptor antagonist. - blocks the biologic activity of IL–1 by binding to IL-1R type I. - Dosage: 100 mg/day administered daily by subcutaneous injection (the same time each day). - can be used alone or in combination with DMARDs (other than TNF blocking agents). - Side Effects: injection site reactions decreasing of immunity increased risk of serious infection neutropenia (severe neutropenia is especially high in the combination anakinra/anti-TNF agents anakinra is not used in combination with TNF inhibitors in medical practice). Tumor necrosis factor (TNF) inhibitors TNF- - pro-inflammatory cytokine produced by macrophages and lymphocytes Etanercept (Enbrel™) - human fusion protein - a low potential for immunogenicity - Mechanism: binds TNF- at high affinity in the circulation, preventing interaction with the cell surface TNF- receptors and clears TNF- from the circulation. - reduce the rate of radiographic progression. - Dosing: 25mg given by subcutaneous (SC) injection twice weekly. - Usual time to maximal effect: 1-2 weeks, with some continued improvement over the next 4 weeks. - Side effects: injection site reactions, mild upper respiratory infection symptoms Infliximab (Remicade™) - a chimeric monoclonal antibody - Mechanism: binds TNF– with high affinity and specificity in the circulation. - currently used only in combination with methotrexate - inhibits the progression of structural damage - Dosing: 3 mg/kg given as an intravenous infusion followed with additional 3 mg/kg doses at 2 and 6 weeks after the first infusion, then every 8 weeks thereafter. - Side effects: development of human anti-chimeric antibodies (HACA) which would block infliximab from binding TNF-. "cytokine release syndrome" (fever, chills, headache after the infusion of the antibody) a risk of infections (especially on concomitant immunosuppressive therapy) Methotrexate - early onset of action (4-6 weeks) - high patient tolerability - Indications: - persistent, active disease, with poor prognostic factors (presence of rheumatoid factor, rheumatoid nodules, poor functional status, young age, erosions on x-ray). - Dosage: an initial dosage of 7.5mg orally once weekly. If no effect after 4 to 6 weeks - the dose can be increased up to 25mg weekly (in the elderly or in partial responders) - in patients who experience serious GI side effects - IM injections - contraindications: renal insufficiency, liver disease, alcohol abuse, leukopenia, thrombocytopenia, untreated folate deficiency, obesity, diabetes, hepatitis B or C – increase methotrexate hepatotoxicity. 6 - Usual Time to Maximal Effect: 4 to 6 weeks, with 70% of patients having some response. Side Effects rare: hepatic cirrhosis, interstitial pneumonitis and severe myelosuppression common: stomatitis, mild alopecia and GI upset - are related to folic acid antagonism (prophylaxis: folic acid 1mg daily supplementation). increased risk of localized herpes zoster infection, teratogenic effect (effective birth control is needed). Antimalarials Hydroxychloroquine (Plaquenil, 200mg tablets) and Chloroquine (because of great ocular toxicity is not recommended) - relatively safe, well-tolerated and effective in the treatment of RA (of mild to moderate severity). - Mechanism of action in the treatment of RA is unknown. - usual time to maximal effect: 3 to 6 months - Side Effects: ocular toxicity: corneal deposits, extraocular muscular weakness, loss of accommodation, retinopathy (ophthalmologic examination before and during the period of treatment is needed). Gold (Myochrysine, Solganal – intramuscular, Auranofin - oral gold compound, less effective). - Mechanism in RA is unknown. - Dosage: initially 10 mg intramuscularly, 25mg - given the second week, then 50mg is given weekly until a response has occurred or until a total of 1 g has been given. If there is a favorable response - 50mg every 2 weeks for 3 months, then every 3 weeks for 3 months and then finally to a maintenance monthly dose (continued indefinitely). - Usual Time to Maximal Effect: 4 to 6 months. Side Effects: rash , ulcerations and mucositis of the mouth, tongue, and pharynx , altering renal function (most often - mild proteinuria, rarely - nephrotic syndrom), immune thrombocytopenia, granulocytopenia, and aplastic anemia Immunosuppressive and other cytotoxic agents azathioprine (Imuran) - a purine analog cyclophosphamide (Cytoxan) - an alkylating agent cyclosporin A - an immunosuppressive agent - used in aggressive disease or extra-articular manifestations - serious toxicity’s including bone marrow suppression, infection, secondary malignancy, renal insufficiency. MUSCLE RELAXANTS - used to manage the pathological muscle spasms, associated with: - CNS diseases (cerebral palsy, multiple sclerosis, stroke) Benzodiazepines - Temazepam facilitate the action of GABA in the CNS (mainly in the spinal cord) Baclofen - acts as GABA agonist at GABA-B receptors - produces hyperpolaryzation in the cord and brain with the resultant presynaptic inhibition of impulses - can also reduce pain in patients with spasticity (by inhibition of release of substance P in the spinal cord) Tizanidine - α2 adrenoceptor agonist - inhibits nociceptive transmission in the spinal cord Dantrolene - mechanism of spasmotytic action outside the CNS - decreases the release of Ca ions from sarcoplasmatic reticulum in skeletal muscle - used in the treatment of malignant hyperthermia caused by general anesthesia or neuromuscular blocking drugs 7